Acetabular Protrusion
What is an Acetabular Protrusion?
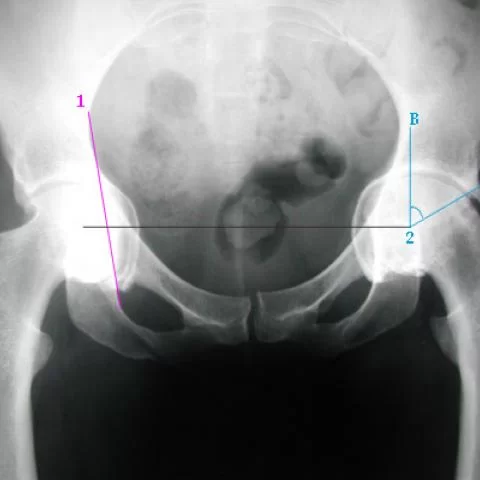
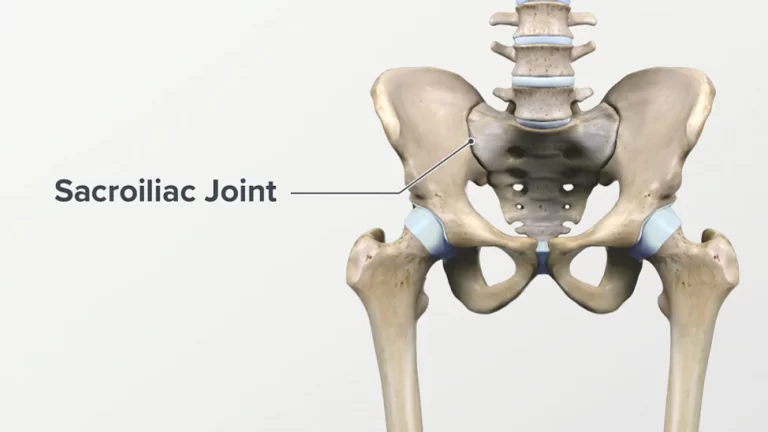
Acetabular overcoverage, also known as protrusion acetabuli or acetabular protrusion, is a hip-joint problem. It is defined by the abnormal extension or protrusion of the hip joint’s cup-shaped acetabulum into the pelvic cavity.
Ilium, ischium, and pubis, the three (3) bones that make composed the hip bone of the pelvic bone or girdle, make up the hip bone. The femoral head is medially relegated in protrusion asymmetry because the medial portion of the femoral cortex is medial to the ilioischial line. The very deep socket could extend into the pelvis.
Cause of Acetabular Protrusion
Developmental factors: Acetabular protrusion may result from incorrect hip joint development during the pregnancy or it may be congenital, meaning it is present at birth.
Acquired causes: Over time, disorders including osteoarthritis, rheumatoid arthritis, or other inflammatory joint problems can affect the structure of the hip joint.
Sign and Symptom
Protrusion acetabular may be asymptomatic. The first indicator is discomfort and a limitation in joint range of motion (ROM).
Classification
Protrusio acetabuli is different into two types, 1. primary and 2. secondary.
leading protrusion In middle-aged women, the acetabuli protrudes more and more, and this condition may be related to osteoarthritis. They could be related.
Depending on the reason, which may include a femoral head prosthesis, cup arthroplasty, septic arthritis, a central fracture dislocation, or total hip replacement (THR) surgery, one may classify secondary protrusion acetabuli as unilateral or bilateral. One may also consider unilateral or bilateral protrusion acetabuli.
Trauma, fibrous dysplasia, and tuberculous arthritis can all induce unilateral protrusion of the acetabulum. Rheumatoid arthritis, Paget’s disease, osteomalacia, Marfan syndrome, and ankylosing spondylitis are a few conditions that can lead to bilateral protrusion of the acetabulum.
Treatment of Acetabular Protrusion
The severity of the symptoms and joint damage determines the course of treatment for acetabular protrusion. Initially, conservative treatment techniques such as rest, physical therapy, painkillers, and activity reduction may be used.
Surgery may be required in cases of greater severity. Surgical options can include:
Hip arthroscopy:
a minimally invasive treatment to relieve impingement and remove any damaged tissue.
Periacetabular osteotomy (PAO): A surgical treatment to realign the hip joint by repositioning the acetabulum.
Total hip replacement: A total hip replacement may be the best choice to treat pain and restore hip function in severe cases of osteoarthritis and joint degeneration.
Post-operative Physiotherapy Treatment
physiotherapy protocols vary in weight-bearing, range of motion, bracing, strengthening, and return to sport guidances. The use of a personalized, criteria-based progression through the stages of rehabilitation is supported by evidence, such as physiotherapy guidelines backed by two-year outcomes. Patient-reported outcomes for the biopsychosocial domain should be included in outcome measurements.
General principles include:
- Pain management
- Swelling management
- Regain normal joint range of motion.
- Progress weight-bearing status.
- Gait training.
- To regain full lower limb muscle power, engage in strength training.
- Proprioception, balance, and coordination training.
- Sport-specific training to return to previous activities
Phase 1: Immediate rehabilitation (1-3 weeks)
Short crank stationary bike: no resistance
Quad sets
Gluteus sets
Transverse Abdominus isometrics with diaphragmatic breathing
Prone lying
Prone glute squeeze with knee flexion
Supine heel slides
Quad rocking
Hooklying pelvic clock
Hooklying with bent knee fallouts
Hooklying marching
Hooklying with hip abduction and adduction, isometric
Passive circumduction
Passive Internal Rotation log rolling
Hip joint mobilizations Grad I, II caudal glides
Soft tissue mobilization- Lumber Spine, glutes, Hamstring, quad, hip flexor, adductors
On the first postoperative day after surgery, postoperative care was started right away. The first phase lasts three weeks. Phase 1’s objectives are to reduce discomfort, protect the tissues that have been healed, stop muscular inhibition, and stop the development of anterior hip contractures.
Crutches and the postoperative brace were used for two weeks after surgery. The patient advanced to weight bearing as tolerated after two weeks. Although muscle weakness is predicted during this period, a successful transition to full weight-bearing is made possible by a modest stimulation of the quadriceps and gluteus muscles. During this stage, isometric exercises are continued, and passive range of motion (PROM), including circumduction, should be done within bounds.
The following PROM limitations apply to weeks 1 through 3:
- Flexion 90°
- Extension 0°
- Abduction 25° to 30°
- Internal rotation (IR) at 90° of hip flexion 0°
- Internal Rotation(IR) is prone to limited comfort
- External rotation (ER) at 90° of hip flexion 30°
- External rotation (ER) in a prone position at 20°
Progress in Range of motion is allowed within a pain-free range after three weeks. The patients must reach full, pain-free weight bearing before moving on to phase II.
The objectives of Phase 2 are to maintain protection of the repaired tissue, restore full hip range of motion and normal gait patterns, and strengthen the hip, pelvis, and lower extremities with a focus on the gluteus medius. Phase 2 lasts from week 4 to week 8 and has these objectives. Strengthening exercises such as the leg press, double-leg squats followed by single-leg squats, and step-ups and step-downs progress from partially to fully weight-bearing postures.
Standing on one leg while rotating the trunk against resistance from an elastic band and standing with the shoulder extended while facing resistance from the band both serve to address core stability and strength. Patients advance to tri-planar stepping, and activities involving double-, followed by single-leg stances, are used to progress patients’ balance. For cardiovascular endurance, elliptical trainer activity can be started between 6 and 8 weeks after surgery and last up to 10 minutes.
Active hip range of motion (AROM) in all planes that are complete and pain-free
a normalized gait without pain
Four out of five on a manual muscle test for hip flexor strength.
Manual muscle testing revealed hip abduction, adduction, extension, and internal/external rotation strength of 4 (of 5).
Phase 3: Advanced rehabilitation (9-12 weeks)
4-point alternate arm and leg extension
Lunges all directions
The lateral elastic band walk
Monster walks with an elastic band
Single-leg squat on an unstable surface
Front and side plank progression
Single-leg stance with rotation against band resistance
Phase 3’s objectives include developing balance, proprioception, and cardiovascular endurance as well as restoring hip flexor muscle strength to 4 and 4+ (of 5) for all other hip motions. Avoiding contact sports, vigorously strengthening the hip flexors, and forcing or aggressively painful stretching are all precautions. Possessing hip flexor muscle strength of 4+ and 5 (of 5) in all other lower extremity musculature is a requirement for progression to sport-specific training.
Phase 4: Sport-specific training (>12 weeks)
Return to run protocol Progress in jogging (began in week 12 at stage 1)
Phase 4 of treatment allows the athlete to start a jogging progression program as well as jumping and agility drills that are tailored to their sport and/or job-related duties. Full hip range of motion in all planes and cardiovascular endurance appropriate for the demands of sport and/or work must be shown before return to play (RTP) is taken into consideration. To pass the RTP exam, you must have average core and lower-extremity strength and flexibility. RTP testing analyses biomechanical performance using slow-motion video.
During the Y-balance test, the athletes must compare their anterior reach within 4 cm and their posteromedial and posterolateral reach within 6 cm from limb to limb. A single hop for distance, a triple hop for distance, and a triple crossover hop for distance must all be executed by the competitor with at least 90% limb symmetry. In the second stage of the RTP test, a single-leg squat off of an 18-inch box is followed by a video examination of a double-leg squat. The athlete must not show any lateral hip or lower extremity deviation from the working side while performing the double-leg squat.
The ipsilateral patella does not cross the plane of the great toe at the whole depth of the squat, and there must be no indication of hip internal rotation or valgus to pass the single-leg squat test. A depth jump from an 18-inch box, landing in a squat, and then jumping straight up in one fluid motion, concluding in a squat posture and 15-foot lateral cone shuffles, make up the last portion of the RTP test. When passing, one must demonstrate strong control throughout cone shuffles without hip internal rotation or valgus on the plant leg, as well as appropriate hip and knee alignment at takeoff and landing.
Rang of motion and mobility
After hip arthroscopy, early range of motion (ROM) is often recommended. Preventing postoperative joint stiffness and probable intraarticular adhesions are the immediate objectives. Early postoperative recommendations frequently include pendulum or circumduction ROM exercises to lower the likelihood of intra-articular adhesion formation. A rehabilitation program that includes several daily circumduction exercises greatly lowers the rate of revision arthroscopy.
ROM is often carried out in a pain-free environment. Repetitive ROM in the sagittal plane is frequently performed on a stationary bike. Although they are not always advised, continuous passive range of motion (CPM) machines may be prescribed post-operatively for sagittal plane ROM. An activity that involves quadruped rocking can help with early flexion.
The patient can manage the range of motion while partially loading the joint by achieving flexion in this way.
The parameters and timeframes for ROM advancement differ between protocols and depending on the particular surgical procedures carried out.ROM measures may be used during procedures to treat capsular laxity to safeguard the afflicted tissue. When operations on the anterior capsule and iliofemoral ligament are done, external rotation and extension are temporarily restricted.
In cases where the posterior capsule was surgically treated, flexion and internal rotation are restricted. Although the indications and duration of usage of a postoperative ROM brace are not widely agreed upon, it is frequently used.
When postoperative stress across the joint capsule is a problem, this brace can be adjusted to different degrees of extension and flexion.
Weight-bearing consideration
Depending on the surgery, there may be different weight-bearing precautions. There is often only a brief time of partial weight bearing, frequently two weeks or less, in minimally invasive instances like isolated labral debridement. If the bone (osteoplasty) or cartilage (microfracture) has been treated, the protected weight-bearing stage may be extended. A prolonged time of protected weight bearing may also be needed for extensive acetabular labrum repairs. The partial weight bearing may be continued for up to six weeks in these more complicated instances. Patients are often not advised to adopt a non-weight-bearing gait pattern unless the surgical technique calls for extensive preservation of the damaged osseous or chondral structures.
Due to the hip flexors being activated, keeping the affected leg in a non-weight-bearing position increases the compressive stresses across the hip joint. The preferred assistive device is often a pair of axillary crutches. Even with slight swelling and pain following surgery, there may be significant reflex inhibition of the gluteus medius, which can impair muscle function and cause compensatory movement patterns such as the failure to keep the pelvis stable in the frontal plane while walking. Clinically, a contralateral pelvic drop is evident in patients with severe gluteus medius weakness or inhibition when the unaffected limb loses support during the swing phase and the patient assumes a single-leg standing position on the affected lower extremity.
Crutches are frequently advised to patients to stop this pelvic drop and enable them to walk with more normalized muscle activation and gait pattern. Allowing patients to walk using compensatory patterns could result in persistent intra-articular discomfort and/or overuse of the hip’s accessory muscles, which could slow the healing process. Even if this persists over the durations specified in post-operative guidelines, it is advised that patients stay on crutches until they can ambulate without any deviations.
Muscular strengthening exercise
The postoperative strengthening exercises that are advised by protocols and/or clinicians differ greatly. The patient’s range of motion (ROM) and weight-bearing tolerance should be taken into account when choosing interventions to ensure that there is sufficient range of motion and neuromuscular control to complete exercises without reinforcing inappropriate patterns or escalating discomfort and inflammation. Exercises that specifically stress the iliopsoas or iliotibial band (ITB) may be postponed to allow for tissue recovery in circumstances where these structures have been released or extended.
To prevent muscle atrophy, submaximal isometric exercises at the thigh, pelvis, and trunk should be recommended first. It is advised to concentrate on the multifidus muscle, which runs the entire length of the spinal column but is most developed in the lumbar region, and the traverses abdominus. for lumbar spine stability with transfers. The local core stabilizer multifidus muscle is important for both static and dynamic spinal stability. It is advised to conduct gluteal, quad, and iliopsoas isometrics while lying on your back to encourage a neutral hip position and reduce anterior soft tissue stiffness.
As the patient improves, greater attention is put on strengthening the gluteal muscles, particularly the gluteus medius and hip abductors because of their importance in maintaining the pelvis’ frontal plane stability during functional tasks like gait. Although there is little literature describing muscle activation patterns during particular workouts in the healthy population, research on muscle functioning patterns in the population with non-arthritic hip pain is available.
With a future goal of using information regarding the diseased and postoperative population, as it becomes accessible, protocols should be created taking this knowledge into account. demonstrates how the external rotator strengthening has progressed. The person starts with an external rotation utilizing a stool that is partially loaded and band-resisted.
The patient can begin resistive hip external rotator strengthening in a full-weight-bearing position after they can maintain stability in the frontal plane (adequate hip abductor strength).
Prognosis
Before the femoral neck presses against the pelvis, the protrusion may continue to advance
FAQs
What is acetabular protrusion?
The intrapelvic expatriation of the acetabulum and femoral head, also known as protrusion acetabuli, is what causes the femoral head systems to be medial to the ilioischial line. It should be treated differently from coxa profunda.
What causes acetabular protrusion?
Trauma, fibrous dysplasia, and tuberculous arthritis are three conditions that can cause unilateral protrusion acetabuli. Rheumatoid arthritis (RA), osteomalacia, the Marfan pattern, or ankylosing spondylitis are among conditions that can result in bilateral (B/L) protrusion acetabuli.
What is the treatment for acetabular protrusion?
Total hip arthroplasty with lateralization of the mug to a typical position offers a reliable long-term option for individuals with significantly more severe arthritis.
Can the acetabulum be repaired?
The majority of acetabular fractures require surgical correction. Your surgeon may perform open reduction and internal fixation (ORIF), depending on the pattern and severity of your damage. Your surgeon will reposition the broken pieces of bone using an ORIF.
Is acetabular protrusion painful?
The femoral head occasionally protrudes into the true pelvis, a condition known as protrusion acetabula. It has been linked to osteoarthritis and hip discomfort in young people.