Arthritis on back
What is Back Arthritis?
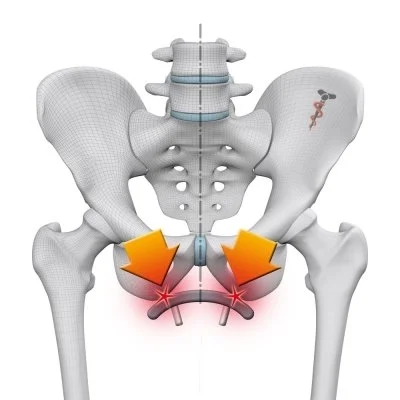
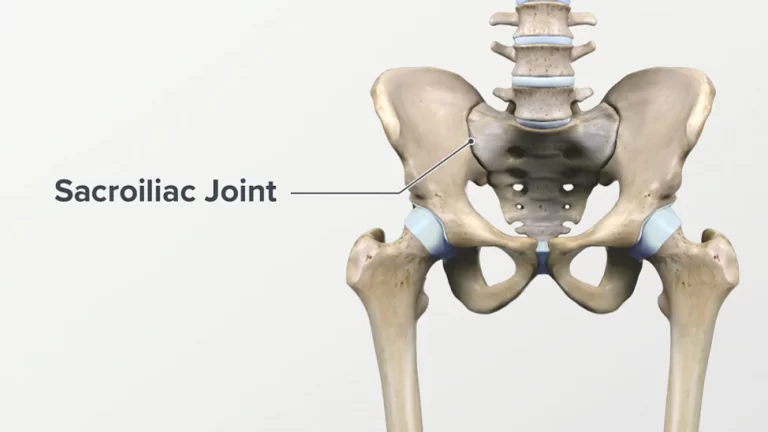
Spinal Back arthritis is inflammation of the facet joints within the spine or sacroiliac joints between the spine and the pelvis. it’s going to be related to wear and tear, autoimmune disorders, infection, and other conditions. Sometimes, the inflammation can also affect the sites where ligaments and tendons attach to the bones of the spine. no matter the exact location, arthritis within the back or neck can be painful and often becomes chronic.
The joints in your spine are known as facets. Facets are lined with cartilage that permits movement as the joints in the spine rub together. When the cartilage gets damaged, it causes friction within the joints, which results in inflammation. This inflammation can cause back pain.
What types of back arthritis are there?
There are many sorts of arthritis that can affect your back, but the 2 most common types are osteoarthritis and rheumatoid arthritis.
- Osteoarthritis (OA): the foremost common form of back arthritis, osteoarthritis may be a degenerative joint disease that causes the cartilage cushioning at the end of joints to gradually wear down, causing pain and stiffness within the back. Individuals with OA frequently experience mechanical pain that worsens with activity and movement and improves with rest. the danger of osteoarthritis increases with age.
- Rheumatoid arthritis (RA): Rheumatoid Arthritis is an autoimmune disorder that affects the lining of the joints. This inflammatory arthritis frequently affects the cervical region of the spine (neck). it’s more commonly diagnosed in women.
- Fibromyalgia: Widespread muscle pain and fatigue are chronic causes.
- Polymyalgia rheumatica: An inflammatory disease that causes widespread muscle pain and stiffness.
- Spondyloarthritis: this is often a group of inflammatory diseases that affects both the joints and the areas where the ligaments and tendons are attached to the bones. There are several sorts of spondyloarthritis, including :
- Ankylosing spondylitis: this is often a type of spinal arthritis that causes inflammation of the vertebrae and the joints at the base of the spine.
- Psoriatic arthritis: this is often an autoimmune disorder triggered by psoriasis and it is characterized by an itchy, scaly rash.
- Reactive arthritis: during this type of arthritis, a gastrointestinal or genital infection probably triggers joint inflammation. it always affects the lower back.
- Enteropathic arthritis: this is often a type of arthritis linked to inflammatory bowel disease.
- Undifferentiated spondyloarthritis
- Juvenile spondyloarthritis
Though each of those spondyloarthritis conditions can bring on different symptoms, all of them can cause inflammation and pain in the spine. The treatment for spinal arthritis varies counting on several factors, including:
- type and severity of arthritis
- level of pain
- age
- overall health status
Because arthritis may be a chronic disease (meaning there is no cure), the treatments typically specialize in pain management and preventing further damage to the joints. Other types of arthritis that can result in backaches can be caused by conditions, such as:
Infections
Other autoimmune diseases (like lupus or psoriasis)
Crystals forming in joints (gout)
Causes of Back Arthritis
- The Aging process
- As your body ages, the fluid that lubricates your joints — called synovia — can become inflamed. This makes it harder to maneuver as our joints
- get stiff. Repetitive use is another explanation for back arthritis that accompanies age. Completing the identical motion over and over can cause the joint to
- wear out.
- Injury or Trauma
- Suffering an injury to your back, like in a sports or auto accident, can create connective tissue. That connective tissue can cause arthritis that restricts joint
- movement and causes stiffness and pain. Arthritis may occur even after a big period of time post-injury.
- Degenerative Disease
Some diseases cause the body to interrupt down prematurely. These are referred to as degenerative diseases. some degenerative diseases that can cause arthritis include:
- Rheumatoid arthritis
- Diabetes
- Degenerative disk disease
- Autoimmune disorders
- Having one of these diseases doesn’t guarantee that you will get arthritis, but your chances will go up significantly.
Symptoms of Arthritis in the Back
Common symptoms of back arthritis may include:
- Back pain – especially within the lower back – tends to be worse in the morning, particularly half-hour after waking up. The pain subsides with activity as the day progresses.
- Back stiffness
- Intermittent joint pain which will be aggravated by motion
- Other areas of the body have pain and swelling (inflammatory arthritis)
- Pain that disturbs sleep is usually an indicator of osteoarthritis
- Swelling and tenderness in one or more joints and these changes can also be triggered by weather changes
- Sensing of bone grinding or rubbing when moving the spine
- Loss of flexibility within the joints is mainly experienced as an inability to bend or pick something off the floor
- Whole-body weakness
- Fatigue
- Headaches
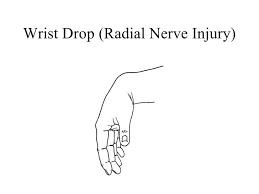
- A sensation of pinching, tingling, or numbness during a nerve or along the spinal cord
- Bone soreness within the lower spine
- Burning sensation after physical activity
- Muscle spasms
- Decreased range of motion
- Bone spurs (extra bits of bone around the affected joints that sense like hard lumps)
Some of the late signs of back arthritis include:
- Pain that radiates toward the arms and legs
- Muscle weakness
- Loss of bowel or bladder function
- Loss of coordination or changes within the capability to walk
- Severe back spasm
- Kyphosis (humped spine deformity)
Back pain and Stiffness
While back pain may be a common symptom, not everyone with back arthritis experiences it. Stiffness, which occurs because the joint hardens, maybe a frequent complaint among those with back arthritis. It can inhibit you from doing simple activities, such as gardening or getting dressed. Both of those symptoms can be assisted significantly with physical therapy exercises for lumbar arthritis. Increasing your elasticity and range of motion can help reduce the pain. Your physiotherapist can achieve this with targeted movements that strengthen the muscles and take the strain off your joints.
Swelling and tenderness
Some people feel swelling and tenderness around the arthritic vertebrae. While this symptom isn’t the most common, it can interfere with daily activities and cause an excellent deal of discomfort. As inflammation sets in, the world can swell. This causes tenderness thanks to pressure on the spine.
Nerve pain or numbness
As arthritis causes joints to interrupt down, bone spurs can form. These are available in contact with nerves in the spinal column and cause tingling, pain, and numbness in other areas. You may not notice these sensations all the time, but they will become problematic when doing even the most basic activities — like bending over to tie your shoes or reaching up to urge something from the top shelf.
How do doctors diagnose back arthritis?
If you experience lower back pain or stiffness for quite 2 weeks, you ought to see a doctor for a medical evaluation. A diagnosis of spinal arthritis can be broken down into 3 steps. you’ll expect the following during your consultation with a doctor:
- Medical history taking – You will be asked to describe your symptoms, other medical conditions, current medications, experience with other treatments, family medical records, and general lifestyle habits, eg. exercise, smoking, and alcohol habits.
- Physical examination – aimed toward assessing overall general health, musculoskeletal status, nerve function, reflexes, and evaluation of the problematic joints of the rear. Your doctor is going to be looking at muscle strength, flexibility, and your ability to perform daily living activities like walking, bending, and reaching.
- Scans and tests – Scans could also be ordered to assess the presence or severity of joint damage. this will be visualized with an X-ray. For a more detailed assessment of the vertebral canal, medulla spinalis, nerve roots, discs, and ligaments, a CT scan or resonance imaging (MRI) may be ordered. Blood tests or testing of the synovia inside a joint may also be used to confirm a spinal arthritis diagnosis.
Treatment for Back Arthritis
Nonsurgical treatments for back arthritis
Depending on the type of arthritis you have and how it is affecting your back, you’ll treat you with medications, such like:
- Pain-relieving medications (like acetaminophen)
- Nonsteroidal anti-inflammatory drugs (NSAIDs, like ibuprofen) both relieve pain and reduce inflammation
- Creams and ointments which will relieve pain
- Corticosteroids, like prednisone and cortisone, are either taken orally or injected into a joint, to decrease inflammation and reduce pain
- Disease-modifying antirheumatic drugs (DMARDs) and biologics if you’ve got rheumatoid arthritis
Pain management specialists specialize in holistic management in which injections play a key role. Injections are safe, effective, non-surgical interventions and options include :
- Facet Joint Injections: Facet joint injections involve placing needles near the troublesome joints under x-ray guidance followed by the injection of medicines to alleviate pain.
- Radiofrequency Treatment: This procedure involves placing special needles under x-ray guidance, near the nerves carrying the pain sensation. These nerves are then treated using the electrical current produced by radio waves. This decreases the pain signals being transmitted to the brain resulting in pain relief. This procedure can provide prolonged pain relief and doesn’t require a hospital stay or prolonged rehabilitation.
Surgical Treatment
Here are a number of the most common back surgeries, and therefore the conditions each help.
Discectomy
Discs are the tiny cushions between the bones of your spine (the vertebrae) and allow them to move without grinding against each other. Discectomy removes the damaged part of a herniated disc that’s putting pressure on the nerves of your spinal cord. Surgeons often perform discectomy through a really small incision, which is named a microdiscectomy. They either use small tools placed through a tube into your back, or a laser to get rid of the damaged area of the disc.
Nucleoplasty (also called plasma disc decompression or percutaneous discectomy) may be a newer variation of the procedure for people with milder herniated discs. The surgeon inserts a little needle into the disc that is causing pain. The needle releases radiofrequency energy, which removes a little amount of tissue in the center of the disc — shrinking it to reduce pressure and pain.
Who it helps: People with a ruptured intervertebral disc that is pressing on nerves of the spinal cord and causing radiating pain or weakness in the arm or leg.
Pros: Discectomy can reduce radiating pain or other symptoms of a ruptured intervertebral disc.
Cons: It won’t help other causes of back pain. Surgery also won’t help the disc from getting herniated again. And together with typical surgical risks such as bleeding and infection, it can damage nearby nerves or blood vessels.
Laminectomy
Laminectomy is surgery to get rid of part or all of the lamina, the bony roof that sits over the vertebral canal. It’s done to widen the vertebral queue and relieve pressure on spinal nerves from spinal stenosis, a herniated disk, an injury, or a tumor.
Who it helps: People with back or neck pain, sometimes together with numbness or weakness in the arm or leg, that hasn’t improved with conservative treatments like NSAIDs or physiotherapy.
Pros: Laminectomy relieves numbness, radiating pain, and weakness caused by compressed nerves. It can also enhance bowel and bladder problems caused by nerve compression.
Cons: It isn’t as effective for pain within the back as it is at relieving symptoms from compressed nerves, and any improvements you experience can fade if your arthritis eventually worsens. Dangers of this procedure range from bleeding and infection to nerve damage.
Spinal Fusion
Spinal fusion welds together two or further vertebrae in your spine to stabilize them and keep them from moving. Fusing the vertebrae prevents pain once you bend, lift or twist. This surgery is additionally done to stabilize bones of the spine after an infection or tumor has damaged them.
Who it helps: This surgery is often helpful for people who have back pain with movement from a herniated disk, spinal stenosis, scoliosis, infection, vertebral fracture, or tumors.
Pros: Spinal fusion can help to alleviate pain when you move.
Cons: Joining the vertebrae together will make your spine less flexible, so you’ll lose some range of motion. Sometimes symptoms come after surgery.
Vertebroplasty and Kyphoplasty
These two comparable procedures ease pain and other symptoms from compression fractures of the vertebrae, which are generally caused by osteoporosis. Both involve bolstering fractured bone with a cement-like material that’s injected into the vertebra. The difference is that with kyphoplasty, the doctor places a little balloon-like device into the compressed vertebra and inflates it to restore height and reduce the deformity.
Who they help: People with backache and decreased function caused by compression fractures of the spine.
Pros: These operations are minimally invasive, and they are frequently very effective at relieving the pain of a compression fracture. About 75% of individuals regain movement and are able to get active afterward.
Cons: Risks of the procedure include numbness, bleeding, infection, and weakness. If you’ve got osteoporosis, you’ll develop more compression fractures and continue to have pain after the procedure.
Foraminotomy
This procedure removes bone spurs and other blockages to widen the world around the vertebrae and relieve pressure on compressed nerves.
Who it helps: People with narrowing of the spine (stenosis) caused by arthritis, disc degeneration, tumors, or bone diseases like Paget’s Disease.
Pros: Foraminotomy can relieve symptoms caused by the nervous disorder, including pain, numbness, and weakness within the arm or leg.
Cons: Risks include infection, blood loss, and nerve damage, there are also a few chances that the procedure won’t relieve your pain, or that your pain will return.
Artificial Disc Replacement
This procedure replaces a worn or damaged disc within the spine with a manmade disc made from either metal or a combination of metal and plastic. It’s an alternative to fusion surgery.
Who it helps: People with back pain caused by damaged discs within the spine.
Pros: Artificial disc replacement relieves back aches and improves mobility. It can restore more normal movement in your spine compared to fusion surgery.
Cons: It might not completely eliminate pain.
Depending on the condition causing your back pain, you’ll have more than one type of surgery to choose from. Discuss the advantages and risks of each procedure with your doctor, also as your preferences, to seek out the one that will best suit your condition and treatment goals.
Physiotherapy Treatment
Exercise
Exercise could also be the last thing on your mind when your back is hurting, but it’s a critical part of managing spinal arthritis. Gentle exercises, like yoga and Pilates, can help increase mobility and reduce pain.
Regular strength training and adaptability exercises such as stretching can help strengthen back and core muscles, which support a healthy spine.
Cardiovascular exercise like swimming or walking promotes good circulation in the spine and helps maintain a healthy weight. ask your healthcare provider before beginning any exercise program.
- Stretching
If you’ve got muscle stiffness in your back, stretching can loosen your muscles and facilitate your movement more easily. There is a spread of stretches you can do, but commonly targeted areas include:
- Hamstrings
- Glutes
- Lower back
- Abs
Stretching these muscles can help decrease strain on your back and improve your posture.
Hamstring Stretch
When you have OA of the spine, the hamstring muscles (the muscles that line the back of your thigh) tend to get tight. This exercise helps to stretch the hamstring muscles, helping you are feeling more flexible.
Lie on your back with the leg to be stretched straight with a belt around the bottom of your foot. Using the belt for support, elevate your leg until, At the back of your thigh and knee, you feel a gentle stretch. Hold for up to 30 seconds. Slowly lower. Perform 3 repetitions on all sides, 1 time daily.

2. Knees-to-Chest Stretch
Lie on your back in a supine position and pull one knee toward your chest, using your hands. Be gentle, there’s no have to force this action. Hold it there for 15 seconds and then return your foot to the floor. Do about 10 to fifteen lifts and then repeat with the other leg. Knee-to-chest should be done once or twice each day. Doing it very first thing in the morning and at the end of the day, to alleviate compression on your spine. If you’ll do a one-legged knees-to-chest without ache, try lifting both legs.

3. Gentle Spine Twist
Lie on your back together with your knees bent and your feet flat on the floor. Keep your shoulders nice and firm on the ground, too. Gently roll both bent knees to at least one side and stay there for 10 to 15 seconds. Breathe! Return to the beginning position and repeat the gentle spine twist on the opposite side. As with the knees-to-chest stretch, do 10 to fifteen of these once or twice per day.

4. Cat-Cow Stretch
Position yourself on your hands and knees. First, arch your back gently then slowly move to an edge where you allow your abdomen to sag. Go to each position submaximally only. The cat-cow makes an excellent warm-up for the bird-dog exercise, and it helps mobilize your facet joints at the rear of your spine.

5. Child’s Pose
These stretch targets are the low back and mid-back directly. Start on your hands and knees together with your hands put under the shoulders and hips over the knees. Transfer your buttock back toward your heels, touching it if possible. Allow your chest to subside toward the floor and rest on your thighs (if possible) until you are feeling a stretch in the butt and low back. If you would like to stretch your upper back and arms, keep your arms call in front of you as you hold.
Otherwise, you’ll choose to put your hands by your side.
The stretch hold for 30+ seconds for 2-3 sets.
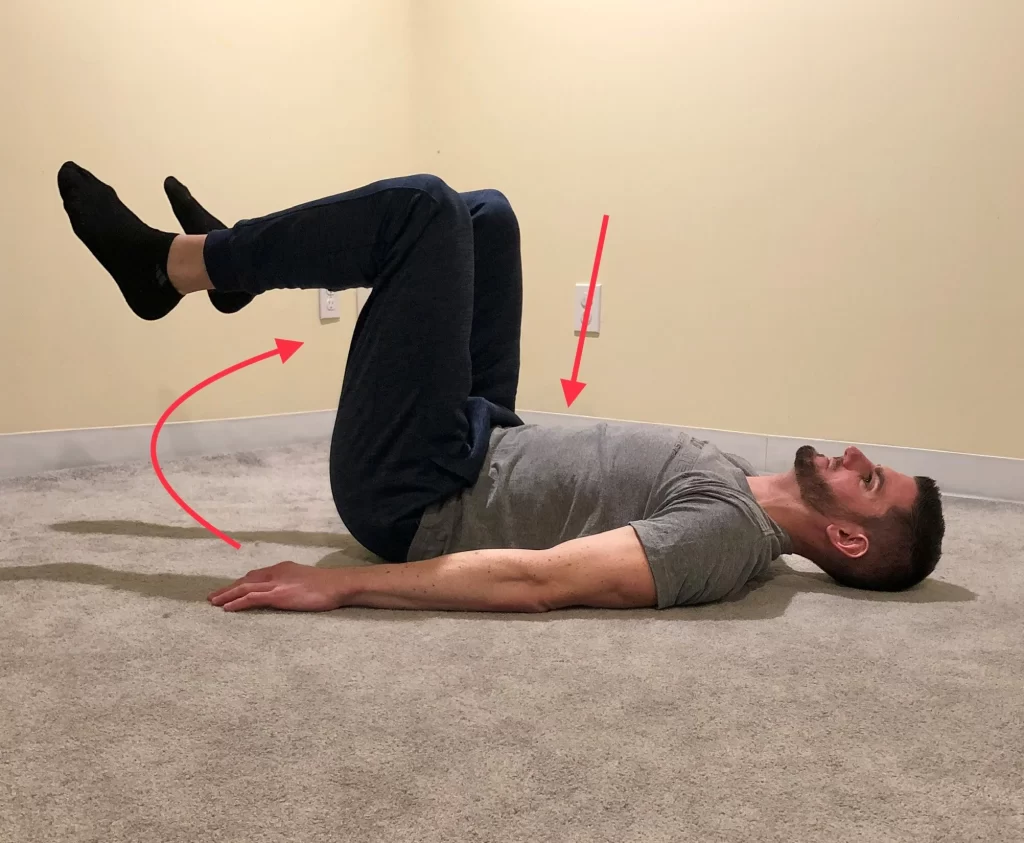
6. Double Knee Raise
Lie on your back in a supine position with both knees bent and feet flat on the floor. Before starting the move, ensure your lower abdomen is tight (your belly should feel tight as if to guard yourself if someone was going to punch you in the stomach). this may keep your low back from arching. Then, lift both feet off the floor as you slowly bring your knees up to hip level. Hold for a flash before returning to the starting position.
Repeat for 10-15 repetitions for 2-3 sts. If your back curves at any time it means the move is just too hard for you. you’ll modify to single leg lifts or even just practice tightening your abs and holding. don’t hold your breath.

7. Plank
Move to the ground on your hands and knees. Put yourself on your forearms at shoulder level apart, elbows directly under the shoulders, and forearms parallel to every other. Keep good upper body posture and a straight spine as you move your weight onto both your knees (easier) or toes.
Your low back shouldn’t be curved nor the hips are flexed with the butt up in the air. Once you’ve found the right position, specialize in keeping the abs tight and breathing.
Hold for 10-30 seconds for 2-3 sets. you’ll build to 60+ seconds with time. If planking on the knees remains too difficult, you’ll start by standing at an incline against the wall or a board. To progress, you’ll do a plank on an exercise ball.

8. Bridge
Lie on your back together with your knees bent and feet flat on the floor at hip-width apart. Tighten your abs and squeeze the butt as you lift your hips off the ground as high as you’ll go. If you notice any cramping in your hamstrings or your back hurts, try again with a deep specialization in muscle activation in your abs and butt.
Hold for five seconds at the top of each repetition and repeat 10 times. Complete 2-3 sets. To progress, you’ll try a single-leg bridge or hold weight at your hips.

9. Clamshell Exercise
This exercise strengthens the muscles on your outer hips and lower abdominals, aiding the overall stability of your lower spine and legs.
Lie on your side with both knees bent. Tighten your lower abdominal muscles by pulling in your belly button towards the floor without holding your breath. Keeping your feet together, slowly take your top knee up as if your legs are opening sort of a clamshell. don’t roll backward. Slowly lower your knee. Perform 10 repetitions on all sides, 1 time daily.
10. Gluteus Strengthening
This exercise will facilitate your strengthening of the gluteus muscles (the large muscles at the back of your hip), aiding in trunk control, leg stability, and balance while you stand and walk.
Lie on your stomach together with your hips over a pillow to support your back. Keeping the leg to be exercised straight, squeeze your buttocks and take the leg up slightly off the bed. Slowly lower. Perform 10 repetitions on all sides, 1 time daily.
11. Abdominal Strengthening
This exercise develops the body’s ability to contract and control its abdominal muscles, resulting in increased support of the spine.
Lie on your back in a supine position keeping the spine and pelvis neutral and making a curve in your knees. Tighten your lower abs muscles by pulling in your belly button towards the spine without holding your breath. Breathe continuously while keeping up the abdominal contraction, holding for 10 seconds. Do 3 sets of 10 repetitions, 1 time daily.
12. Core Building
Strong core muscles facilitate your maintaining good posture. If you suffer from back arthritis, building your core muscle can help improve symptoms and decrease your pain.
Whether you’re doing planks, modified crunches, or side bends, it’s an honest idea to consult a physical therapist or personal trainer to learn how to do the exercises correctly. this may prevent injury or further stress on your back.
13. Improve Balance
We introduce specific movements and activities to enhance your balance and increase stability to prevent trips, falls, or further injury. We also prescribe a low-impact fitness routine for you to strengthen the spine, hip, and abdomen muscles to extend mobility and improve balance.
14. Training for daily activities
Daily activities can become a challenge if you’ve got advanced arthritis or the spine. We help train you to urge up from the bed, bathtub, or chair and bend or devour objects with greater ease.
15. Walking
Walking may be a low-impact form of exercise that can help with aerobic conditioning, heart and joint health, and mood. it’s essential to wear proper shoes and stay hydrated, whether or not the walking is not strenuous. it’s often sensible to walk slowly initially and then increase the pace when possible. A person might want to start a walking routine on flat, even surfaces before getting to uphill, downhill, or uneven surfaces.
16. Cycling
As Arthritis increases the danger of cardiovascular disease, it’s vital to keep the heart as healthy as possible. Cycling can help improve cardiovascular function. Riding a stationary bike are often a safe way to get the joints moving and improve cardiovascular fitness. A benefit of a static bike is that a person can be supervised while riding. an individual can also ride their bikes outsides to get fresh air. In addition to improving aerobic conditioning, cycling can decrease stiffness, increase leg strength and range of motion, and build endurance.
17. Flowing movements, such as tai chi and yoga
- May reduce arthritis pain
- Helps improve strength and balance
- May lower stress and anxiety
- Low impact
- Suitable for all age groups
18. Pilates
Pilates may be a low-impact activity that can increase trusted Source flexibility for enhanced joint health. It is often helpful to do Pilates poses that activate the core muscles and emphasize motions that assist with stability. Pilates is often good for overall movement patterns, almost like tai chi and yoga.
People new to Pilates should start slowly and seek advice from a certified trainer if possible.
19. Water exercises
Water helps support weight by minimizing gravity, which suggests that water exercises do not impact heavily on the joints. Swimming, water aerobics, and other gentle water exercises can increase range of motion, strength, flexibility, and aerobic conditioning. they will also reduce trusted Source joint stress and stiffness.
20. Acupuncture
Acupuncture is an older Chinese practice that uses a small, thin syringe to stimulate acupuncture points on the body to promote healing.
Acupuncture for backache involves the practitioner inserting a syringe into specific trigger points on the body (e.g., lower back, hip, back of the knee).
The syringe touching these points is believed to stimulate the central system nervous and may release chemicals that could assist alleviate symptoms and relieve pain. Acupuncture is related to a significant decrease in pain intensity, enhanced functional mobility, and better quality of life.
21. Massage Therapy
Massage therapy may be a therapeutic approach to pain management. A certified massage therapist will use techniques to massage and manipulate tissues and muscles to release deep tension. additionally, massage therapy boosts circulation, promoting repair and reducing inflammation within the muscles, tissues, and joints. Massage therapy can improve range of motion and adaptability, alleviate pain, and improve emotional and mental well-being on a short-term basis. If you can’t see a massage therapist, you’ll use massage devices and self-massage at home.
22. Meditation
Mindfulness-based practices like meditation can assist the body in reducing stress, and relaxing. When stress is decreased, inflammation levels and tension in the body also reduce, which may give relief to those living with back pain.
investigation shows that meditation can help to decrease acute stress and pain response within the body. In addition to the physical advantage of meditation, numerous people living with chronic pain find it beneficial for enhancing their emotional and psychological state.
Meditation has been proven beneficial in decreasing anxiety and depression and promoting deeper sleep. All of those offer advantages to people with arthritis, enhancing their overall quality of life. There are numerous different types of meditation approaches. Research accessible apps and online instructional videos to search for the right meditation method for you.
23. Resistance Training
Adding resistance strength training to your exercise routine allows you to focus on specific muscle groups while focusing on a strong core and stability. Resistance exercises are often done with body weight, resistance bands, or some appropriately weighted dumbbells.
24. Hot and cold packs
Hot packs stimulate blood flow to the injured area, soothing the pain, while cold packs decrease inflammation and swelling. just in case no heat or ice packs are available, you’ll use a flannel cloth and soak it in warm or cold water.
25. Transcutaneous Electrical Nerve Stimulation (TENS)
It blocks your nerves from sending ache messages to the brain. It uses a little electronic device that sends pulses to the nerve endings by creating a tingling sensation to appease the pain.
26. Hydrotherapy
It uses water to alleviate the symptoms of arthritis. Patients perform specialized exercises in water with temperatures starting from 33 to 36 degrees Celsius with the guidance of a licensed physiotherapist.
27. Use of braces or taping
If you’ve got advanced spine arthritis, we’d recommend taping or using special braces to support your joints.
Home Remedies and Lifestyle
There are a variety of home remedies and lifestyle changes that can be added to your arthritis management techniques. These are often very helpful in reducing pain so you’ll live a full, active life.
- Weight Loss– When you’re carrying extra weight, it puts extra pressure on the spine, resulting in numerous conditions, including back pain and spinal arthritis. Maintaining a healthy weight can decrease pressure and stress on the joints and decrease back pain. Aim to eat a healthy, diet by consuming many fruits, vegetables, whole grains, and protein. Avoid processed foods also as foods high in sugar to help lose extra weight.
- Staying active — To fight the aches and stiffness that include spinal arthritis, staying mobile is one of the best things you can do. Your therapist can work with you on active and passive techniques and also as recommended daily exercises to keep the spine flexible and mobile.
- Strengthening your core — Strong supporting muscles play a key role in holding up the spine and taking pressure off the joints. physiotherapy programs will involve targeted treatment programs to strengthen core muscles and stabilize the spine.
- Improving your posture — together with a stronger core, actively that specialize in posture improvement can help to evenly distribute weight and put less stress on the spinal joints, which may help with arthritis in the back symptoms.
- Practicing a healthy lifestyle — From managing your weight to ergonomic adjustments to eating anti-inflammatory foods, your therapist can provide information on how lifestyle factors contribute to arthritis in the back.
- Quit Smoking- Smoking affects quite your lungs—it affects all tissues in the body and reduces the body’s ability to heal, making arthritis more resistant to treatment. Smoking is related to lower back pain and intervertebral disc disease, and smokers report high levels of pain compared to nonsmokers. There are many methods to assist you to quit smoking. Your healthcare provider can direct you to the proper smoking cessation program for you.
See your doctor if you feel any of the following:
- Pain that’s sharp, stabbing, and constant.
- Pain that causes you to limp.
- Pain that lasts quite 2 hours after exercise or gets worse at night.
- Pain or swelling that doesn’t get better with rest, medication, or hot or cold packs.
- Large increases in swelling or your joints sense “hot” or red.
FAQ
Can Physical Therapy Help Arthritis in the Back?
Physical therapy is very beneficial for arthritis back pain treatment. A certified physiotherapist can teach you physical therapy exercises for lower back
arthritis which will decrease your symptoms and get you back on your feet. Back pain is one of the most common reasons people seek professional help
from a physiotherapist. Strengthening the muscles around the vertebrae permits the muscles — not the joints — to do the work. Stronger muscles will facilitate your move with less pain and discomfort. physiotherapy is crucial to decreasing the symptoms of back arthritis.
Can arthritis cause numbness?
Numbness is usually a symptom of nerve involvement. as an example, numbness within the arm may be connected to nerve irritation in the neck. In such a
situation, turning or bending the top to the involved side may increase the symptoms. for instance, a pinched nerve within the right side of the neck may cause numbness within the arm and hand when a person starts to look back over the right shoulder. If nerve irritation becomes more rigorous, the arm and hand may become weak. A physical examination of X-rays and an MRI of the neck and electrodiagnostic tests could also be useful in establishing the
diagnosis.
Am I at risk for arthritis?
Certain factors make it more likely that you simply will develop arthritis. you’ll control some risk factors, et al. you cannot. By changing the danger factors you can control, you’ll decrease your risk of getting arthritis or making arthritis worse.
Can children get arthritis?
Yes, children can get arthritis. the foremost common type of arthritis found in children is juvenile idiopathic arthritis (JIA), also referred to as childhood arthritis or juvenile rheumatoid arthritis.
Signs and symptoms of childhood arthritis may involve:
Joint pain
Swelling
Fever
Stiffness
Rash
Fatigue (tiredness)
Loss of appetite
Inflammation of the attention
Difficulty with daily living activities (ADL) like walking, playing, and dressing.
Childhood arthritis causes permanent harm to the affected joint or joints. Early diagnosis and proper treatment are important to stop or minimize permanent damage. there’s no treatment for childhood arthritis, but few children with childhood arthritis achieve permanent remission, which suggests the disease is no longer active.
Is arthritis serious?
Arthritis is extremely serious. it’s actually Canada’s most prevalent chronic health condition. Left untreated, it can cause significant and often irreparable damage to your joints, and in some cases your skin, organs, and other areas of the body leading to pain, fatigue, loss of function, and disability which will present considerable challenges to your quality of life. there’s no cure for most forms, so once you’ve got been diagnosed, arthritis is with you at all times.





3 Comments