Benign Prostatic Hyperplasia (BPH)
What is Benign Prostatic Hyperplasia (BPH)?
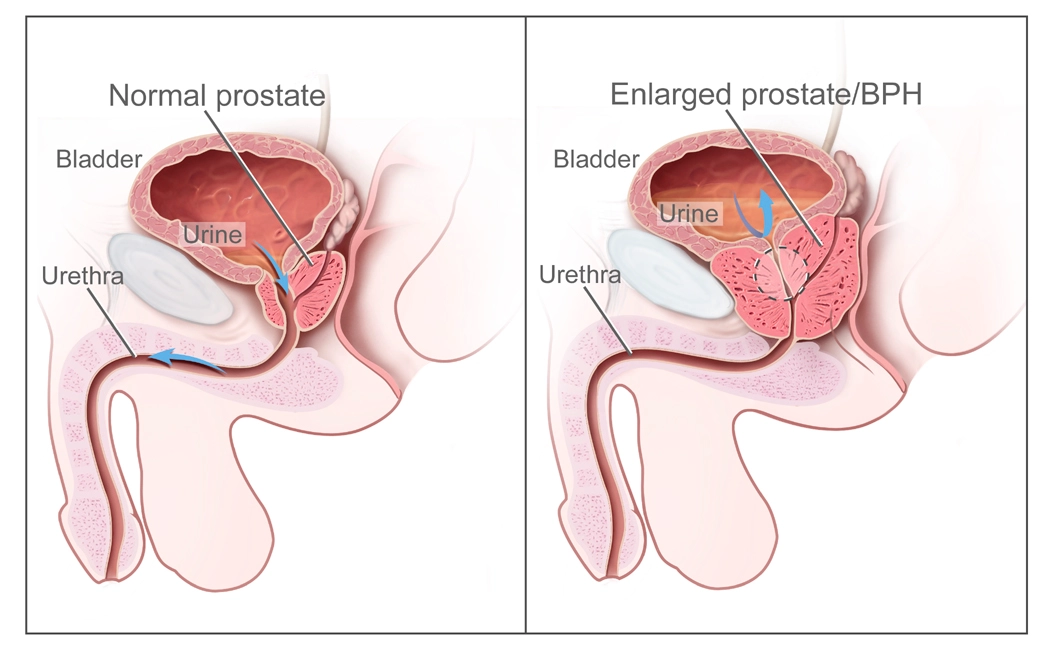
- The expansion of the prostate and surrounding tissue is known as benign prostatic hyperplasia or BPH. As a man ages, his prostate goes through two key growth phases. The prostate doubles in size in the early stages of puberty. The second lasts for the majority of a man’s life and starts at age 25. Your prostate may enlarge with age. BPH is the point at which it becomes problematically huge.
- The urethra is compressed by the growing prostate. The wall of the bladder thickens. The bladder may get weaker and less able to empty over time. The bladder then holds onto the urine. Many of the BPH lower urinary tract symptoms (LUTS) are caused by these issues. Your healthcare team may use this information to decide if and what kind of therapy to recommend for you if you have BPH.
How Does the Prostate Work?
Prostate function mostly involves producing fluid for semen. It weighs roughly an ounce and is about the size of a walnut. It is positioned in front of the rectum and beneath the bladder. It circumscribes the urethra, a tube. Urine is transported via the urethra from the bladder to the penis.
Who is at Risk for BPH?
- Men over 50, since aging increases the risk of BPH
- Men with BPH in their fathers
- Overweight or obese men
- Men who don’t maintain their level of activity
- A small percentage of males with ED (erectile dysfunction )
Symptoms of Benign Prostatic Hyperplasia (BPH)
An enlarged prostate may irritate or obstruct the bladder. One of the most prevalent signs of BPH is the frequent need to urinate. This may involve the requirement to urinate every one to two hours, primarily during the night.
Other symptoms of BPH are listed below:
Feeling that your bladder is full even after passing urine is known as incomplete emptying.
- Frequency: the frequent ask to urinate, roughly every hour to two hours.
- Intermittency: the requirement to repeatedly stop and resume urinating.
- Urgency: feeling the need to urinate immediately, as if you can’t wait to do so.
- Weak stream: a weak emptying flow.
- Straining: difficulty urination or the need to push or strain to pass urine.
- Nocturia: the requirement to use a bathroom more than twice at night.
Causes of Benign prostatic hyperplasia:
- BPH’s causes are unclear. It mostly affects older guys. Changes in hormones are considered to be involved.
- Testicular hormones might be the primary cause. For instance, men’s blood levels of active testosterone decrease with age. Levels of estrogen remain constant. When these hormonal changes drive the development of prostate cells, BPH may result. Regarding the function of dihydrotestosterone (DHT), there is another idea. This hormone in males promotes the growth of the prostate. Studies indicate that DHT levels are greater in elderly males. Testosterone production declines.
Diagnosis of BPH
Symptom Score Index:
- Your doctor may discuss the BPH Symptom Score Index with you if you have any changes in your urine or any associated symptoms. This exam was created by the American Urological Association (AUA) to evaluate symptoms related to the bladder.
- When diagnosing BPH, this is frequently the initial step. BPH can be rated as minor to severe based on the score. Your medical history and the findings may be discussed between you and your healthcare practitioner. The International Prostate Symptom Score (IPSS) is another name for this.
Physical Exam:
- Usually, the following step is a digital rectal exam (DRE). You either bend over or lie on your side during a DRE. To feel the prostate gland’s back wall, the doctor reaches into your rectum with a gloved, lubricated finger. The physician is searching for lumps, hard areas, discomfort, or enlargement. This 10-to-15-second test is a valuable tool for issue identification.
Urine Tests:
- The purpose of these tests is to measure your urine discharge efficiency. This indicates to the physician whether the urethra is full or blocked. There are several kinds:
- This procedure examines a urine sample to look for vital indicators including blood, infection symptoms, glucose (sugar), protein, and other elements that may help your urologist determine the source of your symptoms. Testing urine is another way to look for bladder cancer. See your doctor as soon as possible if you have blood in your urine, have pain or burning when you pass urinate, or are unable to pass urine at all.
- Urine remaining in the bladder after urinating is measured using post-void residual volume, or PVR. The purpose of this is to identify the issue. It can also be carried out ahead of surgery.
- The urine flow rate is measured using uroflowmetry. The purpose of this is to identify the issue. It can also be carried out ahead of surgery.
- Pressure in the bladder during urination is measured using urodynamic pressure flow research.
Scans:
- The purpose of these examinations is to measure the prostate’s dimensions. Among the BPH scans are:
- The size and form of the prostate may be seen by using ultrasounds to examine the body.
A cystoscopy is a diagnostic procedure that uses a scope to examine the bladder or urethra.
More in-depth scans include computed tomography (CT) and magnetic resonance imaging (MRI). If surgery is required to restore the urine flow, these are carried out. An extremely clear picture of the prostate and its surroundings is produced by these scans. It displays the exact location and size of the prostate enlargement.
Blood Tests:
- Blood tests may be performed if cancer is suspected.
- Blood tests that measure the prostate-specific antigen (PSA) are used to screen for prostate cancer. The PSA blood test measures PSA levels, which are unique to the prostate gland. You may get this blood test performed in a lab, hospital, or doctor’s office. A few days before the test, refrain from having sex as this might inflate the PSA reading.
- Very low PSA is seen in the blood when the prostate is healthy. A rapid increase in PSA might indicate a problem. PSA levels can increase as a result of both benign (non-cancerous) prostate enlargement and prostate inflammation (prostatitis). Cancer is the most dangerous reason for a spike in PSA.
Treatment of Benign Prostatic Hyperplasia (BPH)
- BPH has a wide range of therapies. The best course of action for you will be determined in consultation with your healthcare professional. Treating mild instances might not even be necessary. Minimally invasive surgery (surgery performed without anesthesia) might be useful in some situations. Additionally, sometimes a mix of therapies is most effective.
The main types of treatments for BPH are:
- Active Surveillance
- Prescription Drugs
- Less Invasive Surgery
- More Invasive Surgery
Active Surveillance:
- BPH frequently just has to be actively monitored. This implies that your BPH will be monitored regularly but not actively treated; routine urologist visits may be necessary to keep an eye on things. An annual exam is typical. Before making any further recommendations, your healthcare practitioner will search for more serious or recent problems. Exercise and diet plans are frequently suggested as ways to control or avoid symptoms.
- It is advisable for men with mild to moderate symptoms to engage in active monitoring. For men who are not concerned by the symptoms of BPH, it is also a possibility.
Prescription Drugs:
- For men with BPH, prescription medication may also be an option. Among the drug types are:
- To lessen the symptoms of BPH, alpha-blockers are medications that relax the muscles in the bladder and prostate. They don’t reduce prostate size, but if there is a blockage, they could help with urine flow. The immediate onset of action is one advantage of alpha-blockers. Dizziness, lightheadedness, fatigue, and breathing difficulties are possible side effects. An excellent candidate would be a man with moderate to severe BPH or a man who finds his symptoms uncomfortable. If you have cataract surgery scheduled soon, alpha-blockers are not a smart option.
- Among the medications that block alpha waves include, doxazosin, silodosin, tamsulosin, and terazosin.
- 5-Alpha receptor inhibitors are medications that work by preventing DHT from entering the prostate and increasing urine flow. Male hormone DHT has the potential to accumulate in the prostate and lead to prostate enlargement. These medications may lessen the chance of BPH issues and the requirement for surgery. Reduced desire (sex desire) and erectile dysfunction are side effects. The medications must be continued to stop the symptoms from returning. For men with exceptionally big prostate glands, they can be the best option.
- These prescription medications, which include finasteride and the drug, may take many months to start working completely.
- An alpha-blocker and a 5-alpha reductase inhibitor are used in combination treatment. Together, they might be able to prevent the progression of BPH more effectively than either medication alone. You can experience greater adverse effects from taking two medications than from taking just one. Dizziness, erectile dysfunction, weakness or lack of energy, and a decrease in blood pressure after rising from a seated or lying down position are a few possible adverse effects. Antimuscarinics may be added by a urologist for people experiencing symptoms of an overactive bladder. Uncontrollably squeezing the bladder muscles is known as an overactive bladder. Urine demand becomes frequent and urgent as a result. It may result in leakage or incontinence. The bladder muscles are relaxed by antimuscarinics.
- This therapy is a suitable fit for men with bigger prostates.
Possible drug combinations include
- Finasteride and doxazosin
- One pill contains both the medication and dutasteride, the combined drug.
- Alpha-blockers and antimuscarinics
- Healthcare professionals do not advocate for phytotherapies or herbal remedies. The saw palmetto plant is one popular herb. Much significant research demonstrates their ineffectiveness. Supplements differ in terms of purity and quality as well.
Less Invasive Surgery:
- Minimally invasive surgery, also known as MIST, can frequently be performed as an outpatient procedure without the need for an overnight hospital stay. Usually, recovery happens more quickly. Certain MISTS do not lessen your chance of requiring a second operation or prescription refills. Whenever you are thinking about a MIST or even more invasive surgery, make sure to consult your urologist about the rates of repeat treatments.
- Men with the following symptoms or those who have taken BPH medication but it did not help are good candidates:
- weak urine stream
- straining to begin urinating
- blockage of the urinary system, bladder stones, and blood in the urine
- Not completely emptying
- Loss of prostate blood
- There are several options for less invasive surgical procedures. The choice will be based on your personal preferences, general health, and the size of your prostate.
- Prostatic urethral lift (PUL): inserts small implants into the prostate using a needle. The enlarged prostate is lifted and compressed by these implants, removing the obstruction to the urethra. These implants are difficult to remove and remain in the body permanently. Both local and general anesthesia are options for PUL procedures.
- The body is not sliced during this therapy, and tissue is not removed or damaged. Many eligible men have enlarged prostates and problems related to the urinary system. This kind of prostate surgery has less sexual side effects than other forms. Even if you had a PUL, you may still have an MRI. Consult your physician about any allergies you may have to nickel, titanium, or stainless steel, as well as how PUL may affect the picture quality of any future MRIs performed to detect prostate cancer. Future research may be useful in determining the long-term durability of PUL therapy, which has been assessed in current trials spanning five years.
- Water vapor thermal therapy (WVTT): employs steam or water vapor to kill prostate cells, compressing the urethra. This procedure can be performed under local anesthesia at a physician’s office or following pain medication. It makes use of a unique portable tool that has a needle on the end. It produces steam by mixing radiofrequency radiation with water. Rapid cell death is caused by the steam and needle. The prostate then shrinks as a result of the body’s natural healing process eliminating the dead tissue.
- If men have tried prescription medicines and found them ineffective, or if they do not want to take medication for BPH, they may be suitable candidates. Men who would rather forego surgery or who wish to escape any negative consequences on their sexual life can also be suitable candidates.
- You may need to use a catheter for a few days due to blood in your pee. Urinating painfully or often should stop in two to three weeks. Erectile dysfunction and other sexual adverse effects are unlikely.
- According to current research, symptoms should improve for at least five years.
- Temporary Implanted Prostatic Devices (TIPD): are placed into the prostatic urethra using a cystoscope, where they remain for about a week until being taken out by a urologist. Its function is to alter the morphology of the urine duct temporarily. Urine flow and BPH symptoms are marginally improved when the urethra is reshaped, resulting in a small decrease in prostatic obstruction. This low-risk procedure can be done in the operating room or in an office. It could remove a bladder obstruction. Urinary tract infections, incontinence, and urethral scarring are among the uncommon side effects of TIPD. Some men suffer burning when they pass urine and intense or frequent urges to go to the toilet.
- Prostate Artery Embolization (PAE): radiologists use a radiologic technique to attempt and reduce the whole prostate gland to alleviate symptoms by blocking the blood supply to the gland. There are no long-term data available for this more recent technique to determine its durability. Urinary problems are likely alleviated by PAE, at least temporarily—less than a year. For the usual treatment of LUTS, there is insufficient evidence to support the use of PAE over other readily accessible less invasive treatments; however, in a very limited patient population, there is evidence of a brief advantage of PAE when compared to observation.
- Catheterization: utilizes a catheter—a tube—in the bladder to remove waste. Catheters can be inserted via the urethra or by making a tiny bladder puncture just above the pubic bone. Men with a clogged prostate and issues controlling their bladder might benefit from this alternative. Even yet, the advantages of catheters are transient. One danger is infection. Men who are waiting for surgery or for their medicine to take effect are the greatest candidates for this treatment. They also assist in cases of infection and in situations when surgery is not recommended for men who are nearing the end of their lives. Two categories exist:
- Every six to eight hours, clean the area where the catheter is inserted and taken out. Someone else or you can accomplish this. When the urine flow ceases, the catheter is taken out for this.
The longer the catheter stays in the bladder is referred to be indwelling.
More Invasive Surgery:
- More invasive surgery is advised in situations of severe BPH or when other treatments are ineffective. Best for surgery if you:
- Are not able to urinate
- Suffer from kidney damage
- Experience recurrent urinary tract infections
- Have a large amount of bleeding
- Urinary bladder stones
- There are several choices available for more invasive surgical procedures. The choice will be based on your health, the knowledge of your physician, and your preferences. The options below are listed from least to most intrusive.
- Transurethral incision of the prostate (TUIP): is employed to enlarge the urethra in cases when a little obstruction is caused by a tiny prostate gland. Small incisions are made by the surgeon during TUIP in the prostate and bladder neck, where the urethra connects to the bladder. Urination becomes easier as a result of the urethra becoming wider and the prostate’s strain on it is lessened. One to three days are spent in the hospital. After surgery, a catheter is placed in your bladder for one to three days. For certain males, further care is required. Men who require surgery but do not wish to have their prostate removed completely are ideal candidates.
- Photoselective vaporization (PVP): is a method that uses a strong laser to burn prostate tissue. Most guys have little trouble having a PVP. The operation is performed in the hospital as an outpatient procedure, or occasionally in the doctor’s office. There aren’t many adverse consequences. Most men can discontinue medicinal treatment after PVP. Most men can benefit from this procedure, except those who have very big prostates. This technique is also helpful for men who are more likely to bleed, such as those who take blood thinners or have weak hearts, because it results in very little blood loss.
- Transurethral resection of the prostate (TURP): is a frequent procedure for BPH.TURP cuts and removes tissue using either laser light or electric current. Anaesthesia and a device called a resectoscope that is placed into the penis are used to do this. The resectoscope has an electrical loop, light, and irrigating fluid. The loop closes blood arteries and tears tissue. Using a catheter, the excised tissue is drained into the bladder and out of the body. Men who have moderate to severe symptoms of BPH and need surgery can be ideal candidates for TURP.
- Holmium laser enucleation of the prostate (HoLEP) is the process by which a surgeon inserts a resectoscope into the urethra through the penis. Excess prostate tissue is destroyed using a laser that is placed into the resectoscope. There is extremely minimal bleeding and no need for incisions. Your hospital stay may just last one night. Although a catheter is utilized, it is often taken out the next day. Men who want to avoid more invasive surgery yet have bigger prostates can benefit from this procedure. Men who are more likely to bleed, such as those on blood thinners, would make suitable candidates for HoLEP.
- Thulium laser enucleation of the prostate (ThuLEP) is comparable to HoLEP but employs a distinct kind of laser. Similar to HoLEP, the surgeon inserts a resectoscope into the urethra through the penis. Excess prostate tissue is destroyed using a laser that is placed into the resectoscope. Men who want to avoid more invasive surgery yet have bigger prostates can benefit from this procedure. There is extremely minimal bleeding and no need for incisions. Your hospital stay may just last one night. Although a catheter is utilized, it is often taken out the next day. Men who are more likely to bleed, such as those who use blood thinners, could also be ideal candidates for ThuLEP.
- Transurethral vaporization of the prostate (TUVP): is the procedure when a resectoscope equipped with an electrical current-sending instrument, a lens, and a light is inserted into the urethra by the surgeon to eliminate prostate tissue. Little blood vessels are sealed by the heat from the electrical current, lowering the chance of bleeding. Both bleeding and fluid absorption are minimal. You can often go home without a catheter after spending one night in the hospital. TUVP may be a suitable option for men with bigger prostates who want to avoid more invasive surgery.
- Transurethral water–jet ablation (TWJA): makes use of water jets under high pressure to remove extra prostate tissue. Using ultrasonography, the surgeon first pinpoints the exact site of the extra tissue. After that, the region is targeted by the high-pressure water jets. To lessen the chance of bleeding, the surgeon inserts a second device to plug tiny blood arteries. To avoid blood clots, the patient must spend one night in the hospital for bladder irrigation. After the procedure, you might need to wear a catheter for around 48 hours, but you should be able to return home the next day.
- A simple prostatectomy uses robotic or laparoscopic-aided surgery to remove the prostate gland entirely. The surgeon must perform this procedure with competence. Only males with the biggest prostate glands are eligible for this. This treatment is long-term. Following surgery, you will likely spend a few days in the hospital and have restricted activity for a few weeks. While you recover, a catheter will often be required for one to two weeks.
Summary
The expansion of the prostate and surrounding tissue is known as benign prostatic hyperplasia or BPH. As a man ages, his prostate goes through two key growth phases. The prostate doubles in size in the early stages of puberty. The second lasts for the majority of a man’s life and starts at age 25. Your prostate may enlarge with age. BPH is the point at which it becomes problematically huge.
The urethra is compressed by the growing prostate. The wall of the bladder thickens. The bladder may get weaker and less able to empty over time. The bladder then holds onto the urine. Many of the BPH lower urinary tract symptoms (LUTS) are caused by these issues. Your healthcare team may use this information to decide if and what kind of therapy to recommend for you if you have BPH.
FAQs
What is benign prostatic hyperplasia’s primary cause?
Prostate enlargement’s true etiology is uncertain. The size of the gland and testosterone levels may be influenced by aging-related factors and modifications in the testicular cells. Males who have had their testicles removed early (for example, as a result of testicular cancer) are not at risk of having BPH.
How can an enlarged prostate be reduced as quickly as possible?
The greatest ways to reduce an enlarged prostate naturally involve a mix of healthy eating habits, exercise, cutting back on liquids before bed, and behavioral adjustments like frequent urination.
Which course of action is most effective for benign prostatic hyperplasia?
For the majority of BPH patients, TURP is the most successful therapy. However, medicines and less intrusive therapies are preferred in people 65 years of age and above. Elderly individuals may experience greater post-operative problems and need more time for recovery.
How can I get my prostate to get smaller?
Bigger prostate glands are treated with 5-alpha reductase inhibitors. If the prostate gland is swollen, they reduce it. The two available 5-alpha reductase inhibitors are Propecia and the drug.
Does an enlarged prostate benefit from drinking lots of water?
All things considered, drinking lots of water is beneficial to your overall health. Therefore, it’s beneficial for your prostate to consume a lot of water. Your body’s organs all depend on adequate water to operate healthily and effectively.
Reference:
- Benign prostatic hyperplasia (BPH) – Diagnosis and treatment – Mayo Clinic. (2023, February 21). https://www.mayoclinic.org/diseases-conditions/benign-prostatic-hyperplasia/diagnosis-treatment/drc-20370093
- Professional, C. C. M. (n.d.). Benign Prostatic Hyperplasia. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/9100-benign-prostatic-hyperplasia
- image: Benign prostatic hyperplasia (BPH) – Diagnosis and treatment – Mayo Clinic. (2023, February 21). https://www.mayoclinic.org/diseases-conditions/benign-prostatic-hyperplasia/diagnosis-treatment/drc-20370093