Cauda Equina Syndrome
What is Cauda Equina Syndrome?
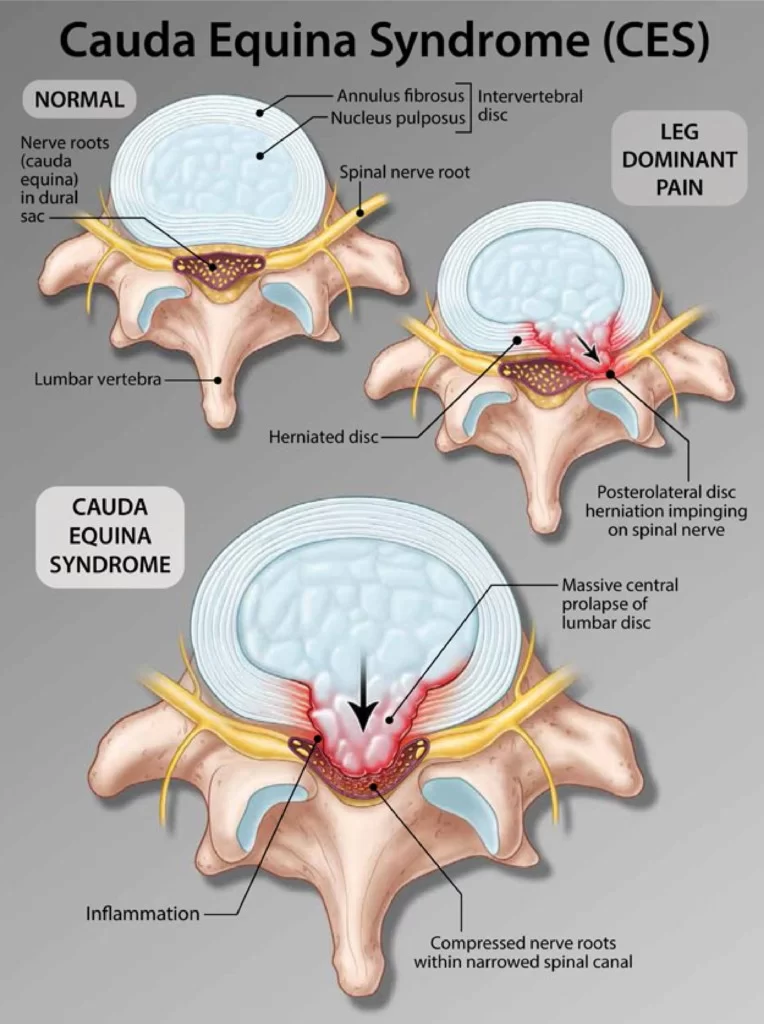
Cauda equina syndrome (CES) occurs when the nerve roots of the cauda equina are compressed and disrupt motor and sensory function in the lower extremities and bladder.
Patients with this syndrome are often admitted to the hospital in a medical emergency. CES can lead to Bladder-Bowl incontinence and weakness or paralysis of Both Lower limbs.
It was first described in 1934.
Cauda equina syndrome is a medical emergency needing urgent hospital treatment to avoid permanent bladder and bowel problems.
Causes of Cauda Equina Syndrome:
Cauda equina syndrome occurs more often in adults than in children, but it can occur in children who have a spinal birth defect or have had a spinal injury.
- A herniation (bulging) of a spinal disk in the lumbar area that presses on the nerves (the most common cause).
- Narrowing of the spinal canal (stenosis).
- A spinal lesion or tumor ( metastatic cancer and Paget’s disease) or cancer
- A spinal infection( staphylococcus and tuberculosis bacteria ), inflammation, hemorrhage, or fracture.
- A complication from a severe lumbar spine injury such as a car crash, or fall, or other traumatic injury such as a stabbing.
- A birth defect such as an abnormal connection between blood vessels (arteriovenous malformation).
Symptoms of Cauda Equina Syndrome:
Symptoms of cauda equina syndrome can develop suddenly but may take weeks or months. The onset of the condition is often described using the following distinctions:
* Acute onset is marked by a rapid development of symptoms that often includes severe low back pain and significant loss of bladder and bowel function. In an acute onset, sensory and motor deficits in the lower body typically develop within 24 hours.
* Gradual onset can develop over progressively, and symptoms may come and go over the course of several weeks or months. Gradual onset usually typically includes partial or intermittent loss of bowel and bladder function, as well as recurring low back pain in combination with muscle weakness and numbness and bladder and/or bowel incontinence or dysfunction. Sciatica may also occur in one or both legs.
* Loss of bowel or bladder function may include incontinence (inability to retain urine or stool), and/or constipation (inability to eliminate urine or stool).
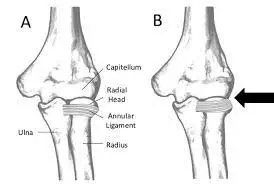
* Neurological symptoms in the lower body. Weakness, tingling, or numbness in the legs, and/or feet on one or both sides of the body is a common symptom. Lower body weakness or numbness may make it difficult to walk or stand.
* Altered sensation in the “saddle region,” or saddle anesthesia. The saddle region is the area of the body that would be in contact with a saddle when sitting on a horse. This region includes the groin, the buttocks and genitals, and the upper inner thighs. With cauda equina syndrome, all or parts of this region may have neurological symptoms of numbness, tingling, and/or weakness.
* Sexual dysfunction that has come on suddenly.
How Diagnosis is done in Cauda Equina Syndrome?
* A medical history, in which you answer questions about your health, symptoms, and activity.
* A physical examination to assess your strength, reflexes, sensation, stability, alignment, and movements.:-
Physical examination for cauda equina or conus medullaris syndromes would be incomplete without tests for a sensation of the saddle and perineal areas, bulbocavernosus reflex, cremasteric reflex, and anal sphincter tone, findings for all of which are likely to be abnormal.
Muscle strength of the following muscles should be tested to determine the level of lesion:
L2 – Hip flexors (iliopsoas)
L3 – Knee extensors (quadriceps)
L4 – Ankle dorsiflexion (tibialis anterior)
L5 – Big toe extensors (extensor hallucis longus)
S1 – Ankle plantar flexors (gastrocnemius/soleus)
Poor anal sphincter tone is characteristic of cauda equina syndrome. Babinski sign or other signs of upper motor neuron involvement suggest a diagnosis other than cauda equina syndrome, possibly spinal cord compression.
Physical examination for cauda equina or conus medullaris syndromes would be incomplete without tests for a sensation of the saddle and perineal areas, bulbocavernosus reflex, cremasteric reflex, and anal sphincter tone, findings for all of which are likely to be abnormal.
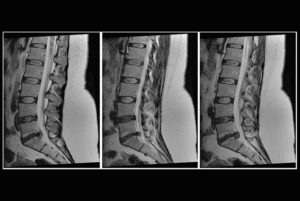
Magnetic resonance imaging (MRI) scan, which uses magnetic fields and computers to produce three-dimensional images of your spine.
A myelogram – an X-ray of the spinal canal after injection of contrast material – can pinpoint pressure on the spinal cord or nerves.
A computed tomography (CT) scan.
Differential Diagnosis in Cauda Equina Syndrome:
- Conus medullaris syndrome
- Herniated Nucleus Pulposis
- Lumbar disc herniation
- Lumbar Radiculopathy
- Lumbar vertebrae fracture
- Mechanical back pain
- Peripheral neuropathy
- Spinal cord compression
- Spinal tumor
- Sacral fractures
- Abscesses
- Lymphoma
- Central or centerolateral disk prolapsed
- Space-occupying lesions that compress nerve roots have been described as causes of CES.
- Spinal Canal stenosis
- Spinal Anesthesia
- Neoplasm
- Ischemia
Prevention of CES:
Early diagnosis is the key for CES.
Signs AND Symptoms that allow early diagnosis include changes in bowel and bladder function and loss of sensation in the groin. Changes in sensation can start as pins and needles lead to numbness. Changes in bladder function may be changes to stream or the inability to empty the bladder fully. If a person progresses to full retention intervention is less likely to be successful.
Treatment in Cauda Equina Syndrome:
Medical treatment :
- Depending on the cause of your CES, Treatment is Vary :
- NSAIDS, corticosteroids. These can reduce swelling.
- If you are diagnosed with an infection you may need antibiotics. If a tumor is responsible, radiation or chemotherapy may be needed after surgery.
Surgical Treatment :
Urgent surgery is usually the treatment of choice. The goal is to reverse the symptoms of neural dysfunction. Left untreated, CES can result in permanent paralysis and Bladder Bowl incontinence.
The management of true cauda equina syndrome frequently involves surgical decompression. When cauda equina syndrome is caused by a herniated disk early surgical decompression is recommended.
Cauda equina syndrome of sudden onset is regarded as a medical/surgical emergency.
Surgical decompression by means of laminectomy or other approaches may be undertaken within 6,24 or 48 hours of symptoms developing if a compressive lesion, e.g., ruptured disc, epidural abscess, tumor, or hematoma is demonstrated. Early treatment may significantly improve the chance that long-term neurological damage will be avoided.
Physiotherapy Treatment :
Physiotherapy Treatment is Variable According To Weakness In the Lower Limb, Mostly Lower Limb Assessment Procedure Will be Taken And Then Treatment Plan Will Be Decided.
Goals of Physiotherapy Treatment :
- Maintain R.O.M (Range of Motion)
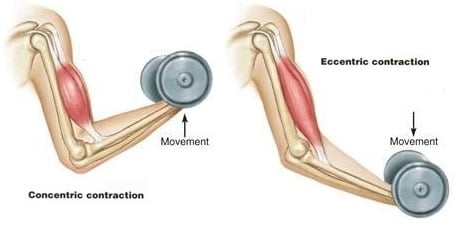
- Strengthening Exercise of Lower Limb.
- Gait Training.
- Improve standing Balance.
- Restoring Bladder-Bowl Control
- Avoid Bed-Sore
MMT(Manual Muscle Testing) of the Lower limb is performed and according to which strengthening exercise of the lower limb is planned. Regular progression of muscle power will be tested in between.
Explained The Condition To The Patient Then Rehabilitation Procedure Will Be Started Mostly by Sit To Stand, Gait Training, Walker Walking Then Balancing Exercise, Stair Climbing, and Related Exercise According To The Condition and the Involvement of Neuron Lesion Treatment Will Be Variable.
Exercise is highly effective in Strengthening Exercise- balance following a CES diagnosis.
Regular physical activity can also be helpful when it comes to improving circulation and blood flow to the lower extremities — a common problem for those living with this condition.
Consistent exercise can boost mood and decrease symptoms of depression, making it a must for those diagnosed with CES.
How to gain Bladder-Bowl control?
Rehabilitation of CES depends on the severity of the injury. If permanent damage occurs, then impairment in Bladder-Bowl control may result. Once the surgery is performed, resting is required until the bladder-bowel dysfunction can be assessed. Urinary catheterization may help with bladder control. Gravity and exercise can help control bowel movements.
Physiotherapy Treatment mainly for Bladder-Bowl Control is Pelvic floor exercises that assist in controlling bowel movements. These exercises can be done standing, lying, or on all fours with the knees slightly separated. Full recovery of bowel and bladder control can take as long as two years. Electrical stimulation, IFT is also used to strengthen of Bladder-Bowl Muscle.

Gait Training in CES?
Gait Training depends upon power in lower limb muscles. if standing balance is achieved then gradually gait training started. Parallel Bars are used initially then gradually gait training with a walker and as gait improves try to reduce support and then stick and as progress improves normal gait without any support gait started.





6 Comments