Cerebral Palsy
What is a Cerebral Palsy?
Cerebral palsy (CP) is a neurological disorder that affects movement, muscle tone, and motor skills. It is caused by damage or abnormalities in the developing brain, usually before or during birth, but sometimes it can occur in early childhood. The specific cause of CP is often unknown, but it can be associated with factors such as premature birth, low birth weight, infections during pregnancy, genetic abnormalities, and certain maternal health conditions.
DEFINITION:
- Cerebral palsy is a chronic disability of the central nervous system origin characterized by aberrant control of the movement of posture, appearing early in life and not the result of progressive neurological disease.
TOPOGRAPHIC CLASSIFICATION OF CEREBRAL PALSY:
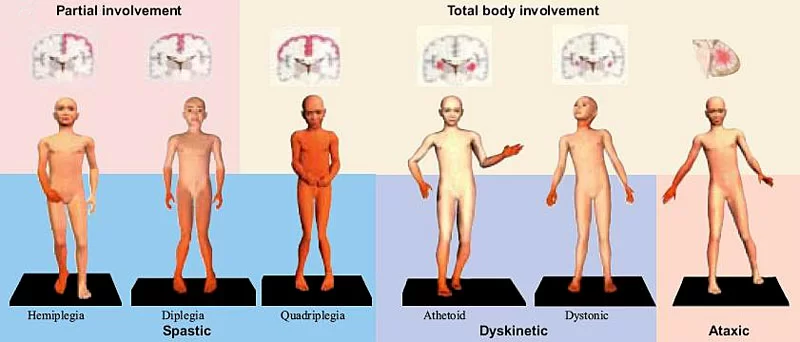
- MONOPLEGIA: Paralysis of one limb involvement.
- HEMIPLEGIA: UMNL of one side of body involvement.
- DIPLEGIA: UMNL of all four limbs involvement but legs more involved than arms. May be symmetric or asymmetric.
- QUADRIPLEGIA(TETRAPLEGIA): Total loss of all four limbs and torso.
- DOUBLE HEMIPLEGIA: Bilateral UMNL. Arms and legs involved. Pseudobulbar palsy also.
- TRIPLEGIA: Paralysis of three limbs, both extremities on one side and one on the other. Paralysis of the upper and lower extremities and of the toes.
PHYSIOLOGICAL CLASSIFICATION OF CEREBRAL PALSY:
MUSCLE TONE:
- Many motor function terms describe Cerebral Palsy’s effect on muscle tone and how muscles work together. Proper muscle tone when bending an arm requires the bicep to contract and the triceps to relax. When muscle tone is impaired, muscles do not work together and can even work in opposition to one another.
- Two terms used to describe muscle tone are:
- Hypertonia/Hypertonic: Increased muscle tone, often resulting in very stiff limbs. Hypertonia is associated with spastic Cerebral Palsy
- Hypotonia/Hypotonic: Decreased muscle tone, often resulting in loose, floppy limbs. Hypotonia is associated with non-spastic Cerebral Palsy
- Two classifications by motor function:
pyramidal (spastic) and extrapyramidal (non-spastic)
PYRAMIDAL OR SPASTIC CEREBRAL PALSY:
- The pyramidal tract consists of two groups of nerve fibers responsible for voluntary movements. They descend from the cortex into the brain stem. In essence, they are responsible for communicating the brain’s movement intent to the nerves in the spinal cord that will stimulate the event. Pyramidal Cerebral Palsy would indicate that the pyramidal tract is damaged or not functioning properly.
- Extrapyramidal Cerebral Palsy indicates the injury is outside the tract in areas such as the basal ganglia, thalamus, and cerebellum. Pyramidal and extrapyramidal are key components to movement impairments.
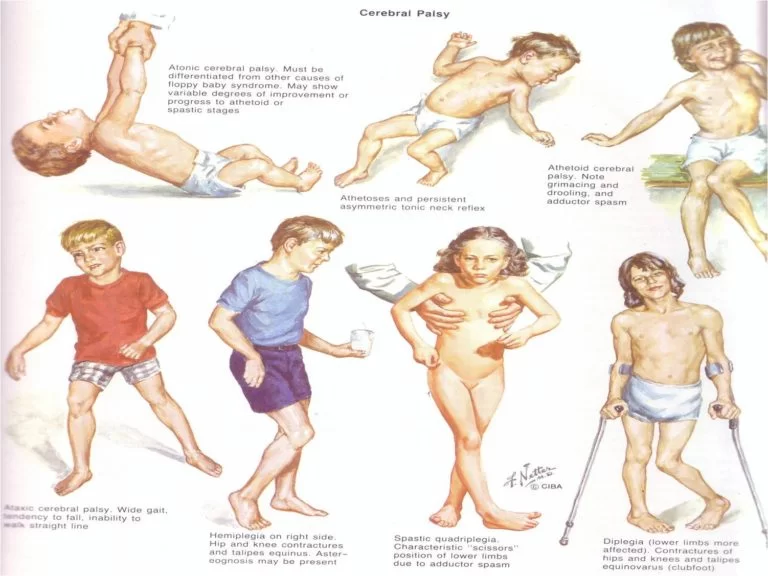
- Spasticity implies increased muscle tone. Muscles continually contract, making limbs stiff, rigid, and resistant to flexing or relaxing. Reflexes can be exaggerated, while movements tend to be jerky and awkward. Often, the arms and legs are affected. The tongue, mouth, and pharynx can be affected, as well, impairing speech, eating, breathing, and swallowing.
- Spastic Cerebral Palsy is hypertonic and accounts for 70% to 80% of Cerebral Palsy cases. The injury to the brain occurs in the pyramidal tract and is referred to as upper motor neuron damage.
- The stress on the body created by spasticity can result in associated conditions such as hip dislocation, scoliosis, and limb deformities. One particular concern is contracture, the constant contracting of muscles that results in painful joint deformities.
- Spastic Cerebral Palsy is often named in combination with a topographical method that describes which limbs are affected, such as spastic diplegia, spastic hemiparesis, and spastic quadriplegia.
EXTRAPYRAMIDAL OR NON-SPASTIC CEREBRAL PALSY:

- Non-spastic Cerebral Palsy is decreased and/or fluctuating muscle tone. Multiple forms of non-spastic Cerebral Palsy are each characterized by particular impairments; one of the main characteristics of non-spastic Cerebral Palsy is involuntary movement.
- Movement can be slow or fast, often repetitive, and sometimes rhythmic. Planned movements can exaggerate the effect – a condition known as intention tremors. Stress can also worsen involuntary movements, whereas sleeping often eliminates them.
- An injury in the brain outside the pyramidal tract causes non-spastic Cerebral Palsy. Due to the location of the injury, mental impairment and seizures are less likely.
- Non-spastic Cerebral Palsy lowers the likelihood of joint and limb deformities. The ability to speak may be impaired as a result of physical, not intellectual, impairment.
- Non-spastic Cerebral Palsy is divided into two groups, ataxic and dyskinetic. Together they make up 20% of Cerebral Palsy cases. Broken down, dyskinetic makes up 15% of all Cerebral Palsy cases, and ataxic comprises 5%.
Ataxic/ataxia:
- Ataxic Cerebral Palsy affects coordinated movements. Balance and posture are involved. Walking gait is often very wide and sometimes irregular.
- Control of eye movements and depth perception can be impaired. Often, fine motor skills requiring coordination of the eyes and hands, such as writing, are difficult.
- Does not produce involuntary movements, but instead indicates impaired balance and coordination
Dyskinetic:
- Dyskinetic Cerebral Palsy is separated further into two different groups; athetoid and dystonic.
Athetoid:
- Athetoid Cerebral Palsy includes cases with involuntary movement, especially in the arms, legs, and hands.
Dystonia/Dystonic:
- Dystonic/Dystonia Cerebral Palsy encompasses cases that affect the trunk muscles more than the limbs and result in fixed, twisted posture.
- Because non-spastic Cerebral Palsy is predominantly associated with involuntary movements, some may classify Cerebral Palsy by the specific movement dysfunction, such as:
Athetosis:
- Slow, writhing movements that are often repetitive, sinuous, and rhythmic
Chorea:
- Irregular movements that are not repetitive or rhythmic, and tend to be more jerky and shaky
Choreoathetoid:
- A combination of chorea and athetosis; movements are irregular, but twisting and curving
Dystonia:
- Involuntary movements accompanied by an abnormal, sustained posture
Mixed:
- A child’s impairments can fall into both categories, spastic and non-spastic, referred to as mixed Cerebral Palsy. The most common form of mixed Cerebral Palsy involves some limbs affected by spasticity and others by athetosis.
GROSS MOTOR FUNCTION CLASSIFICATION SYSTEM (GMFCS):
- The GMFCS is a universal classification system applicable to all forms of Cerebral Palsy. Using GMFCS helps determine the surgeries, treatments, therapies, and assistive technology likely to result in the best outcome for a child.
- Additionally, the GMFCS is a powerful system for researchers; it improves data collection and analysis and hence results in better understanding and treatment of Cerebral Palsy.
GROSS MOTOR FUNCTION CLASSIFICATION SYSTEM(GMFCS) CLASSIFICATION LEVELS:
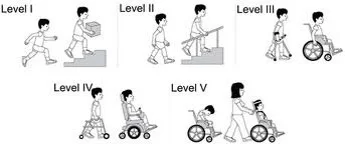
- GMFCS Level I – walks without limitations.
- GMFCS Level II – walks with limitations. Limitations include walking long distances and balancing, but not as able as Level I to run or jump; may require use of mobility devices when first learning to walk, usually prior to age 4; and may rely on wheeled mobility equipment when outside of the home for traveling long distances.
- GMFCS Level III – walks with adaptive equipment assistance. Requires hand-held mobility assistance to walk indoors, while utilizing wheeled mobility outdoors, in the community, and at school; can sit on their own or with limited external support; and has some independence in standing transfers.
- GMFCS Level IV – self-mobility with the use of powered mobility assistance. Usually supported when sitting; self-mobility is limited; and likely to be transported in a manual wheelchair or powered mobility.
- GMFCS Level V – severe head and trunk control limitations. Requires extensive use of assisted technology and physical assistance; and transported in a manual wheelchair, unless self-mobility can be achieved by learning to operate a powered wheelchair.
Causes of Cerebral Palsy
- Congenital cerebral palsy results from brain injury during a baby’s development in the womb. It is present at birth, although it may not be detected for months. It is responsible for CP in about 70% of the children who have it.
- An additional 20% are diagnosed with congenital cerebral palsy due to a brain injury during the birthing process. In most cases, the cause of congenital cerebral palsy is unknown. Some possible causes are:
- Infections during pregnancy:- Mothers can pass infections to the fetus during pregnancy. Prenatal infections are most dangerous in the first few weeks after conception. German measles (rubella) and cytomegalovirus (CMV) during pregnancy are known causes of cerebral palsy. These viruses cause the mother’s immune system to release proteins that not only attack the infection but also cause inflammation in the baby’s brain that interferes with normal development. Mothers who eat raw or undercooked meat can increase the likelihood of getting an infection.
- Infections after birth:- Infections (such as meningitis) contracted by newborns can cause brain damage. Meningitis causes severe inflammation that can damage the motor control centers of the brain.
Severe untreated jaundice: When a newborn has a yellow color to their skin and/or eyes, it is known as jaundice. Jaundice is caused by excess bilirubin, a chemical pigment that is normally filtered out by the liver. It is normal for newborns to experience mild jaundice before their livers fully develop. However, severe jaundice left untreated can turn into a condition known as kernicterus. Kernicterus is characterized by buildup of an unsafe level of bilirubin, which is toxic to the brain - Asphyxiation:- Asphyxiation is a lack of oxygen reaching the brain. It can cause severe brain damage to a baby during birth. Early detachment of the placenta, a ruptured uterus during birth, or the umbilical cord getting pinched in a way that restricts blood flow can cause oxygen deprivation. Choking on an object or a near-drowning experience can also cause asphyxiation that leads to cerebral palsy.
- Head trauma during or after birth:- Blunt trauma to the infant or toddler brain can cause cerebral palsy. Head injuries may occur during labor or delivery or within the first several years of life.
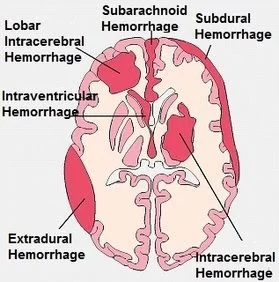
- Brain hemorrhage before birth:- A brain hemorrhage is abnormal bleeding of the brain caused by a ruptured blood vessel, which can cause serious damage to the motor control centers in the brain.
- Genetic causes: There has been some speculation and research to suggest that a minute proportion of cerebral palsy cases are hereditary. This is still being studied, and the number of genetic cases of CP, if they exist, is likely negligible.
- Severe oxygen deprivation to the brain or significant trauma to the head during labor and delivery.
- The physical and metabolic trauma of being born: This can precipitate brain damage in a fetus whose health has been threatened during development.
- Some risk factors that increase the possibility that a child will later be diagnosed with CP include:
- Breech births (with the feet, knees, or buttocks coming out first).
- Vascular or respiratory problems in the infant during birth.
- Physical birth defects such as faulty spinal bone formation, groin hernias, or an abnormally small jaw bone.
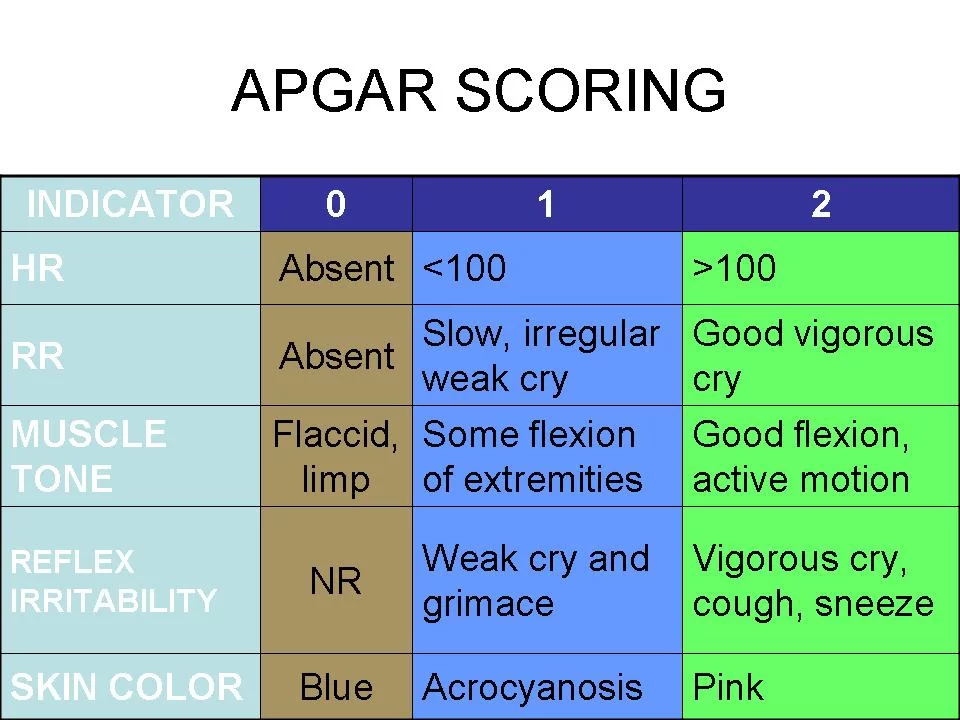
- Receiving a low Apgar score 10 to 20 minutes after delivery. An Apgar test is used to make a basic, immediate determination of a newborn’s physical health. For the test, the infant’s heart rate, breathing, muscle tone, reflexes, and color are evaluated and given a score from 0 (low) to 2 (normal).
- A low birth weight (less than 2,500 grams, or 5 lbs. 7.5 oz.) and premature birth (born less than 37 weeks into pregnancy).
- Being a twin or part of multiple births.
- A congenital nervous system malformation, such as an abnormally small head (microcephaly).
- Seizures shortly after birth.
Signs & Symptoms of Cerebral Palsy
Muscle Tone:
- Proper muscle tone allows limbs to bend and contract without difficulty, enabling an individual to sit, stand, and maintain posture without assistance. Improper muscle tone occurs when muscles do not coordinate together.
- When this happens, those muscles that work in pairs – biceps and triceps, for example – may both contract or relax at the same time, impeding movement and coordination.
- Trunk muscles might relax too much, making it difficult to maintain a tight core; this can result in impaired posture and an inability to sit or to move from a sitting to a standing position.
- A child with Cerebral Palsy may demonstrate any combination of these signs. Different limbs may be affected by different impairments.
- The two most common signs of abnormal muscle tone are hypotonia and hypertonia, but tone can be defined in other ways as well:
- Hypotonia – decreased muscle tone or tension (flaccid, relaxed, or floppy limbs)
- Hypertonia – increased muscle tone or tension (stiff or rigid limbs)
- Dystonia – fluctuating muscle tone or tension (too loose at times and too tight at others)
- Mixed – the trunk of the body may be hypotonic while the arms and legs are hypertonic
- Muscle spasms – sometimes painful, involuntary muscular contraction
- Fixed joints – joints that are effectively fused together preventing proper motion
- Abnormal neck or truncal tone – decreased hypotonic or increased hypertonic, depending on age and Cerebral Palsy type
- Clonus – muscular spasms with regular contractions
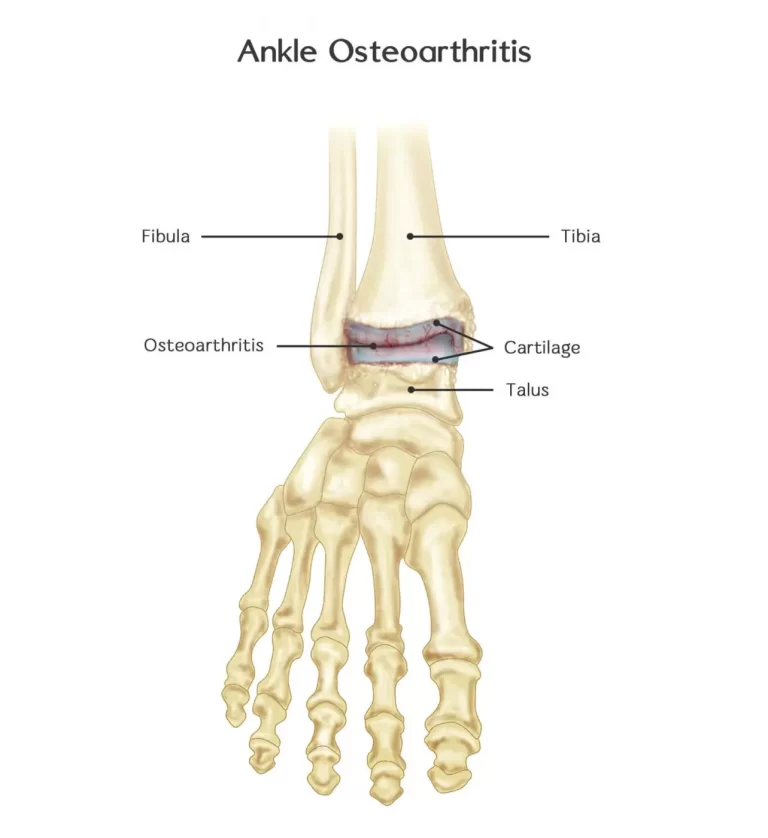
- Ankle/foot clonus – a spasmodic abnormal movement of the foot
- Wrist clonus – the spasmodic movement of the hand
Movement, coordination, and control:
- The impairment of muscle tone affects a child’s limbs and body in different ways, although all children with Cerebral Palsy will likely feel some effect on muscle control and coordination.
- Different muscle control impairments can combine to cause limbs to be perpetually extended, contracted, constantly moving in rhythmic patterns, or jerking spastically.
- Some signs will be more apparent when the child is under stress. Some may be task-related, such as reaching for an object. Sometimes signs will seem to disappear when the child is asleep and muscles are relaxed.
- It is common for a child to experience different types of impaired muscle control in opposite limbs. Coordination and control can likewise be affected differently in each limb.
- The impairment of coordination and control falls under the following types:
- Spastic movements – hypertonic movements where the muscles are too tight resulting in muscle spasms, scissoring of the legs, clonus, contracture, fixed joints, and over-flexed limbs
- Athetoid or dyskinetic movements – fluctuating muscle tone causing uncontrolled, sometimes slow, writhing movements which can worsen with stress
- Ataxic movements – poor coordination and balance-making tasks – such as writing, brushing teeth, buttoning shirts, tying shoes, and putting keys into slots – difficult
- Mixed movements – a mixture of movement impairments, most commonly a combination of spastic and athetoid types, affecting different limbs
- Gait disturbances – control impairments affecting the way a child walks
- Gait disturbances include:
- In-toeing – toes angle or rotate inward
- Out-toeing – toes angle or rotate outward
- Limping – more weight is placed on one foot than the other, causing a dipping, or wavy stride
- Toe walking – the weight is unevenly placed on the toes
- Propulsive gait – a child walks hunched over in a stiff posture with the head and shoulders bent forward
- Spastic and scissor gait – the hips flex slightly making it look like the child is crouching while knees and thighs slide past one another like scissors
- Spastic gait – one leg drags due to muscle spasticity
- Steppage gait – toes drag because the foot drags
- Waddling gait – duck-like walking pattern that can appear later in life
Reflex:
- Certain abnormal reflexes may also indicate Cerebral Palsy. Hyperreflexia are excessive reflex responses that cause twitching and spasticity. Underdeveloped or lacking postural and protective reflexes are warning signs for abnormal development, including Cerebral Palsy.
- Doctor checking child’s reflex
- Reflexes are involuntary movements the body makes in response to a stimulus. Certain primitive reflexes are present at or shortly after birth but disappear at predictable stages of development as the child grows. Specific reflexes that do not fade away – or those that don’t develop as the child grows – can be a sign of Cerebral Palsy.
- Abnormal primitive reflexes may not function properly in children with Cerebral Palsy, or they may not disappear at specific points in development as they do with children with no impairment.
- Common primitive reflexes that may improperly function or persist include, but are not limited to:
- Asymmetrical tonic reflex – when the head turns, the legs on the same side will extend, and the opposite limbs contract like in a fencing pose. Asymmetrical tonic reflex should disappear around six months of age.
- Symmetrical tonic neck reflex – the infant assumes a crawling position when the head is extended. Symmetrical tonic neck reflex should disappear between eight and 11 months.
- Spinal gallant reflexes – when the infant lies on its stomach, the hips will turn towards the side of the body that is touched. Spinal gallant reflexes should disappear between three and nine months.
- Tonic labyrinthine reflex – when the head is tilted back, the back arches, the legs straighten, and the arms bend. The tonic labyrinthine reflex should disappear by three-and-a-half years of age.
- Palmer grasp reflex – when stimulating the palm the hand flexes in a grasping motion. Palmer’s grasp reflex should disappear around four to six months.
- Placing reflex – when an infant is held upright and the back of a foot touches the surface, the legs will flex. The placing reflex should disappear in five months.
- Moro (startle) reflex – when the infant is tilted so his or her legs are above their head, the arms will extend. Moro reflex should disappear in six months.
- Early hand preference can also indicate possible impairments. A child normally develops hand preference in his or her second year. As this is a wide time frame and rough average, the development of hand preference, especially if it is early preference, is cause for concern. Various sources state that early hand preference falls between 6-18 months.
Posture:
- Cerebral Palsy affects posture and balance. Signs may appear as an infant begins to sit up and learn to move about. Typically, posture is expected to be symmetrical. For example, a baby in a sitting position would normally have both legs in front. When bent, they become mirror images of one another.
- Asymmetrical posture means the right and left limbs will not mirror one another. The hip joints are one area where this is often prominent in instances of Cerebral Palsy. One leg will bend inward at the hip, and the other will bend outward.
- Much like reflexes, postural responses are expected reactions when putting a baby in certain positions. They typically appear as the baby develops. Impairment may be a possibility if the responses do not develop, or if they are asymmetric.
- Much like reflexes, postural responses are expected reactions when putting a baby in certain positions. They typically appear as the baby develops. Impairment may be a possibility if the responses do not develop, or if they are asymmetric.
- Common postural responses are:
- Traction
- Landau reflex – when the infant is supported in a lying position, pushing the head down will cause the legs to drop, and lifting the head will cause them to rise. This response appears around four or five months of age.
- Parachute response – when the infant is positioned with his or her head towards the ground, the infant should instinctively reach as if bracing for impact. This response appears around eight to 10 months of age.
- Head righting – when an infant is swayed back and forth, his or her head will remain straight. This response appears around four months of age.
- Trunk righting – when a sitting infant is quickly pushed to the side, the infant will resist the force and use the opposite hand and arm to brace against impact. This response appears around eight months of age.
Balance:

- The impairment of gross motor function can affect a child’s ability to balance. Signs become recognizable as a child learns to sit, rise from a sitting position, and begin crawling or walking. Infants need to use their hands often as they learn these skills. They develop the strength, coordination, and balance to accomplish the task when mastering it without the use of their hands.
- A child’s inability to sit without support can be a sign of Cerebral Palsy. The Gross Motor Function Classification System, or GMFCS, a five-level system commonly used to classify function levels, uses balance while sitting as part of its severity level system.
- Signs to look for when a child sits include:
- Requiring both hands for support
- Having difficulty balancing when not using hands for support
- Unable to sit without using hands for support
- Other signs to look for include, but are not limited to:
- Swaying when standing
- Unsteady when walking
- Difficulty making quick movements
- Needing hands for activities that require balance
- Walking with abnormal gait
- Balance is often the same whether a child’s eyes are open or closed. Balance impairment is most often associated with ataxic, and to a lesser degree, spastic Cerebral Palsy.
Gross motor function (GMF):
- As a child develops, signs of impaired or delayed gross motor function may be noticeable. The ability to make large, coordinating movements using multiple limbs and muscle groups is considered gross motor function.
- Gross motor function may be impaired by abnormal muscle tone, especially hypertonia or hypotonia.
- For example, hypertonic limbs can be too tight, or inflexible, to allow proper flexion and movement; whereas hypotonic limbs may be too loose to properly support a child’s movements.
- As a baby’s brain and body develop, they are expected to reach developmental milestones. Reaching the milestone later than expected, or reaching it but with low quality of movement (such as favoring one side while crawling), are possible signs of Cerebral Palsy.
- Impaired gross motor functions – limited capability of accomplishing common physical skills such as walking, running, jumping, and maintaining balance.
- Delayed gross motor functions – physical skills developed later than expected; often used in conjunction with developmental milestones for predictable stages of development.
- Significant milestones of gross motor function include:
- Rolling
- Sitting up
- Crawling
- Standing
- Walking
- Balancing
- These should be monitored to note when the baby reaches the milestone, and the quality of movement.
Fine motor function:

- Executing precise movements defines the category of fine motor function. Fine motor control encompasses many activities that are learned and involve a combination of both mental (planning and reasoning) and physical (coordination and sensation) skills to master.
- Impaired or delayed fine motor skills are an indicator of possible Cerebral Palsy. Intention tremors, where a task becomes more difficult as it gets closer to completion, is one such sign.
- Examples of fine motor function development are:
- Grasping small objects
- Holding objects between thumb and forefinger
- Setting objects down gently
- Using crayons
- Turning pages in a book
Oral motor function:
- Difficulty in using the lips, tongue, and jaw indicate impaired oral motor function; this is a sign that may be present in up to 90% of preschool-aged children diagnosed with Cerebral Palsy.
- Signs of oral motor function impairment include, but are not limited to difficulty with:
- Speaking
- Swallowing
- Feeding/chewing
- Drooling
- Speech requires proper intellectual and physical development. Cerebral Palsy impairs the physical aspects of speaking by improperly controlling the muscles required to speak. Oral motor impairment can affect:
- Breathing – the lungs, and specifically the muscles controlling inhalation and exhalation necessary for proper speech patterns. The diaphragm and abdominal muscles are important for proper airflow and posture
- Articulating – muscles controlling the face, throat, mouth, tongue, jaw, and palate all must work together to form the proper shape necessary for the pronunciation of words and syllables.
- Voicing – vocal cords are controlled by muscles that essentially stretch the vocal folds between two regions of cartilage.
- Apraxia, an inability of the brain to effectively transmit proper signals to the muscles used in speaking, is one type of speech impairment common to Cerebral Palsy. It is divided into two types:
- Verbal apraxia – affects the articulation muscles, especially regarding the specific sequence of movements needed to carry out proper pronunciation. It is common in children with hypotonia.
- Oral apraxia – affects the ability to make nonspeaking movements of the mouth, but is not related solely to speaking. Examples of oral apraxia would be the inability to lick the lips or inflate the cheeks.
- Dysarthria is another speech impairment common to Cerebral Palsy. Like apraxia, it is a neurological impairment, as opposed to a muscular condition. It is often found in Cerebral Palsy that results in hypertonia and hypotonia. Dysarthria is broken into the following subgroups:
- Ataxic dysarthria – slow, erratic, inarticulate speech caused by poor breathing and muscular coordination
- Flaccid dysarthria – nasal, whiny, breathy speech caused by the inability of the vocal chords to open and close properly. There may be difficulty with consonants.
- Spastic dysarthria – slow, strenuous, monotone speech and difficulty with consonants
- Mixed dysarthria – all three may be present.
- Drooling is another sign of Cerebral Palsy that results from muscles in the face and mouth not being able to properly control coordination. Some specific factors which can contribute to drooling are impairments in:
- Swallowing
- Closing the mouth
- Positioning the teeth
- Inability to move saliva to the back of the mouth
- Tongue thrusting
- Feeding difficulties can be present with Cerebral Palsy. They typically manifest as decreased ability to chew and swallow, and may also involve choking, coughing, gagging, and vomiting.
DIAGNOSTIC STUDY:
- Physical Assessment
- Observe LBW, preterm, and those with low Apgar scores at 5 minutes.
- Observe infants who have seizures, intracranial hemorrhage, metabolic disturbances
- Since control of movement does not occur until late infancy, dx may not be confirmed until after 6 months of age.
Warning signs:
- Physical Signs:
- poor head control after 3 months
- stiff or rigid arms/legs, arching back, floppy or limp posture
- Cannot sit up without support for 8 months
- Uses only one side of the body or only the arms to crawl
- Behavioral Signs:
- Extreme irritability or crying
- Failure to smile by 3 months
- Feeding difficulties
- Persistent gagging or choking when fed
- After 6 months of age, the tongue pushes soft food out of the mouth.
PHYSIOTHERAPY MANAGEMENT:
&
- Physiotherapy especially when started early in life, is helpful in promoting normal motor development, and preventing deformity and contractures.
- In the young child, it aims at reducing abnormal patterns of movement and posture and promoting normal ones so as to enable the child to gain maximal functional independence.
- A number of techniques have been used for this purpose. The neurodevelopmental Bobath technique is commonly used.
- It consists of guiding the child through normal sequences of motor development,
- Inhibition of primitive and abnormal reflexes,
- Reinforcement of normal postural reflexes and
- Facilitation of normal movements.
- The goal of physical therapy is to help individuals:
- Develop coordination
- Build strength
- Improve balance
- Maintain flexibility
- Optimize physical functioning levels
- Maximize independence
- Overcoming physical limitations
- Expanding the range of joint motion
- Building and maintaining muscle tone
- Increasing recreational capabilities
- Identifying alternate ways to perform everyday tasks
- Fostering independence
- Decreasing the likelihood of contractures, bone deformity
- Educating children and parents about adaptive equipment
- Providing sensory stimulation
- Increasing fitness
- Increasing flexibility
- Improving posture
- Improving gait
- Minimizing pain and discomfort
- The largest benefit of therapy to the child with Cerebral Palsy is in the treatment of problematic conditions when they occur, including:
- Muscle atrophy or tightening
- Loss in joint range of motion
- Muscle spasticity
- Pain in muscles and joints
- Joint inflammation
- Contractures (muscle rigidity)
- Physical therapy performed by physical therapists such as,
- soft tissue mobilization (kneading of the muscles)
- joint mobilization
- specialized exercises
- stretching
- endurance exercises designed to meet therapeutic goals
- Exercises often include the use of equipment, such as:
- Weights
- Exercise machines
- Bands
- Rollers
- Balance balls
- Heat and cold packs
- Ultrasound technology
- At some centers, sports or recreation like swimming, dancing, and playing games such as throwing and catching a ball, may be used to help children develop muscles, balance, coordination, and range of motion.
- Swimming, because the child is almost entirely submerged in the water, will give children an opportunity to do exercises they cannot do otherwise; moving against the water, kicking and other beneficial exercises can be accomplished in a pool, sometimes in braces. These methods can provide children with an opportunity to play and have fun.
- Adaptive equipment including braces, splints, walkers, orthotics, wheelchairs, and even computers will be used in therapy; therapists will modify the equipment as needed. The therapist will also play an instructive role in this regard for children and parents, teaching them how to use the equipment.








My son is 6years old.i am at Delhi.
He is suffering spastic cp.
Please suggest
Mob no 9891177064
My son is 5 years old, e is having scissor leg by birth
Please contact Doctor Mainly Pediatric Neurophysician Doctor