Clavicle Fracture
Overview
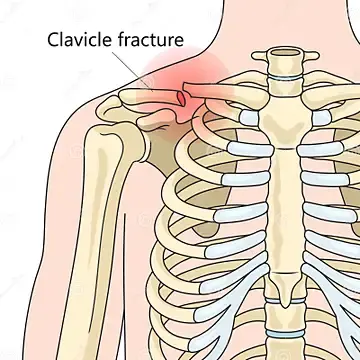
A fracture of the clavicle occurs when one of the primary bones in the shoulder (collarbone) breaks. About 5% of all adult fractures are of this type, making it a fairly common fracture.
It is the most common fracture in childhood. The most common cause of a clavicle fracture is a fall that lands on the lateral shoulder.
Most clavicle fractures result from an outstretched arm or a fall onto the shoulder compressing the bone to the point of breaking. If you have a broken collarbone, moving your arm can be very painful and challenging.
Clavicle fractures are very common injuries in adults (2.5–5%) and children (10–15%), making up 44–66% of all shoulder fractures. It is the most common fracture in childhood.
The clavicle also called the collarbone, connects the shoulder blade to the breastbone. Falls, car crashes, and sports injuries are the main causes of broken clavicles. Newborns can break their clavicle on occasion.
A sling can be used to treat many clavicle fractures, keeping the arm and shoulder immobile until the fractured bone heals. Nonetheless, the fracture can result in a considerable displacement of the broken bone in some clavicle fracture cases.
Relevant Anatomy
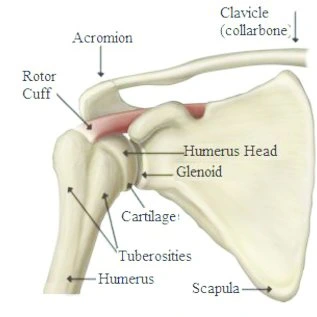
The skeleton’s first ossified bone is the clavicle. It articulates proximally with the sternum (sternoclavicular joint) and distally with the acromion (acromioclavicular joint), acting as the only bony link between the arm and the trunk. Because fibrocartilage rather than hyaline cartilage lines these joints, they are known as atypical synovial joints.
The acromioclavicular and coracoclavicular ligaments attach the clavicle to the scapula, and the sternoclavicular ligaments bind it to the sternum.
There is a “S” shape to the clavicle. The proximal half has an outward (convex) curve that provides room for the neurovascular bundle of the upper limb. The distal half of the scapula concavely curves back to join the acromion and coracoid. Clavicle fractures usually occur at the midshaft, or junction, between these two curves, probably because this is the thinnest area of the bone and does not have ligamentous attachments to neighboring bones.
The body, shaft, and tip make up the clavicle’s three components. The body of the clavicle is shaped like a triangle and has rounded ends. This section of the clavicle runs along your neck and front shoulders. The middle part of the clavicle, called the shaft, extends downward and toward your chest. This is where it narrows and curves around your ribs. The tip of the clavicle finally turns to face your spine from the back. You attach it to your first rib.
When displacement happens, the sternocleidomastoid muscle, which attaches to the proximal portion of the clavicle, pulls the proximal fragment of the fracture superiorly, or cephalad. The distal fragment is inferiorly displaced by the weight of the arm (caudad). Shortening, or the fractured bone ends being pulled past one another, is a common occurrence. This is mainly caused by the pectoralis and subscapularis muscles, which pull the arm inward and towards the chest.
Despite the clavicle’s subcutaneous location and the thin layer of soft tissue covering it, open fractures are uncommon. Nonetheless, tenting—the deliberate stretching of the skin layer above—occurs quite frequently. If treatment is not received, tenting may lead to an open fracture and necrosis of the skin covering it. Therefore, tenting suggests closed reduction or surgical repair.
Epidemiology
Between 2% and 10% of all fractures are clavicle fractures. One in a thousand people experience a clavicle fracture annually. These are the most frequent fractures in children, with men accounting for about two-thirds of all clavicle fractures. The distribution of clavicle fractures is bimodal, with the two peaks being individuals over 55 (falls) and men under 25 (sports injuries). About 20% of clavicular fractures in females and over 30% in males occur in people between the ages of 13 and 20.
Three areas of the clavicle can sustain fractures: 3 percent of cases involve the proximal third, 28 percent involve the distal third, and 69 percent involve the middle third.
Medial clavicle fractures accounted for only 2 to 3 percent of all clavicle fractures in earlier research. Subsequent analysis, however, showed that 9.3% of clavicle fractures involved the medial third. The authors speculate that the association’s widespread use of CT (only CT was used to diagnose 22% of medial clavicle fractures) may be the cause of their higher rate.
The middle third of the clavicle is where the majority of pediatric fractures (95%) occur. These are typically not displaced in children under the age of ten, but most of them are when they get older. Clavicle fractures account for 95% of fractures sustained during childbirth.
The consequences of a low-energy fall are more likely to cause injuries in the elderly, but moderate-to-high-energy mechanisms, such as car accidents or sports injuries, are more likely to cause these injuries in younger people.
Falling onto the shoulder causes approximately 87% of all clavicle fractures. Sports and vehicle accidents are the most common causes of fractures in young people. Riders are the most damaged in traffic accidents, accounting for 75%, after drivers and passengers (26%), people who walk (17%), and motorcyclists.
Unusual causes of clavicle fractures include direct blows from objects to the clavicle (7%) and indirect trauma from falls onto an outstretched hand (6%) There is no correlation between the mechanism of injury and the fracture site (i.e., which third is involved).
Direct compression, or applying force directly to the shoulder, is the most common mechanism for clavicle failure, research has shown, contrary to the conventional belief that a fall onto an extended hand was the common mechanism.
Causes of Clavicle Fracture
Some typical reasons for a broken collarbone include the following:
- Falls look like reaching on an outstretched shoulder or arm.
- Sports injuries are defined as direct hits to the shoulder sustained on a field, rink, or court.
- Traffic accidents include collisions involving cars, bikes, and bicycles.
- Hard vaginal deliveries usually result in birth injuries.
Risk Factor
Children and teenagers are more likely than adults to have a broken collarbone. As one gets older, the risk drops. Then, in the elderly, it rises again as they age and lose bone strength.
Sign and Symptoms
A clavicle fracture can make it difficult and extremely painful to move your arms.
Other signs that point to a fracture include:
- Shoulder drooping both forward and downward
- Unable to raise the arm due to discomfort
- A grating feeling when you attempt to lift the arm
- A defect or swelling over the fracture
- Bruising, edema, and/or soreness surrounding the clavicle
- Discomfort that gets worse when you move your shoulder
- If you gently pinch the skin over the break, it might resemble a tent.
- A lump on the shoulder or close to it
- A noise made when moving the shoulder that is grinding or crackling
- Inflexibility or stiffness in the shoulder
Classification
The Allman classification system, which divided the clavicle into three groups based on location and was later revised by Neer (in which Group II was further classified into three types), is typically used to describe clavicle fractures.
Group I: The most common location, midshaft fractures, also referred to as middle-third fractures,
Group II: Fractures to the lateral or distal third. A normal, non-union at work.
Group III: Medial or proximal third fractures.
Craig’s classification was more specific for fractures of the lateral third, whereas Robinson’s classification was more specific for various fracture patterns in the middle third.
Types of Clavicle Fracture
1] Near the sternum (least common)
A clavicular fracture is a break in the bone that occurs directly below the chin. The term “clavicle” refers to the group of bones that connect your shoulder blades to the rest of your chest. They help to support your upper back and stabilize your shoulders. Its three components are your body, neck, and clavicle tip.
The body part of the clavicle bends backward as a person falls forward due to the impact force. Because of their attachment to the clavicle, the shoulder blades may also move outward due to the force of the collision. As a result, the clavicle tips may separate from the body and neck.
This kind of clavicle fracture happens near the base of the clavicle. A direct blow to the side of your chest, like being whacked by a baseball bat or falling off a bicycle, is what causes it.
Causes
The majority of clavicle fractures result from falls involving the hands or elbows. Additional potential reasons consist of:
- Falling off a bicycle
- Struck by a moving object
- Car Accident
- Taking a blow or a kick
- Being shot in the head
- Bitten by a dog
- Absorbing damage from a big object
- Obstructing
2] Around the AC joint (its second-most common)
The clavicle is the long, thin bone that connects the shoulder blade to the sternum. It helps stabilize the shoulder girdle and provides attachment points for many essential muscles. The clavicle is formed by the meeting point of the neck and the body. The body is shaped like an upside-down “U,” whereas the neck is more like the letter C.
The result of a bone fracture at one end is a clavicle fracture. People usually trip and fall onto their elbow or outstretched hand in this manner. If the fall is severe enough, the clavicle’s body part could break off. The neck and body of the clavicle split as a result.
This kind is caused by an impact that occurs directly above the shoulder joint. For example, a person falling on their back and hitting their shoulder can cause a clavicle fracture. Additionally, the force may climb the arm.
Causes
The most common way for this fracture to occur is from being struck forcefully by a hard object, like a rock, hammer, or baseball bat. Falling off a ladder or stairs is another frequent cause.
3] Between the AC joint and the sternum in the middle of the bone (most common)
A fracture to the clavicle occurs when the ends of the clavicle break apart. This could happen if you fall forward onto your hands and arms or backward onto your chest. A crack in the middle of the clavicle is called a midshaft fracture. A midshaft fracture is caused by the clavicle’s ends being pulled apart.
When the clavicle splits in two, this kind occurs. It happens when something strikes the shoulder area directly, but not hard enough to break the clavicle completely. Rather, the bone fractures.
Causes
Pulling apart both ends of the bones can result in midshaft fractures. They usually occur when someone trips and falls on their arm or chest. Other possible causes include car crashes, motorcycle accidents, bicycle accidents, and sports-related injuries.
Diagnosis
Physical Examination
People who have fractured their clavicle typically experience pain that is localized to the area of the fracture. The affected extremity is typically kept close to the body. Patients may report hearing a snapping or cracking sound at the scene of the injury. The most commonly reported mechanism is a fall onto the lateral shoulder. Some less common mechanisms are direct blows to the clavicle or fall onto an outstretched hand.
The patient may exhibit a palpable or visible deformity over the fracture site during a physical examination. Patients with middle-third clavicle fractures typically have their shoulders pulled downward because the latissimus dorsi and pectoralis major muscles affect the distal fragment. The sternocleidomastoid elevates the proximal fragment. There may be tenderness, ecchymoses, crepitus, or localized clavicle edema.
Tenting of the skin denotes a high risk of severe angulation or displacement of the fracture, which could result in an open fracture. A comprehensive neurovascular examination is necessary because the brachial plexus and subclavian vessels are located close to the clavicle. Underlying edema, discoloration, or decreased distal pulses are possible signs of subclavian vascular injury. Brachial plexus injuries may result in distal neurologic findings.
A further reason for a comprehensive lung examination is the possibility of lung apex damage in rare instances, which can result in hemothorax or pneumothorax. Dyspnea or diminished breath sounds may be a clinical sign. Palpate the surrounding ribs and scapula to look for any possible concurrent fractures of those bones.
Patients without a history of acute trauma may develop a stress fracture as a result of repetitive stress on the proximal clavicle from various activities.
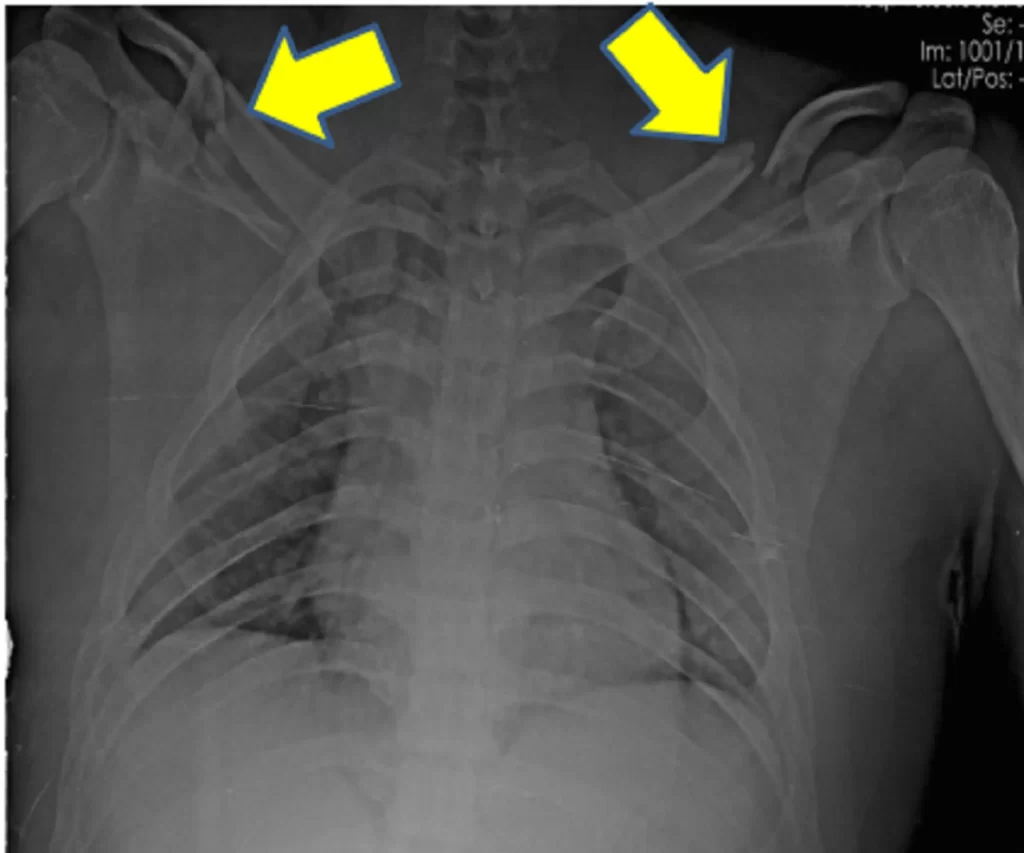
X-Rays
Standard anteroposterior clavicle radiographs should be obtained for each patient presenting with a clavicle injury. The evaluation of the degree of clavicle displacement is improved with a second 45-degree cephalic tilt view radiograph. Furthermore, the amount of overlap between the scapula and first rib is decreased by this additional view.
Images of dense structures, like bone, can be obtained using X-rays. Your physician will request an X-ray:
- To assist in determining the fracture’s location
- To find out more about how severe the break is
- To look for any further injuries, the doctor might also request an X-ray of your entire shoulder
CT-Scan
While most clavicle fractures are visible in these views, a CT scan may be necessary to guide treatment in the less common proximal or distal fractures to evaluate intra-articular involvement. A pneumothorax or rib injury should be clinically suspected, and this can be determined by taking an expiratory posteroanterior chest radiograph. If the neurovascular injury is a concern, arthrography, ultrasonography, and CT may be used to guide further management.
The first methods used to evaluate the proximal clavicular stress fractures are plain radiographic views and, if necessary, a CT scan. Further imaging may be required to rule out inflammation and neoplasia in patients exhibiting swelling in this area on radiography and in clinical assessments.
Different Diagnosis
A diagnosis can often be made based on the physical examination and medical history of the patient.
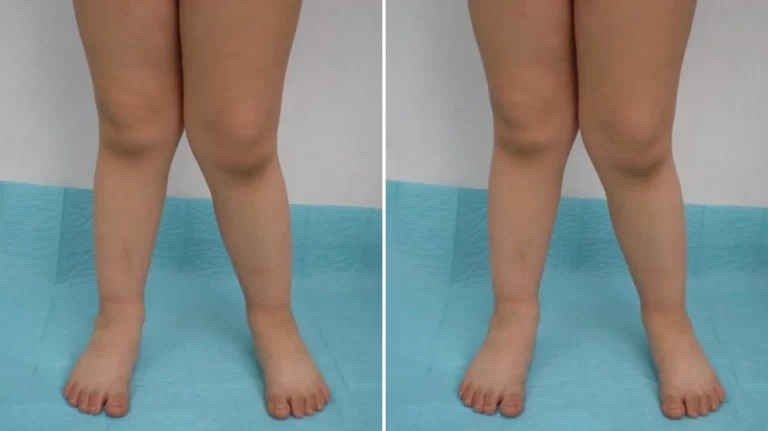
As differential diagnoses for a clavicle fracture, conditions such as rotator cuff injury, rib fracture, scapular fracture, shoulder dislocation, and sternoclavicular joint injury can be made.
Treatment of Clavicle Fracture
Depending on many variables, such as age, neurovascular compromises, the location (mid-shaft, distal, proximal), the type of fracture (displaced, undisplaced, comminuted), and whether the injury is open or closed, clavicle fractures are treated surgically or conservatively.
The conventional conservative management strategies for clavicle fractures have involved immobilization with a sling and subsequent rehabilitation. This still produces good results for undisplaced fractures, but for displaced mid-shaft clavicle fractures, conservative treatment results in longer recovery periods before returning to the sport, higher rates of re-injury, and suboptimal shoulder function because of clavicular mal-union and shortening, which causes thoracoscapular dyskinesia.
Similarly, it has been shown that athletes with displaced lateral fractures who receive conservative care have a high rate of non-union and subsequently impaired shoulder function.
Operative intervention is therefore recommended for fractures of the midshaft that are fully displaced, shortened by more than 2 cm, or comminuted, and is routinely performed for displaced lateral fractures in athletes.
Nonsurgical Treatment
If the fractured ends of the bones have not shifted too much out of place, you might not need surgery. Many broken clavicles heal without surgery.
The following are a few nonsurgical options:
- Arm support: Immediately following the break, a simple arm sling is usually used for comfort to keep your arm and shoulder in place while the injury heals.
- Medication: One kind of painkiller that can ease discomfort while the fracture heals is acetaminophen.
- Physical therapy: Although it will hurt, it’s important to keep your arms moving to prevent stiffness in the shoulders and elbows. Patients often begin doing elbow motion exercises as soon as possible after an injury.
A common consequence of a fractured clavicle is weakness in the arms and shoulders. Once the bone begins to heal, your pain will go down and your doctor might recommend some light shoulder exercises. These movements will assist in avoiding weakness and stiffness. Once the fracture has completely healed, you will progressively start doing more difficult exercises.
FOLLOW-UP CARE
Until your fracture heals, you must schedule frequent checkups with your physician. During these visits, the doctor will take X-rays to make sure the bone is healing in the right place. After the bone heals, you can gradually get back to your regular activities.
CAUSES
A clavicle fracture may occasionally move before healing. To make sure the bone stays in the right place, you must see your doctor as prescribed.
A fracture is referred to as nonunion if it does not heal.
In patients with a good range of motion and minimal pain, additional nonunion treatment may not be required.
In other situations, nonunion can cause excruciating pain and necessitate surgery.
When the fracture pieces do move and the bones heal in that alignment, it results in a malunion. Surgery might or might not be required for this, depending on how much your arm moves and how much the bones are misaligned.
A large lump may develop over the fracture site as it heals. Even though it usually gets smaller over time, a small bump often remains that way indefinitely.
Surgical Treatment
Your doctor may suggest surgery if the fractured ends of the bones have shifted significantly out of alignment.
Typically, surgery involves repositioning the broken bone pieces and preventing them from moving further until they mend. This can help strengthen your shoulders once you’ve healed.
Open reduction and Internal fixation
This is the most widely used technique for treating clavicle fractures. Reducing the bone fragments to their correct alignment is the first step in the procedure. The bone fragments are then fastened in place using special metal hardware.
Typical techniques for internal fixation consist of:
1] Plates and screws
Once realigned, the fractured bone fragments are held in place by special screws and metal plates attached to the outside of the bone.
A small patch of numb skin beneath the incision may become noticeable after surgery. This numbness will eventually become less noticeable. Since the clavicle is directly beneath the plate, you may feel it through your skin.
After the bone has healed, plates and screws are usually left in place unless they cause discomfort. Although hardware problems are uncommon, some patients claim that seatbelts and backpacks irritate the area around their collarbones. In this case, it is possible to remove the hardware before the fracture mends.
2] Pins or screws
Pins or screws can be used to hold the fracture in place after the bone ends have been replaced. Placing screws or pins typically requires fewer cuts than placing plates.
Because pins and screws often irritate the skin where they are inserted, they are usually removed once the fracture has healed.
Physiotherapy Management
Rehabilitation aims to improve and restore shoulder function for activities of daily living, employment, and sports. The first few weeks of the rehabilitation regimen could be a little different based on the main course of treatment (e.g., surgical vs. conservative).
Fracture healing may take longer with nonoperative treatment. Conservatively treated clavicular midshaft fractures usually heal 18 to 28 weeks after the injury. As a result, regular follow-ups are required to ascertain whether the fracture site has been appropriately unioned. As a result, the rehabilitation plan may also vary based on the co-morbidities of each individual.
The first few weeks (2-4 weeks) following an acute undisplaced fracture can be used to apply the POLICE principle, which is further covered below with clavicle fractures.
Precaution
A sling or figure-of-eight brace is used to immobilize the patient’s shoulder until the clinical union is completed. A figure-of-eight brace is widely thought to prevent or reduce secondary fracture shortening during the fracture healing period. However, it is linked to additional pain and discomfort, such as nerve compression that results in transient brachial plexus palsies and venous blood return restriction.
The study did not find any differences in the nonunion rate or healing time between these two clavicle fracture treatment modalities. As a result, it is usually recommended to immobilize the patient during internal rotation for two to four weeks while wearing a sling. Wear the sling during the day, excluding when you exercise, and take care of yourself. Whether or not they choose to wear it at night, patients need to use caution.
Whenever a patient coughs or sneezes violently, they run the risk of experiencing respiratory excursions that could move their clavicle. They can be taught coughing techniques with active assistance if needed.
Progression
It’s critical to learn about the bone healing stage to proceed with the optimum loading.
1] Bone healing from the injury day to a week later
There is no stability at the fracture site.
Inflammatory phase of the bone healing stage, with no callus visible on the radiograph.
2] Bone healing in the second week
Minimum amount of stability at the fracture site
Early reparative stage of bone healing, with some callus formation visible on the radiograph
1-2 weeks of therapy following an injury:
- Use of the previously described arm sling (necessitated most of the time).
- To prevent stiffening of the elbow and wrist, self-mobilization of the joint outside of the sling is necessary multiple times a day.
- It could hurt to raise your elbow higher than shoulder level.
- For the first one to two weeks, the range of motion for the shoulder should typically be restricted to pendulum exercises.
- Neck range of motion and proper posture are taught.
3] Bone healing three to six weeks after damage
Stability: The fracture site becomes stable as callus formation begins.
Stage of bone healing: On the radiograph, the fracture line and reparative stage are less noticeable.
3–6 weeks of therapy following an injury:
- Reduce the amount of time spent using arm slings in non-dependent positions.
- Start your regular, mild daily activities using your arm and shoulder.
- Shoulder active-assisted to active range of motion in a single plane with no more than 90 degrees is recommended within the first 6 weeks.
- Exercises for scapular mobilization are discussed.
- Within four to six weeks, one can begin shoulder isometric exercises with a moderate level of resistance.
- Don’t lift anything heavy for the entire six weeks.
- You can begin a gradual progression of cardiovascular endurance training with static cycling and brisk walking.
4] Bone healing six to eight weeks after damage
Fractures stabilize by then.
During the reparative stage of fracture healing, bridging callus is evident.
5] Eight weeks later
The fracture line becomes less noticeable as the remodeling phase starts.
6–12 weeks of therapy following an injury:
- After six weeks, shoulder range of motion in all planes—free, active, and assisted—is typically permitted, with passive ROM being tolerated.
- After six weeks, progressive resistive exercises (isotonic) are recommended for the rotator cuff, biceps, triceps, and scapular stabilizers.
- Avoid carrying any weight until a clinical fracture occurs.
- Sports and jobs requiring weight bearing and arm use are typically put on hold until the patient is pain-free and radiographs show no further fracture consolidation, which is usually six to twelve weeks later.
As the remodeling phase progresses, the fracture line becomes less obvious.
6–12 weeks of therapy after a trauma:
- Six weeks is usually the limit for shoulder range of motion in all planes (free, active, and assisted), with passive ROM being tolerated.
- It is advised to perform progressive resistive exercises (isotonic) for the rotator cuff, triceps, biceps, and scapular stabilizers after six weeks.
- Till a fracture manifests itself clinically, avoid bearing any weight.
- Weight-bearing activities and occupations involving the use of the arms are usually postponed until the patient is pain-free and radiographs demonstrate no additional fracture consolidation, which is typically six to twelve weeks later.
Rehabilitation After Postoperative Treatment
For middle third clavicle fractures, primary open reduction and internal fixation with a plate (locking compression plate) and screws allow for immediate post-operative mobilization and more rigid fixation. More rapid bone mending is achieved with surgical management compared to conservative care.
As a result, compared to conservative management, mobilization and strengthening exercises can be recommended earlier, and the period of immobilization is shorter. An earlier progression of the same exercise program can be suggested as a precautionary measure.
Complications
Most clavicles that break heal quickly. When issues are available, they might involve the following:
- Injury to a nerve or blood vessel: In rare cases, the sharp edges of a broken collarbone can cause damage to adjacent nerves and blood vessels. If you experience numbness or coldness in your arm or hand, get medical help right away.
- Poor or sluggish healing: A severely fractured collarbone may take a long time to heal. A shortened bone can result from poor bone-to-bone joining during healing.
- A lump in the bone: During the healing process, a bony lump develops where the bone joins itself. Due to its proximity to the skin, the lump is easily visible. Not all lumps go away with time; most do.
- Osteoarthritis: Fractures involving the joints connecting the breastbone or shoulder blade to the collarbone may raise the chance of arthritis developing in that joint later on.
Serious complications are uncommon in clavicle fractures. Injuries to the subclavian vessels or brachial plexus can happen during presentation or while the clavicle heals and forms a callus. Peripheral neuropathy may arise from compression of the brachial plexus caused by excessive callus formation.
Malunion, or the healing of a clavicle fracture with angulation, shortening, or an unattractive appearance, is the most frequent consequence of clavicle fractures. The majority of patients with clavicle fracture malunions have normal function and are not clinically significant. Neurologic or functional issues may arise from some malunions, particularly in cases where the shortening is more than 2 cm. Delay in surgical correction may be an option for patients whose malunion is causing them to experience ongoing pain, reduced range of motion, or decreased strength.
When a fracture does not heal in four to six months, it is called nonunion. The nonunion rate for all nonoperatively treated middle-third clavicle fractures is 6%; for displaced fractures, it rises to 15%. Distal third clavicle fractures have nonunion rates ranging from 28% to 44%. Advanced age, female gender, smoking, fracture comminution, significant displacement or shortening of the fracture, and insufficient immobilization are risk factors for nonunion.
Many clavicle fracture nonunion patients have no symptoms and don’t need any additional care. Some patients with a clavicle fracture who do not heal may experience persistent pain, limited range of motion, or functional loss. For additional surgical care, an orthopedic surgeon should be consulted for these patients.
Complications from proximal-third clavicle fractures include posttraumatic arthritis and nonunion. Acute pneumothorax, brachial plexus injury, and subclavian vessel injury are among the serious intrathoracic injuries that can arise from proximal clavicle fractures that are displaced inward. The highest incidence of nonunion occurs in fractures of the distal third of the clavicle; however, many of these patients have asymptomatic nonunions. A late consequence may be acromioclavicular joint degenerative arthritis.
Prognosis
The prognosis for clavicle fractures is generally good. Most clavicle fractures are treated conservatively, meaning surgery is not necessary. Patients are immobilized with a figure-of-eight brace or sling until the clinical union is achieved. This typically occurs in adults within 6 to 12 weeks and children within 3 to 6 weeks. Patients should work on strengthening and range-of-motion exercises under the guidance of physical therapists once immobilization is no longer necessary.
Six weeks following an injury, patients can typically return to their regular activities. After two to four months of rehabilitation, the athlete must demonstrate radiographic evidence of bony healing, no palpable discomfort, full range of motion, and normal shoulder strength before returning to full-contact sports.
Preventions
There are several ways to prevent a fracture of the clavicle:
- Use safety equipment when participating in risky activities such as sports.
- Avoid riding a motorcycle without a helmet.
- Never drive after consuming alcohol or drugs.
- Always use a seat belt.
- Be aware of dogs, especially if they bite.
- Avoid contact sports such as football, rugby, hockey, basketball, and soccer.
- Hold off on diving into the water.
- Avoid lifting large objects.
- Use safety gear when playing sports that involve hitting, throwing, or tackling.
- Always keep your head up when getting out of a car.
- When working with machinery, avoid distractions and stay focused.
- Stop descending in shallow waters.
Summary
The best approach to treating patients with clavicular fractures is to form a multidisciplinary team that includes an orthopedic surgeon, an emergency department physician, a primary care physician, a nurse practitioner, and a physical therapist.
Orthopedic consultation should be sought right away by patients who have neurovascular compromise, open fractures, skin tenting, or any break in the skin near the fracture.
Non-surgical management is the initial treatment option for fractures that are not displaced.
On the other hand, because surgical management offers better return rates and return times than conservative management, it is the preferred course of action for displaced mid-shaft fractures and the accepted treatment for displaced lateral fractures in athletes.
The fracture may heal in eight to twelve weeks, and most patients have positive outcomes. However, a small percentage of patients may have chronic pain and restricted shoulder range of motion.
It is safe to recommend an early mobilization rehab protocol in cases of acute or non-union post-operatively.
FAQs
How serious is a fractured clavicle?
A hospital stay is necessary when treating a broken clavicle. Typically, a sling is placed on your arm to aid in the healing of your clavicle. To help with pain, you will also be given painkillers. Surgery might be required to fix a severe break, but this is uncommon.
Do clavicle fractures need surgery?
A clavicle fracture is a painful break in the clavicle. The majority of people don’t require surgery, but some do to realign the fractured bone fragments. Recovery from physical therapy is essential to resume daily activities.
How can a fractured clavicle heal the quickest?
With ice, arm support, pain medication, and exercise, most broken collarbones heal. Either a shoulder immobilizer or a sling is used to support the arm. Similar to a sling, a shoulder immobilizer also has a strap that encircles the waist.
Is a broken clavicle painful?
It can be extremely painful and difficult to move your arm if you have a broken collarbone. A sling can be used to treat many clavicle fractures, keeping the arm and shoulder immobile until the fractured bone heals. However, in certain cases of clavicle fractures, the fracture causes the bone fragments to shift significantly.
How do you treat a fractured clavicle?
The majority of clavicle fractures are managed conservatively without surgery. Patients are kept immobile until the clinical union is accomplished by wearing a sling or figure-of-eight brace. For adults, this usually happens by 6 to 12 weeks, and for children, by 3 to 6 weeks.
Is a clavicle fracture life-threatening?
Although not fatal, a clavicle fracture can affect a patient’s function and quality of life. Short-term: discomfort, difficulty sleeping, and impairment. Long-term: to non-union or malunion, which may cause persistent pain and function loss.
References
- Clavicular Fracture. (n.d.). Physiopedia. https://www.physio-pedia.com/Clavicular_Fracture
- Clavicle Fracture (Broken Collarbone) – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/clavicle-fracture-broken-collarbone/
- Bentley, T. P. (2023, July 31). Clavicle Fractures. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK507892/
- Broken collarbone – Symptoms and causes – Mayo Clinic. (2022, December 10). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/broken-collarbone/symptoms-causes/syc-20370311
- UpToDate. (n.d.). UpToDate. https://www.uptodate.com/contents/clavicle-fractures#H22
- Clavicle Fractures. (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/clavicle-fractures#:~:text=The%20clavicle%20(collarbone)%20is%20one,physical%20examination%20and%20X%2Drays.
- Professional, C. C. M. (n.d.). Broken Collarbone (Clavicle Fracture). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16874-broken-collarbone-clavicle-fracture
- A. (2022, June 22). 3 Types of Clavicle Fracture: Causes, Symptoms, and Treatment. WOMS. https://worldofmedicalsaviours.com/clavicle-fracture/






One Comment