Coxa Plana
What is the Coxa Plana?
Coxa=hip bone plana=flat part
coxa plana are also known as Legg-Calvé-Perthes disease
coxa plana are flattening of the femoral head epiphysis and is associated with many skeletal disorders. as in Legg-CalvéIdiopathic osteonecrosis of the femoral epiphysis seen in children is referred to as Perthes disease. With growing, the acetabulum develops a secondary deformity.
Perthes are considered idiopathic conditions, and there are no apparent predisposing factors.
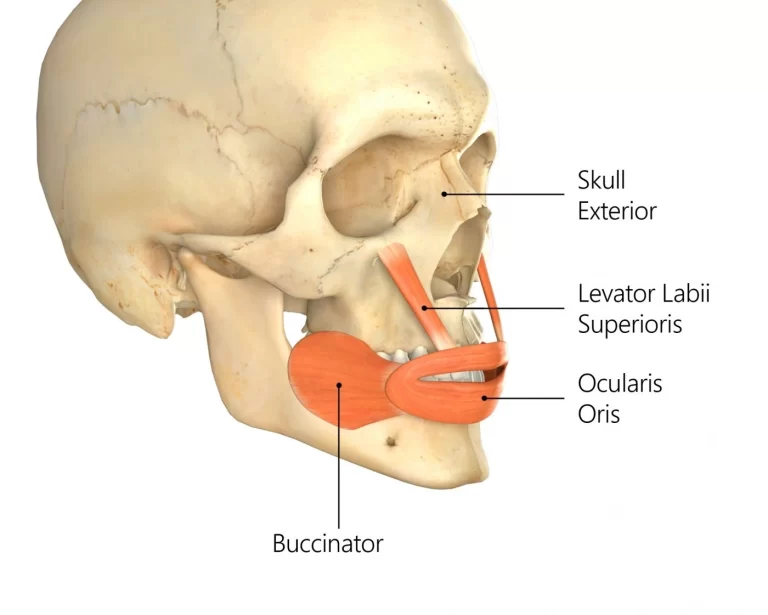
Anatomy of the Coxa Plana
Coxa planum is a disease of the before normal hip joint in which the bony nucleus of the femoral head becomes necrotic. The dead bone is slowly replaced by the normal stages of bone repair. During this process, there is usually some flattening of the generally spherical femoral head and deformity of the acetabulum.
Epidemiology
A kind of idiopathic osteonecrosis or osteochondrosis of the femoral head in children is known as Perthes’ disease. The epiphysis has avascular necrosis, which impairs the enchondral ossification of the femoral head.
Boys are impacted five times more frequently than girls. Compared to slipping upper femoral epiphysis (SUFE), presentation often occurs at a younger age, peaking at 5 to 6 years. mostly affects males between the ages of 5 and 12.
Presenting symptoms include pain and limping that normally affect only one hip but rarely both over a month.
Cause
There is no known cause of Legg-Calvé-Perthes disease( LCPD). It might be idiopathic or result from another etiology, such as trauma (macro or recurrent microtrauma), coagulopathy, or steroid usage, that would impair blood flow to the femoral epiphysis. About 50% of patients have thrombophilia, and up to 75% of patients should have coagulopathy.
A nutritional disruption of the upper femoral epiphysis caused by some interference with its circular sclerotic alterations in the femoral neck is the most prevalent kind of coxa plana. Sclerosis is the end outcome of an earlier joint inflammation.
It is diagnostic of exclusion for other osteonecrosis causes, such as Gaucher disease, leukemia, sickle cell disease, and corticosteroid usage.
Pathology
Uncertainty surrounds the precise etiology of osteonecrosis in Perthes disease. Osteonecrosis often develops as a result of an irregular or compromised blood supply to the femoral epiphysis, which causes bone loss, fragmentation, and ultimately the structural collapse of the femoral head. Bilateral osteonecrosis occurs in around 15% of cases.
Clinical symptoms:
Most children present with atraumatic hip pain or a limp. Some kids have a coincidental history of trauma. This may precipitate the exhibition of the realization of signs that had been long-standing.
Blood tests are typically normal in Perthes. It is necessary to be certain that there is no other reason for osteonecrosis (e.g. sickle cell disease) during the workup
Differential Diagnosis
The following conditions should be considered when making a differential diagnosis for LCPD: In a differential diagnosis, any illnesses that cause necrosis of the skull or those that resemble them are questioned:
- Slipped superior femoral epiphysis
- Osteomyelitis
- Secondary causes of osteonecrosis
- Dysplasia epiphyseal capitis femoris (Meyer dysplasia)
- Tumors
- Haemophilia
Juvenile Rheumatoid Arthritis : a chronic inflammatory disorder that occurs before the age of 16 and can occur in all races.
Outcome Measures
- Lower Extremity Functional Scale.
- Harris Hip Score
- Hip Disability and Osteoarthritis Outcome Score
Diagnosis:
History
Limp with sudden or gradual onset, frequently painless (1–3 months).
Depending on where the pain originates, it may be limited to the hip or relate to the knee, thigh, or abdomen.
The pain usually becomes worse with time and exercise.
There shouldn’t be any signs of systemic illness.
Physical examination
decreased hip abduction and internal rotation.
The anteromedial thigh and/or knee were the source of pain on rotation.
because of discomfort and inactivity, the thighs and buttocks atrophy.
Afebrile Difference in limb length
Gait Analysis
Acute analgesic gait: Short-stance phase brought on by discomfort in the weight-bearing leg.
Trendelenburg gait (chronic): During the swing phase, the pelvis tilts downward away from the injured hip
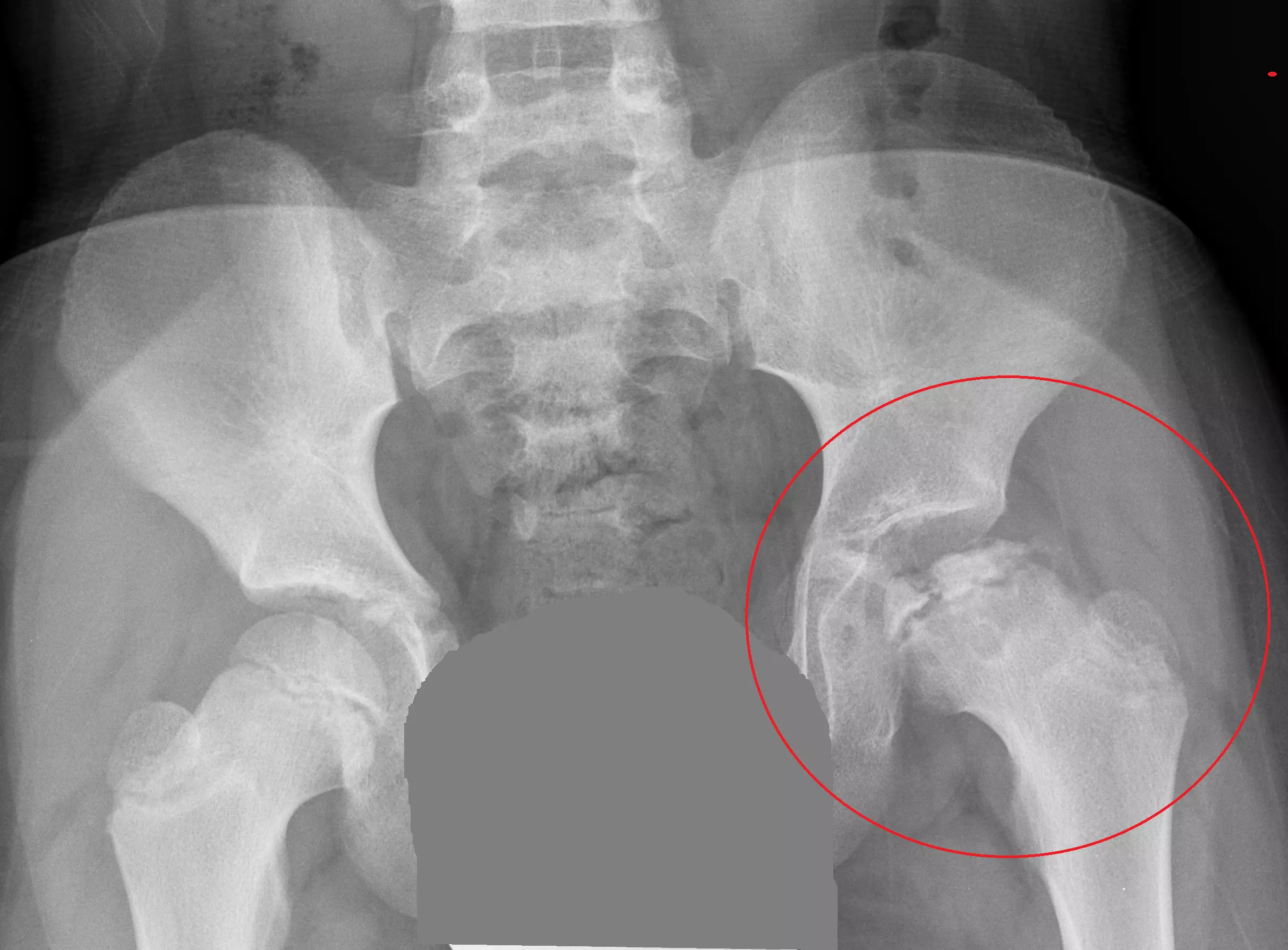
Radiographic features
A pelvic radiograph is the most effective first diagnostic for the diagnosis of Perthes. A tiny percentage of Perthes patients will have a normal radiograph, and any persistent symptoms may necessitate further imaging, such as an MRI.
MRI
MRI is gaining an increasing role in some scenarios:
early detection, prior to the appearance of x-ray findings
Evaluation of cartilaginous involvement is crucial for prognosis.
evaluating the congruence of the joints in a range of joint positions (needs an open magnet and dynamic imaging)
Dynamic MRI and arthrography both evaluate three key characteristics 3:
Femoral head deformity (also detected on static X-rays and MRI)
congruence: how closely the acetabulum’s and femoral head’s contours line up.
containment: the degree to which the femoral head’s flattened protrusion from the acetabulum is lateral subluxated.
The kids were often a little bit shorter at birth, and they stayed that way until they reached adulthood. The males were 4.4 cm shorter than the reference mean at maturity, and the girls were 2.5 cm shorter. When the patient was diagnosed, before puberty, and during puberty, the growth rate was normal.
A hip ultrasound will frequently be performed as part of the assessment of an atraumatic limp to check for effusion, however, osteonecrosis is unlikely to be detected by ultrasound.
The radiographic findings are those of osteonecrosis. There are separate systems for the stage of Perthes disease:
Catterall Classification
Based on the degree of head involvement
- Group I: Involvement of the anterior epiphysis
- Group II Involvement of the Anterior epiphysis with a main sequestrum
- Group III Only a small part of the epiphysis is not involved 1 more raw
The Herring classification, which is based on the lateral pillar, has the highest interobserver agreement. It is typically identified at the start of the fragmentation stage, roughly 6 months after the onset of symptoms. If the patient has not yet reached the fragmentation stage, it cannot be used accurately.
Group A: There are no density variations and the lateral pillar is fully elevated. The outlook for this group is continuously favorable.
Group B: The lateral pillar keeps at least 50% of its height. If the bone age is higher than 6, the outcome will be unfavorable.
Group C: < 50% of the height of the lateral pillar is maintained. Every patient will have a defective radiographic result. Giving predictive information is the purpose.
The lateral pillar’s height on the anterior-posterior ( AP) X-ray image serves as the basis for this classification.
Controlling symptoms is a key component of Perthes disease treatment, especially in the early stages of the condition. The femoral head becomes fragmented and destroyed as the condition worsens. Operative therapy may be necessary in this case to either ensure that the acetabulum covers the femoral head appropriately or to replace the femoral head in adulthood.
Plain radiograph
The degree of osteonecrosis and how long the blood supply has been altered determine the radiographic changes to the femoral epiphyses:
early: there may be no appreciable change
established: reduction in epiphysis size, lucency
late: fragmentation, destruction
The breadth of the femoral neck (coxa magna) widens as the modifications develop to improve weight-bearing support.
x-ray abnormalities and represent four temporal phases of the disease.
STAGE 1:early/ initial
Widening of the medial joint space due to joint effusion.
Femoral epiphyseal size asymmetry (affected side is smaller)
the apparent rise in femoral head epiphysis density blurring of the epiphyseal plate
radiolucency of the proximal metaphysis
STAGE 2: fragmentationn
Eventually, the femoral head begins to fragment,
with subchondral lucency (crescent sign)
the femoral head outline is difficult to make out
mottled density
thickened trabeculae
STAGE 3:repetative / re-ossification
re-ossification begins
the femoral head’s form becomes more clearly defined.
STAGE 4:heald/residual
The typical findings are:
flatting of the articular surface especially superiorly
the femur’s head and neck becoming wider.
the coxa plana, or femoral head, is widened and flattened (The thin sclerotic line crossing the femoral neck is known as the “sagging rope sign”).
Additionally, tongues of cartilage sometimes extend inferolateral into the femoral neck, creating lucencies, which must be distinguished from infection or neoplastic lesions. The chance of femoral neck deformity is increased by metaphyseal involvement, which also raises the likelihood of early epiphyseal closure and the associated leg length discrepancy.
Diagnostic Procedures
The diagnosis is typically confirmed by an MRI, but the location of the femoral head can also be determined with X-rays
Additionally, tongues of cartilage sometimes extend inferolateral into the femoral neck, creating lucencies, which must be distinguished from infection or neoplastic lesions.
An imaging method that can forecast the outcome at the earliest possible stage of the disease, before major deformity has developed, is preferable because the outcome of Legg-Calvé-Perthes disease (LCPD) is variable.
At the early stage of Legg-Calvé-Perthes disease (LCPD), the degree of femoral head involvement depicted by non-contrast and contrast MRI exhibited no association, indicating that they are evaluating two different components of the disease process. In the initial stage of Legg-Calvé-Perthes disease(LCPD), contrast MRI provided a clearer depiction of the area of involvement.
To quantify femoral head deformity in patients with Legg-Calvé-Perthes disease( LCPD) novel three-dimensional (3D) magnetic resonance imaging (MRI) reconstruction and volume-based analysis can be used. The femoral head deformity in LCPD has shown minor alterations (less than 10%), which can be accurately quantified using the 3D MRI volume ratio approach. This technique may be helpful in assessing how a treatment will affect the contour of the femoral head.
Arthrography
The femoral head and the acetabulum are typically assessed for congruence in a range of situations using arthrography under general anesthesia and traditional fluoroscopy. To stop pelvic irradiation, MRI is replacing this more and more frequently.
When severe, this may result in hinge abduction, in which the flattened femoral head ‘hinges’ on the lateral lip of the acetabulum, enlarging the medial joint space, rather than rotating and moving medially during hip abduction.
Treatment:
Controlling symptoms is a key component of Perthes disease treatment, especially in the early stages of the condition. The femoral head becomes fragmented and destroyed as the condition worsens. Operative therapy may be necessary in this case to either ensure that the acetabulum covers the femoral head appropriately or to replace the femoral head in adulthood.
The prognosis is better in males than in girls for the same age due to less maturity in boys than in girls 5,8, and the more benign disease course is anticipated the younger the age at the time of presentation. In youngsters with a skeletal age of 6 years or less at the time of disease start of 14 years, conservative treatment is beneficial.
Non-operative Therapy:
recommended for kids with lateral pillar involvement or bones less than 6 years old.
Until ossification is complete, activity limitation and protective weight-bearing are advised.
Physical treatment sessions with the patient are still possible.
The use of casts, braces, or orthotics is not recommended by the literature.
Physiotherapy Treatment:
In this patient population, physiotherapy therapies have been proven to enhance ROM and strength. Patients show better gains in their muscle mass, functional mobility, gait speed, and exercise performance quality.
Physiotherapy Goals
- Reduce pain
- Increase ROM
- Increase strength
- The patient will be independent with the proper aid and weight-bearing (WB) safety measures Improve balance
- Improved efficiency in walking
improve ROM (appendix 1 for exercise)
Static stretch for lower extremity musculature.
Dynamic ROM.
Perform an active range of motion and AAROM (active assistive range of motion) following passive stretching to maintain a newly increased range of movement
Improve strength:(appendix 2 for exercise)
Start with isometric exercise, then advance to isotonic exercise in a gravity-reduced position, and finally, advance to isotonic exercise against gravity. Both eccentric and concentric contractions are acceptable.
Start with two sets of 10 to 15 repetitions for each exercise, then work up to three sets for each exercise.
According to local opinion, one should also perform exercises to enhance balance, gait, and pain management.
In children with LCPD, the hip overloading pattern should be avoided. In children with LCPD, gait training to unload the hip may become a crucial part of conservative treatment.
In LCPD between the ages of 6 and 8 at commencement with Herring B involvement, non-surgical treatment using a brace is a trustworthy option to surgical treatment. However, they were unable to determine whether the positive outcomes were due to the brace or to the patients’ favorable prognoses.
Operative Treatment.
Femoral or Pelvic Osteotomy
Indicated in children over 8 years old.
Previous to the femoral head developing a deformity, surgery should be performed.
Valgus or Shelf OsteotomiesIndicated in children who have hinge abduction.
Results in improvements to the abductor mechanism
Hip Arthroscopy
a treatment option for mechanical symptoms and/or femoroacetabular impingement that is becoming more popular
Hip Arthrodiastasis
Considered a more controversial option.
In later life, hip replacements may be must required. and the rate of healing limits the amount of jumping and other impact activities that can be done.
Postoperative management
the following surgery, management
There is a description of the rehabilitation process that includes all of its stages.
Initial Phase (0-2 weeks post-cast removal):
The goals of the Initial Phase are:
Minimize pain(initial phase)
A hot pack is applied to relaxation and pain management with stretching.
Cryotherapy. Medication for pain.
Optimize ROM of hip, knee, and ankle.
Nonresistant static stretch A hot pack may be used, based on patient choice and comfort.
Dynamic ROM.
After passive stretching, do active ROM and Active assisted ROM to keep the newly acquired ROM.
Boost hip flexion, abduction, and extension as well as knee and ankle strength.
Start with hip-based isometric exercises, then go on to isotonic workouts in a gravity-relieving posture.
Start with knee and ankle isometric exercises, go on to isotonic workouts in a gravity-reduced posture, and then proceed to isotonic exercises against gravity.
Start with two sets of 10 to 15 repetitions for each exercise, building up to three sets for each.
Boost functional mobility and gait.
Follow the referring doctor guidelines for Weight bearing situations:
Transfer training and bed mobility to maximize independence with activities of daily living (ADLs).
Using the appropriate assistive equipment, practice your gait with an emphasis on independence and safety..
Improving skin integrity.
Scar massage and desensitization to minimize adhesions.
If possible in a home setting, a warm bath to promote skin integrity after the removal of the cast.
A warm whirlpool may be utilized if the patient is unable to utilize a warm bath for skin integrity management safely.
The frequency of physiotherapist supervision is two to three times per week (weekly).
Intermediate Phase (2-6 weeks post-cast removal)
Goals of the Intermediate Phase
Minimize pain (see ‘initial phase’)(appendix 1 exercise)
Optimise hip ROM in all directions while restoring normal knee and ankle ROM.
For exercises, see “initial phase”
Strengthen your knee and hip joints. (appendix 2 exercise)
hip isotonic workouts that begin with gravity-reduced postures and progress to positions against gravity.
Knee and ankle isotonic exercises should be performed in both low-gravity and anti-gravity situations.
Keep your freedom while moving about with functional mobility, keeping your WB status, and using the right assistive aids.
improving functional mobility and gait.
Observe the weight-bearing status recommendations provided by the referring doctor.
With the proper assistance device, continue your gait training with an emphasis on independence and safety.
Start out slowly, arms submerged, in the pool water that is chest-deep.
Skin Integrity Improvement.
Desensitization and massage for scars should continue.
The physiotherapist is observed two to three times each week (weekly). Due to WB status, it is advised that extracurricular activities be restricted at this period. If the recommending doctor approves, swimming is approved
Advanced Phase (6-12 weeks post-cast removal)
Goals:
Minimize pain (see ‘initial phase’).
increase ROM and flexibility in the knee, ankle, and hip.
Due to mechanical disadvantage, the knee and hip should be strengthened to at least 70% of the unaffected lower extremity, with the exception of the hip abductors, which should be strengthened to at least 60% of the unaffected lower extremity.
Concentric and eccentric contractions during isotonic hip, knee, and ankle workouts in situations with and without gravity.
Depending on the patient’s capabilities and the objectives of the therapy session, weight-bearing and non-weight-bearing (NWB) activities may be combined. Start doing functional, dynamic single-limb exercises supported by the upper extremity (such as step-ups and side steps).
Continue performing resistance-assisted double-limb closed chain exercises and, if your pulmonary function permits it, move to single-limb closed chain activities.
using a stationary bike while keeping the hip at a flexion angle of no more than 90 degrees.
Ambulation without the use of a tool or discomfort.
autonomously climb stairs utilizing a step-to-pattern while receiving upper extremity (UE) assistance.
The balance should be improved to at least 69% of the maximal Paediatric Balance Score (39/56) or to a single-limb stance on the side unaffected.
Improving gait and functional mobility.
The femoral head is deformed in Legg-Calve-Perthes disease, an idiopathic juvenile avascular necrosis.
It is recommended that activities outside of PT are limited to swimming if the referring physician allows it.
Note: Running and jumping activities are not allowed at this time.
appendix 1: ROM exercise
appendix 2:strengthening exercise prescription
appendix 3:guide to the level of evidence referenced in the guideline
Pre-Functional Phase :(12 weeks to 1+ year post-cast removal)
Goals:
Minimize pain(see ‘initial phase’)
The femoral head is malformed in Legg-Calve-Perthes disease, an idiopathic juvenile avascular necrosis.
Static stretch
Increase the strength of the hip abductors to at least 75% of the unaffected lower extremity due to mechanical setback, and the strength of the knee and hip, excluding hip abductors, to at least 80% of the unaffected lower extremity.
Arrange the steps individually, using a reciprocal pattern and support for the upper extremities.
Improve balance to 80% or greater of the maximum Pediatric Balance Score (at least 45/56) or single-limb stance of the uninvolved side.
a pain-free walking style with little impairments and typical effectiveness.
The frequency of physiotherapist supervision is 1-2 times per week (weekly).
In addition to physical therapy, swimming, and biking are advised as directed by the recommended doctor
Functional phase
Pain should be reduced to 1/100 or less (see “initial phase”).
Normalizing ROM: Rise ROM to 90% or greater of the uninvolved side for the hip, knee, and ankle, except for hip abduction, and Improvehip abduction ROM to 80% or greater due to possible bony block.
Strengthen the knee and hip, except the hip abductors, to 90% or more of the unaffected lower extremity. Due to mechanical limitations, the hip abductors must be strengthened to at least 85% of the unaffected lower limb.
Progress isotonic exercises of the hip, knee, and ankle and have concentric and eccentric contractions.
WB and NWB exercises are used in combination based on the patient’s capacity and the goals of the treatment session.
Practical dynamic single-limb activities (e.g. step-ups, side steps) with upper extremity aid as needed for patient safety.
Advancement of single-leg closed-chain exercises with resistance.
using a stationary bike while keeping the hip at a flexion angle of no more than 90 degrees.
Ambulation with typical efficiency and a non-painful limp.
freely negotiating stairs without UE help utilizing a reciprocal pattern.
Improve balance to 90% or greater of the highest score on the Pediatric Balance Scale (at least 51/56) or single-limb stance of the neutral side It is suggested that advance to the Functional Phase occur when the physician has decided there is sufficient re-ossification of the femoral head based on radiographs.
Recall that the advancement of the disease process
Prognosis:
The degree of original femoral head deformity, the proportion of the femoral head involved, and the subsequent secondary osteoarthritic alterations all affect prognosis. Children who have more than 50% of their femoral heads necrotic at the time of diagnosis ought to be managed surgically 14. Good femoroacetabular contact and a round femoral head are the goals of therapy.
Bracing may be utilized to treat milder forms of aberrant femoroacetabular malalignment, while more severe examples may require femoral neck and acetabular osteotomies.
Hip replacements may be required later in life.
The management of pain and symptoms, regaining the hip range of motion, and keeping the femoral head inside the acetabulum are all objectives of therapy.
The more benign the disease course is anticipated in patients who are younger at the time of presentation, and for patients who are the same age, males have a better prognosis than girls since boys are less mature. When a child’s skeletal age is 6 years or less when the condition first manifests itself, conservative therapy is preferred.
Conclusion
An idiopathic juvenile avascular necrosis called Legg-Calve-Perthes disease causes the femoral head to be malformed. The degree of osteonecrosis and the final form of the femoral head has a significant impact on the long-term result and course of treatment for this self-healing disorder. Females often fare worse than men, despite the fact that males are more likely to experience it. Older children also do worse than younger ones.
There is next to no practical evidence due to a lack of exploratory research and the treatments prescribed are mostly based on heuristic models.
Treatments commonly attempt to strengthen and improve the range of motion and strength as well as control pain.
FAQs
What kind of mobility is restricted by Perthes?
10% to 15% of kids with Perthes disease have bilateral hip involvement, generally not simultaneously but temporally staggered. An examination of the body often indicates a limping gait. Internal rotation and abduction are the two basic hip motions that are restricted.
What constitutes a Perthes disease risk factor?
The following are risk factors for Legg-Calve-Perthes disease: 10% familial (delayed bone age by roughly 2 years); Hip avascular necrosis affects up to 5% of people with HIV. The hereditary coagulopathies factor V Leiden and others
What is the most recent method of treating Perthes disease?
Osteotomies are the most popular surgical treatment used to treat Perthes disease. To maintain the femoral head firmly inside the acetabulum, an incision, and repositioning of the bone are necessary in this technique. Screws and plates that are used to maintain this alignment will be taken out after the illness has reached the healed stage.
What defines the coxa plana from the Magna?
Coxa breva: An early closure of the epiphysis that results in a short femoral neck and a tiny femoral head. expanded femoral head: coxa magna. Coxa plana, commonly known as Legg-Perthes disease, is a flat femoral head (osteochondrosis) of the capitular epiphysis of the femur.
Does Perthes disease have an effect on growth?
The kids were often a little bit shorter at birth, and they stayed that way until they reached adulthood. The males were 4.4 cm shorter than the reference mean at maturity, and the girls were 2.5 cm shorter. When the patient was diagnosed, before puberty, and during puberty, the growth rate was normal.