Cuneiform Fracture
Introduction
Cuneiform fractures are relatively uncommon, accounting for only 1-3% of all foot fractures. The cuneiform bones are three wedge-shaped tarsal bones located between the navicular and metatarsal bones in the midfoot. However, when they do occur, cuneiform fractures can be debilitating if not managed properly.
Cuneiform fractures are often the result of high-energy trauma such as falls from height, motor vehicle accidents, or crush injuries. Stress fractures of the cuneiforms can also occur due to repetitive overuse. On x-rays or CT scans, these fractures may appear as a clear break in the bone or just a subtle hairline crack.
Nondisplaced cuneiform fractures generally heal well with immobilization in a cast or walking boot. However, displaced fractures over 2 mm or those at high risk of displacement require surgical fixation with screws and/or plates to ensure proper realignment and stabilization for healing. Delayed treatment or inadequate reduction of cuneiform fractures heightens the risk of post-traumatic arthritis, chronic pain, and stiffness in the midfoot.
Anatomy of the Cuneiform Bones
The three cuneiform bones are the medial, intermediate, and lateral cuneiforms. They articulate proximally with the navicular bone and distally with the bases of the first, second, and third metatarsals.
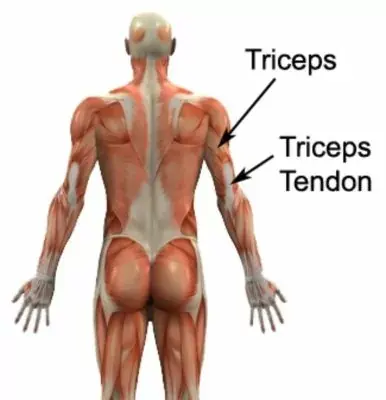
The medial cuneiform is the largest and most distal cuneiform bone. It serves as an attachment point for the tibialis anterior and tibialis posterior tendons on its distal surface. The lateral cuneiform is the smallest and most proximal. Its prominent dorsal surface provides leverage for the peroneus longus tendon. The intermediate cuneiform lies between the other two cuneiforms.
Each cuneiform bone has six surfaces for articulation with neighboring bones. The joints between the cuneiforms and navicular as well as the cuneiforms and metatarsals facilitate gliding motions to distribute forces across the midfoot. These Lisfranc joints are supported by strong interosseous ligaments on their dorsal and plantar sides.
Biomechanics
The wedge shapes and transverse arch alignment of the cuneiform bones play an important role in stabilizing the medial longitudinal arch. During weight bearing, the strong ligaments and intrinsic muscles spanning the midfoot prevent excessive flattening of the arch. Meanwhile, the narrower lateral column and second metatarsal are positioned lower to bear more weight.
Fractures or ligamentous injuries affecting the cuneiforms and Lisfranc joints can disrupt this intricate balance and stability. It is crucial to surgically restore anatomical alignment and mechanics with fixation across displaced fracture sites or joints. Even subtle residual displacement elevates plantar pressures and can lead to post-traumatic arthritis.
Types of cuneiform fractures
Stress or fatigue fractures of the cuneiform bones occur due to repetitive loading and stress. They are most commonly seen in the medial cuneiform bone and usually affect athletes and military recruits. On imaging, they appear as incomplete hairline cracks within the bone cortex. Treatment involves immobilization and activity modification to allow healing.
Avulsion Fractures
Avulsion fractures occur when a strong tendon or ligament pulls a fragment of bone away at its attachment site on the cuneiform. They often happen acutely with a sudden load while running or jumping. Surgical fixation may be needed if the fragment is displaced.
Oblique Fractures
Oblique fractures are diagonal breaks across the bone with displacement between the fracture fragments. They result from direct, crushing blows in high-energy traumas. Due to the instability, operative treatment with open reduction and internal fixation using screws is typically necessary.
Comminuted Fractures
In comminuted fractures, the cuneiform shatters into three or more pieces. Bone loss may occur. These severe, high-impact fractures require accurate reconstruction and fixation using plates, screws, and sometimes bone grafting for the defects.
Displaced Fractures
If a cuneiform fracture becomes significantly displaced, the alignment of the Lisfranc joint complex is altered. This impacts stability and weight distribution across the midfoot. Urgent reduction is vital to prevent long-term sequelae. Open reduction and internal fixation is often needed to maintain alignment while healing.
No matter the type, cuneiform fractures that are unstable or involve joints require anatomic realignment. Even gaps or step-offs over 2 mm can increase the risk of later arthritis and dysfunction. Proper diagnosis and treatment are key to optimizing outcomes.
Signs and Symptoms
- Pain – This is the most common symptom. Pain is located along the midfoot where the cuneiform bones are located. It is usually severe and worsens with standing, bearing weight, or pressing on the area.
- Swelling – There is often significant bruising and swelling over the midfoot. This develops rapidly after the injury. The swelling is often tense and may obscure the anatomical contours of the foot.
- Tenderness – Palpation over the cuneiform bones elicits marked tenderness. This suggests a cuneiform bone fracture rather than a sprain.
- Inability to Bear Weight – Standing or walking is difficult due to pain and instability, so patients often cannot bear weight on the affected foot.
- Deformity – In some cases, the foot appears misshapen or deformed after injury. There may be flattening of the arch due to bone displacement or dislocation of the neighboring joints.
- Bruising – Dark skin discoloration spreads from the midfoot and bases of the toes due to bleeding under the skin. This bruising may not appear until days after the initial injury.
Diagnosis
The diagnosis of a cuneiform fracture begins with a thorough history of the timing and mechanism of injury. Imaging tests are then used to confirm the diagnosis and guide treatment:
- X-rays – Initial standard foot x-rays including anteroposterior, lateral, and oblique views are obtained. Fractures may not be visible for 7-10 days when callus starts to form.
- CT Scan – Computed tomography provides detailed 3D images of bone anatomy to fully assess fractures and displacement.
- MRI – If ligaments around the cuneiform or Lisfranc joints are damaged, magnetic resonance imaging can depict associated soft tissue injuries.
It is critical to promptly diagnose and stabilize cuneiform fractures before displacement worsens. Even subtle fractures can cause lasting consequences if overlooked. Appropriate management relies on an accurate diagnosis via imaging and a complete assessment of the severity.
Treatment plans for cuneiform fractures:
Nonsurgical Treatment
- Cast Immobilization: For non-displaced or minimally displaced stable fractures, immobilization in a non-weight bearing short leg cast or walking boot for 6-8 weeks allows the bones to heal in proper alignment.
- RICE: Rest, ice, compression, and elevation help reduce pain and swelling in cases managed nonsurgically. Ice should be applied for 15-20 minutes several times per day along with compression wrapping and propped elevation.
- Restricted Weightbearing: Only touch-down weight is allowed for 6-10 weeks to prevent displacement while healing. Crutches or a knee scooter will be needed to avoid bearing full weight.
- Physical Therapy: Once the cast is removed and fractures show signs of the clinical union on x-rays, physical therapy starts to restore flexibility, proprioception, and strength, and normalize gait.
Surgical Treatment
Surgery is required for displaced, unstable fractures or those with concomitant Lisfranc ligamentous injuries:
- Open Reduction Internal Fixation: Realigning the bones anatomically is crucial. Fixation with screws and mini plates across fracture lines then maintains this reduction during healing.
- Lisfranc Fixation: Dislocations or fracture-subluxations across the tarsometatarsal (Lisfranc) joints also mandate surgical fixation using screws for 8-12 weeks.
- Bone Graft: Small fractures with missing bone pieces may require bone grafting to span defects and consolidate fractures.
Postoperative care involves strict non-weight bearing with crutches or knee scooters to not disrupt the fixation. Follow-up x-rays are taken periodically to verify maintained alignment while healing progresses for up to 3 months. Physical therapy then continues for 3-6 months restoring flexibility and strength.
The severity, location, and stability of the cuneiform fracture dictate the appropriate treatment for realigning the bones and supporting healing. Both nonsurgical and surgical options can result in excellent outcomes and return to full function if treatment principles are properly applied.
Complications
Delayed Union or Nonunion
If the fracture fails to heal properly within the expected timeframe (delayed union) or doesn’t heal at all (nonunion), further interventions are needed. This includes bone stimulation treatment, grafting, and revision surgery to stabilize the fragments.
Misalignment after a fracture or unreduced articular fractures where joint surfaces remain incongruous can lead to abnormal wear and tear. This causes post-traumatic arthritis to develop earlier, with stiffness, chronic pain, and loss of midfoot mobility.
Avascular Necrosis
The blood supply feeding the cuneiform bones may be disrupted by the injury. If blood flow isn’t restored, the bone tissue can die (avascular necrosis). This requires debridement and bone grafting to treat the resulting osteonecrosis lesion.
Malunion
If a cuneiform fracture heals in a shortened, rotated, or angulated position, it is considered a malunion. The abnormal position alters foot biomechanics and can increase pressure and arthritis in adjacent joints. Corrective osteotomy may be needed.
Infection
Despite antibiotics, open fractures or those requiring surgery have a higher risk of developing deep infections. This may need repeat debridement, intravenous antibiotics, and removal of fixation hardware to treat.
Complex Regional Pain Syndrome
Nerve injury or limb trauma can trigger complex regional pain syndrome, with out-of-proportion pain, swelling, skin changes, and stiffness during recovery. Physiotherapy and medications aim to control symptoms.
With prompt, appropriate treatment aligning any displaced bones, outcomes for cuneiform fractures are often excellent. However, complications can develop, some requiring more surgery. Follow-up care focuses on detecting any signs of complications to address them early.
Outcome and Prognosis
With appropriate management, most isolated, uncomplicated cuneiform fractures heal well without long-term functional impairments. Those at highest risk of complications include open injuries, fractures with significant comminution or articular involvement, and fractures with delayed treatment. Strict adherence to weight-bearing restrictions and rehabilitation is essential for optimal recovery.
The prognosis also depends on patient factors like smoking, diabetes, and osteoporosis which can delay healing. In general, nondisplaced stable fractures have over a 90% healing rate. Even displaced fractures have high union rates if properly reduced and immobilized early on. Full return to sports and activities is expected between 3-6 months with surgery and up to a year with nonsurgical treatment.
Rehabilitation Protocol
The initial rehabilitation goal is protecting the reduction and fracture site from displacement or nonunion. A period of strict non-weight-bearing, cast immobilization, elevation, and icing is followed by gradual weight-bearing, range of motion exercises, stretching, and muscular strengthening.
0-6 weeks: non-weight bearing in a cast or walking boot, frequent ice application, elevation
6-8 weeks: Weight-bearing to 25% body weight in the boot, active toe flexion/extension
8-12 weeks: Progress weight-bearing to 50% body weight, remove the boot for gentle ankle/foot range of motion
3-6 months: Restore full ankle dorsiflexion/plantarflexion and eversion/inversion; strengthen intrinsic and calves with resistance bands; gait training
6+ months: Sport-specific training and high-impact loading permitted once complete fracture healing is confirmed on CT or x-ray.
A graduated rehabilitation program based on fracture healing milestones optimizes function while still protecting the injury site. Most patients can expect to return to normal daily and recreational activities around the 6-month mark.
Key Factors Influencing Healing
- Anatomic reduction and rigid internal fixation for displaced articular or unstable injuries
- Early initiation of range of motion once initial healing occurs
- Controlled weight-bearing forces for solid bony union
- Patient compliance limiting activity before adequate healing
- Adequate bone quality and vascularity around fracture fragments
Tightly managing these critical factors can get cuneiform fracture patients back on their feet again safely, without limitations in motion or residual pain over long-term follow-up.
Preventing Cuneiform Fractures
As the cuneiform bones of the midfoot are vulnerable to high forces, prevention involves mitigating impact and overuse:
- Wear supportive shoes with adequate cushioning for athletic activities
- Gradually increase intensity when changing workout regimens
- Treat foot and ankle instability or arthritis that stresses the medial arch
- Tape or brace the foot during sports like running, basketball
- Stretch and strengthen foot and lower leg muscles for stabilization
- Take breaks when performing repetitive motions like jumping
- Maintain healthy bone density with calcium, Vitamin D
- Avoid smoking and steroid medications that weaken bone
While not all cuneiform fractures can be prevented, managing controllable risks can reduce injury rates.
Summary
- Causes: High-energy trauma like falls or crush injuries; stress reactions to overuse
- Symptoms: Midfoot pain and swelling, bruising, tenderness, inability to bear weight
- Types: Stress, avulsion, oblique, comminuted, displaced articular injuries
- Diagnosis: X-rays and CT scans show fracture alignment; MRI assesses soft tissues
- Nonsurgical Treatment: Cast, boot to stabilize simple fractures during healing
- Surgical Treatment: Open reduction and internal fixation of displaced, unstable fractures
- Rehabilitation: 6-12 weeks non/limited weight-bearing, then progressive strengthening
- Complications: Arthritis, nonunion, malunion, avascular necrosis, infection
- Outcomes: Most achieve union and return to full function by 3-6 months if treated early
- Prevention: Wear supportive footwear, strengthen muscles, manage risk factors
FAQs
What causes a cuneiform fracture?
Cuneiform fractures are usually caused by high-energy trauma from falls, motor vehicle accidents, or crush injuries. Stress fractures can also occur from repetitive overuse and loads on the midfoot.
What are the symptoms of a fractured cuneiform bone?
Symptoms include midfoot swelling, bruising, tenderness when touching the area, severe pain when bearing weight, and inability to walk on the injured foot. The top or medial side of the foot often appears deformed.
How are cuneiform fractures diagnosed?
These injuries are diagnosed with X-rays, CT scans, and sometimes MRIs. Imaging helps classify the fracture pattern, determine the amount of displacement, and assess soft tissue structures around the Lisfranc joint.
How are cuneiform fractures treated?
Nondisplaced stable fractures heal well in a cast or walking boot. Displaced or multiple fragmented fractures require surgery using plates and screws to realign and stabilize the bones. Strict non-weightbearing and therapy are crucial after treatment.
What is the recovery outlook for a fractured cuneiform?
With proper treatment and adherence to weight-bearing restrictions, full recovery takes around 3-6 months for nonsurgical patients and 6-12 months if surgery is performed. Most patients regain normal midfoot function without limitations.
REFERENCES
- McCormack, J. (2023, August 28). Cuneiform Fracture. James McCormack. https://james-mccormack.com/advice-centre/cuneiform-fracture/
- Bell, D. (2020, November 9). Medial cuneiform fracture. Radiopaedia.org. https://doi.org/10.53347/rid-83972
- Cuneiform fractures. (n.d.). https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/midfoot/cuneiform-fracture/definition




One Comment