Deep Vein Thrombosis (DVT)
What is a Deep Vein Thrombosis (DVT)?
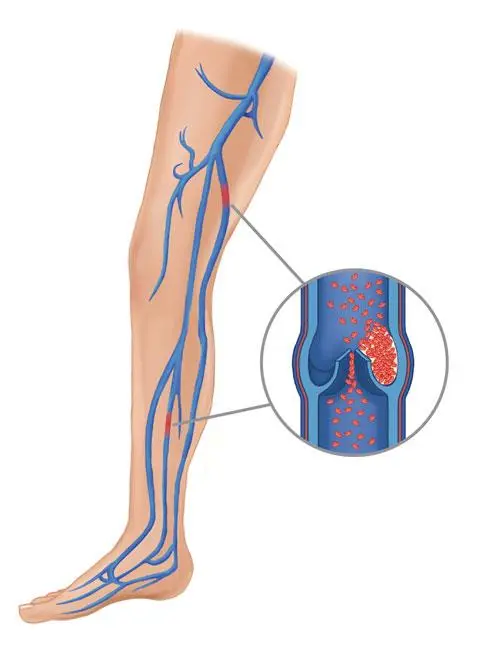
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in your body, usually in your legs. Deep vein thrombosis can cause leg pain or swelling but also can occur with no symptoms.
Deep vein thrombosis can be very serious because blood clots in your veins can break loose, travel through your bloodstream, and lodge in your lungs, blocking blood flow (pulmonary embolism).
Pathophysiology
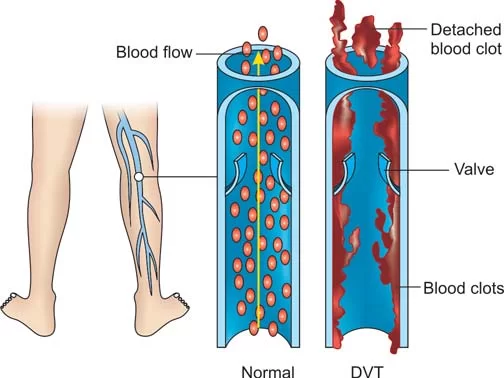
Lower-limb deep venous thrombosis (DVT) affects between 1% to 2% of hospitalized patients. These thrombi disrupt the vascular integrity of the lower limbs and are the source of emboli that
kill approximately 200,000 patients each year in the United States. The causes of thrombosis include vessel wall damage, stasis or low flow, and hypercoagulability. These factors favor clot formation by disrupting the balance of the opposing coagulative and fibrinolytic systems.
Symptoms
Deep vein thrombosis signs and symptoms can include:
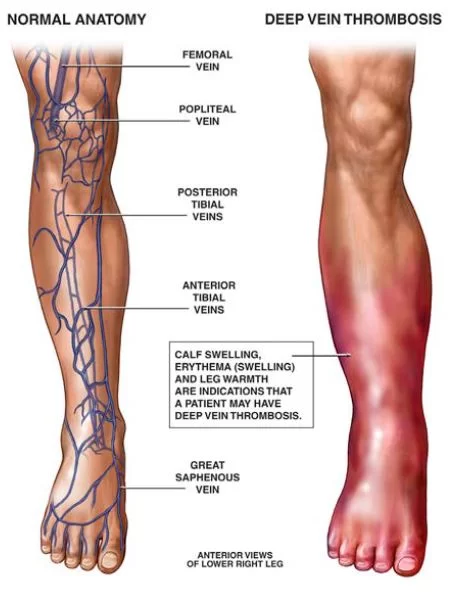
Swelling in the affected leg. Rarely, there’s swelling in both legs.
Pain in your leg. The pain often starts in your calf and can feel like cramping or soreness.
Red or discolored skin on the leg.
A feeling of warmth in the affected leg.
Deep vein thrombosis can occur without noticeable symptoms.
The warning signs and symptoms of a pulmonary embolism include:
Sudden shortness of breath
Chest pain or discomfort that worsens when you take a deep breath or when you cough
Feeling lightheaded or dizzy, or fainting
Rapid pulse
Coughing up blood
Causes
The blood clots of deep vein thrombosis can be caused by anything that prevents your blood from circulating or clotting normally, such as injury to a vein, surgery, certain medications, and limited movement.
Risk factors
Many factors can increase your risk of developing deep vein thrombosis (DVT). The more you have, the greater your risk of DVT. Risk factors include:
Inheriting a blood-clotting disorder. Some people inherit a disorder that makes their blood clot more easily. This condition on its own might not cause blood clots unless combined with one or more other risk factors.
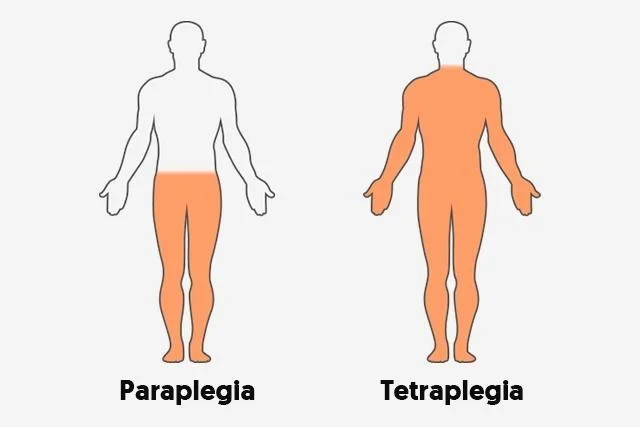
Prolonged bed rest, such as during a long hospital stay, or paralysis. When your legs remain still for long periods, your calf muscles don’t contract to help blood circulate, which can increase the risk of blood clots.
Injury or surgery. Injury to your veins or surgery can increase the risk of blood clots.
Pregnancy. Pregnancy increases the pressure in the veins in your pelvis and legs. Women with an inherited clotting disorder are especially at risk. The risk of blood clots from pregnancy can continue for up to six weeks after you have your baby.
Birth control pills (oral contraceptives) or hormone replacement therapy. Both can increase your blood’s ability to clot.
Being overweight or obese. Being overweight increases the pressure in the veins in your pelvis and legs.
Smoking. Smoking affects blood clotting and circulation, which can increase your risk of DVT.
Cancer. Some forms of cancer increase substances in your blood that cause your blood to clot. Some forms of cancer treatment also increase the risk of blood clots.
Heart failure. This increases your risk of DVT and pulmonary embolism. Because people with heart failure have limited heart and lung function, the symptoms caused by even a small pulmonary embolism are more noticeable.
Inflammatory bowel disease. Bowel diseases, such as Crohn’s disease or ulcerative colitis, increase the risk of DVT.
A personal or family history of deep vein thrombosis or pulmonary embolism. If you or someone in your family has had one or both of these, you might be at greater risk of developing a DVT.
Age. Being older than 60 increases your risk of DVT, though it can occur at any age.
Sitting for long periods of time, such as when driving or flying. When your legs remain still for hours, your calf muscles don’t contract, which normally helps blood circulate. Blood clots can form in the calves of your legs if your calf muscles don’t move for long periods.
Complications
Pulmonary embolism:
A serious complication associated with deep vein thrombosis is pulmonary embolism.
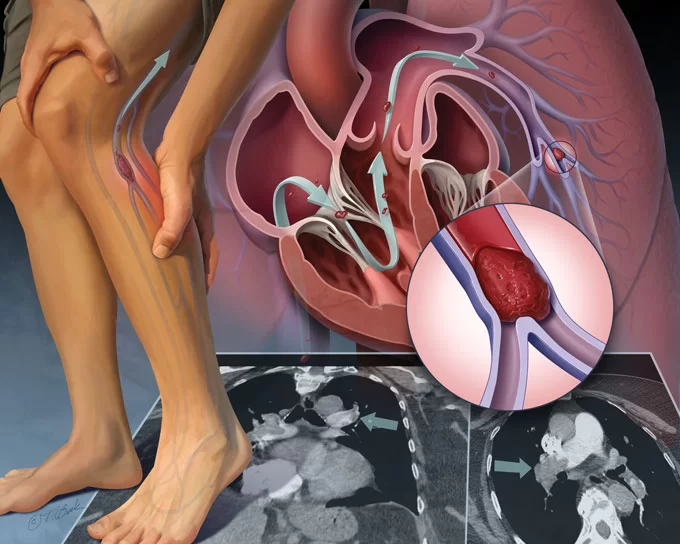
A pulmonary embolism occurs when a blood vessel in your lung becomes blocked by a blood clot (thrombus) that travels to your lung from another part of your body, usually your leg.
A pulmonary embolism can be life-threatening. It’s important to watch for signs and symptoms of a pulmonary embolism and seek medical attention if they occur. Signs and symptoms of a pulmonary embolism include:
Sudden shortness of breath
Chest pain or discomfort that worsens when you take a deep breath or when you cough
Feeling lightheaded or dizzy, or fainting
Rapid pulse
Coughing up blood
Postphlebitic syndrome
A common complication that can occur after deep vein thrombosis is known as postphlebitic syndrome, also called postthrombotic syndrome. Damage to your veins from the blood clot reduces blood flow in the affected areas, which can cause:
- Persistent swelling of your legs (edema)
- Leg pain
- Skin discoloration
- Skin sores
- Prevention
- Measures to prevent deep vein thrombosis include:
Avoid sitting still. If you have had surgery or have been on bed rest for other reasons, try to get moving as soon as possible. If you’re sitting for a while, don’t cross your legs, which can hamper blood flow. If you’re traveling a long distance by car, stop every hour or so and walk around.
If you’re on a plane, stand or walk occasionally. If you can’t do that, exercise your lower legs. Try raising and lowering your heels while keeping your toes on the floor, then raising your toes with your heels are on the floor.
Make lifestyle changes. Lose weight and quit smoking.
Exercise. Regular exercise lowers your risk of blood clots, which is especially important for people who sit a lot or travel frequently.
Diagnosis
To diagnose deep vein thrombosis, your doctor will ask you about your symptoms. You’ll also have a physical exam so that your doctor can check for areas of swelling, tenderness or discoloration on your skin. Depending on how likely you are to have a blood clot, your doctor might suggest tests, including:
Ultrasound. A wandlike device (transducer) placed over the part of your body where there’s a clot sends sound waves into the area. As the sound waves travel through your tissue and reflect back, a computer transforms the waves into a moving image on a video screen. A clot might be visible in the image.
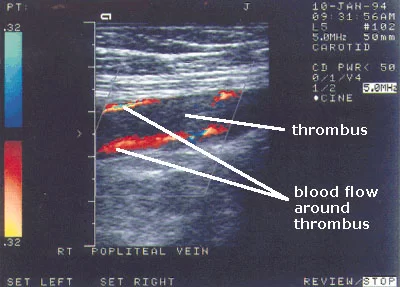
Sometimes a series of ultrasounds are done over several days to determine whether a blood clot is growing or to check for a new one.
Blood test. Almost all people who develop severe deep vein thrombosis have an elevated blood level of a substance called D dimer.
Venography. A dye is injected into a large vein in your foot or ankle. An X-ray creates an image of the veins in your legs and feet, to look for clots. However, less invasive methods of diagnosis, such as ultrasound, can usually confirm the diagnosis.
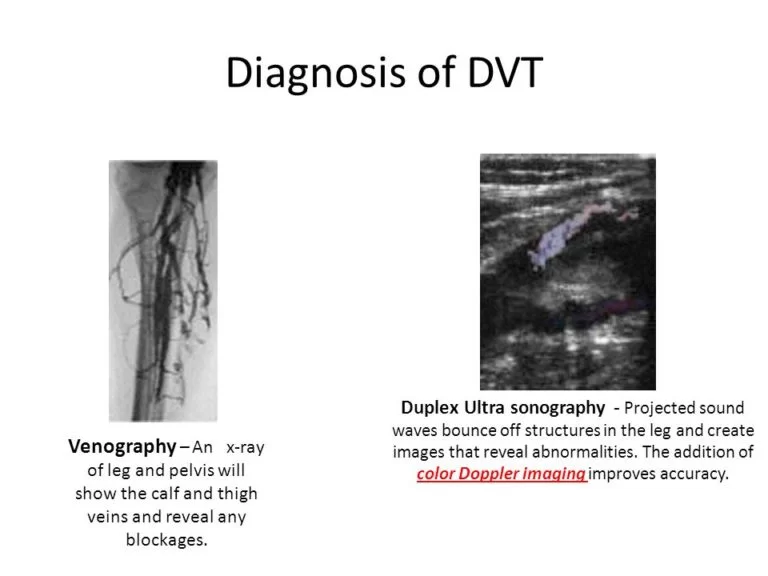
CT or MRI scans. Either can provide visual images of your veins and might show if you have a clot. Sometimes these scans performed for other reasons reveal a clot.
Treatment
Support stockings

Deep vein thrombosis (DVT) treatment is aimed at preventing the clot from getting bigger and preventing it from breaking loose and causing a pulmonary embolism. Then the goal becomes reducing your chances of deep vein thrombosis happening again.
Deep vein thrombosis treatment options include:
Blood thinners. Deep vein thrombosis is most commonly treated with anticoagulants, also called blood thinners. These drugs, which can be injected or taken as pills, decrease your blood’s ability to clot. They don’t break up existing blood clots, but they can prevent clots from getting bigger and reduce your risk of developing more clots.
The injectable medications can be given as a shot under the skin or by injection into your arm vein (intravenous).
Heparin is typically given intravenously. Other similar blood thinners, such as enoxaparin (Lovenox), dalteparin (Fragmin), or fondaparinux (Arixtra), are injected under the skin.
You might receive injectable blood thinner for a few days, after which pills such as warfarin (Coumadin, Jantoven) or dabigatran (Pradaxa) are started. Once warfarin has thinned your blood, the injectable blood thinners are stopped.
Other blood thinners can be given in pill form without the need for an injectable blood thinner. These include rivaroxaban (Xarelto), apixaban (Eliquis) or edoxaban (Savaysa).
You might need to take blood thinner pills for three months or longer. It’s important to take them exactly as your doctor instructs because taking too much or too little can cause serious side effects.
If you take warfarin, you’ll need periodic blood tests to check how long it takes your blood to clot. Pregnant women shouldn’t take certain blood-thinning medications.
Clot busters. If you have a more serious type of deep vein thrombosis or pulmonary embolism, or if other medications aren’t working, your doctor might prescribe drugs that break up clots quickly, called clot busters or thrombolytics.
These drugs are either given through an IV line to break up blood clots or through a catheter placed directly into the clot. These drugs can cause serious bleeding, so they’re generally reserved for severe cases of blood clots.
Filters. If you can’t take medicines to thin your blood, you might have a filter inserted into a large vein — the vena cava — in your abdomen. A vena cava filter prevents clots that break loose from lodging in your lungs.
Compression stockings. To help prevent swelling associated with deep vein thrombosis, these are worn on your legs from your feet to about the level of your knees.
Self-care
Use these suggestions to manage DVT after therapy to avoid problems or more blood clots:
- Inquire about your eating habits. Brussels sprouts, spinach, kale, and other leafy greens are foods strong in vitamin K that may interact with the blood thinner warfarin.
Adhere to the directions on medicine. You will learn how long you require treatment from your healthcare professional. You will require routine blood tests to monitor your blood clotting ability if you are taking specific blood thinners. - Keep an eye out for severe bleeding. Blood thinners may cause side effects like this. What are the warning signs? Ask your healthcare provider. Be aware of what to do in case of bleeding. Inquire with your provider about any activity limitations as well. If you use blood thinners, minor cuts or bruises could worsen into more serious injuries.
- Make a move. The sooner you start moving after surgery or for other reasons that have kept you bedridden, the less likely it is that blood clots will form.
- Put on supportive stockings. If your physician advises wearing them, wear them to help avoid blood clots in the lower legs.
What is the incidence of deep vein thrombosis?
In the US, pulmonary embolism (PE) accounts for 1 to 3 out of every 1,000 adult cases, and up to 300,000 deaths are related to PE/DVT each year. After heart attacks and strokes, it ranks as the third most prevalent vascular disease. Although acute DVT/PE can happen to anyone at any age, it is more common in adults over 60 and less common in children and adolescents. Over 50% of DVTs occur as a consequence of hospitalization for a medical condition or after surgery.
DVTs are more common during a hospital stay since you’re not as mobile as you usually are and instead spend more time lying in bed. DVTs are more likely during a hospital stay since you spend most of your time resting in bed rather than moving around as you typically would.
How can I Prevent DVT?
Following a DVT, you must lower the chance of developing another DVT or PE clot by:
- Following your doctor’s instructions to the letter when taking your prescriptions.
- Maintaining your follow-up consultations with the laboratory and your physician. These inform your doctor on the efficacy of your treatment.
- lifestyle changes: modifying one’s lifestyle to include things like eating better, exercising more, and abstaining from tobacco products.
If you are at a higher risk of acquiring a DVT even though you have never had one, make sure to:
- If you must spend a lot of time sitting stationary, work out your calf muscles. If your flight is long, get up and move around every 30 minutes at the very least. Or, if you’re on a long road trip, get out of the vehicle every 60 minutes.
- As soon as you are well or have had surgery, get out of bed and move around. The earlier you start moving around, the lower your risk of DVT development.
- To lower your chance of a clot, take medication or, if your specialist recommends them, use compression stockings following surgery.
- To lower your chance of a clot, do as instructed by your provider and heed their advice.
Prognosis
Since a DVT can take months or even years to dissolve, you will need to continue taking blood thinners as directed and wearing compression stockings until your doctor instructs you to stop. To ensure that you are taking blood thinners at the recommended dosage, you might require blood testing. Subsequent ultrasounds may be recommended by your provider to see whether your blood clot is remaining in the same location, getting better, or growing larger.
Conclusion
You are not the only one who suffers from deep vein thrombosis. At least a million Americans receive one each year. Numerous therapies may be beneficial, and your physician can tailor your care to meet your specific needs. Make sure you attend all of your follow-up appointments if they prescribe blood thinners so you can be sure you’re receiving the recommended dosage.
FAQs
What are the warning signs of deep vein thrombosis?
Warning signs of Deep Vein Thrombosis are:
Intense aching in the affected area, along with pain, swelling, and soreness in one of your legs—typically your thigh or calf.
skin that is heated around the clot.
red skin, especially below the knee on the back of your leg.
What is the main cause of deep vein thrombosis?
Main causes of deep vein thrombosis are:
Becoming sedentary as a result of prolonged bed rest or stationary sitting, such as when travelling. A family history of haemorrhage. possessing an implanted catheter, or long-term tube in a blood artery.
Is a DVT life-threatening?
Large clots can be deadly because they obstruct blood flow to the lungs. Furthermore, a long-term consequence known as post-thrombotic syndrome (PTS) affects one-third to half of DVT patients due to the harm the clot causes to the vein’s valves.
How is deep vein thrombosis cured?
DVT thrombolysis is a minimally invasive therapy that is frequently used to quickly relieve symptoms and remove big clots from deep veins in patients with symptomatic acute DVT. A tiny catheter is inserted into the leg during DVT thrombolysis under the supervision of an x-ray and ultrasound.
How can I test for DVT at home?
Squeeze the calf after having a friend or family member elevate the outstretched leg to a 10-degree angle. Deep calf discomfort may be a sign of deep vein thrombosis (DVT).
Can thrombosis go away by itself?
A blood clot develops in one of the deeper, bigger veins that pass through the muscles when someone has deep vein thrombosis (DVT). Lower leg deep vein thrombosis is the most common location. It usually disappears on its own and goes unnoticed. However, it could result in discomfort and edoema as symptoms.
Who is at high risk of DVT?
Conditions that raise the risk of DVT include cancer, heart disease, lung illness, and several autoimmune diseases (such lupus or inflammatory bowel disease).




19 Comments