Diabetic Nerve Pain
Introduction
Diabetic nerve pain, also known as diabetic neuropathy, is a common complication of diabetes mellitus that affects the nerves throughout the body. It arises when prolonged high levels of blood sugar associated with diabetes damage the peripheral nerves.
These nerves play a crucial role in transmitting signals between the central nervous system and various parts of the body, such as the extremities, digestive system, and organs.
Diabetic neuropathy is a condition in which the body’s nerves are destroyed as a result of high blood sugar levels caused by diabetes. This disease can develop in diabetics over time. Common symptoms include tingling discomfort, numbness, and loss of sensation, particularly in the hands, arms, feet, and legs.
Diabetic neuropathy is the breakdown and injury of peripheral nerves in diabetics. The characteristic of neuropathies is a progressive loss of nerve fiber function. A prevalent outcome of diabetes mellitus (DM) is diabetic neuropathy, which is thought to impact up to 51% of individuals with type 1 and type 2 DM.
Diabetic neuropathy can appear clinically as mild neuropathic pain and numbness or as asymptomatic. Diabetes-related neuropathy raises the risk of lower limb amputation, foot ulceration, and death.
Nerve problems can affect any organ, including the heart, digestive system, and sexual organs. Neuropathies of different kinds occur in around 60% to 70% of all diabetics, particularly those who have had the disease for more than 25 years. Consistent blood sugar management and a healthy lifestyle, however, can typically avoid or reduce the progression of diabetic neuropathy.
Anatomy with Clinical Importance
The peripheral nervous system refers to the portions of the nervous system outside of the brain and spinal cord. Smaller peripheral nerves are formed by the nerve roots when they arise from the spinal cord. There are motor and sensory fibers that make up the peripheral nerves.
The kind, degree, and distribution of these receptors, nerve fibers, or neurons are all degenerate in diabetic neuropathy. The degeneration starts symmetrically and distally and spreads proximally.
What Does Diabetic Nerve Pain Feel Like?
Diabetics express their nerve discomfort as tingling or burning in their hands, feet, legs, or arms. Sharp pain or cramps are often accompanied by numbness, muscle weakness, difficulty with coordination, and high sensitivity to touch. They may develop sores, blisters, and foot deformities such as hammertoe.
Mechanism of Injury / Pathological Process
Diabetic neuropathy’s pathogenic mechanism is unclear and most likely involves multiple factors. Microvascular disease, hyperglycemia, and cholesterol may be the cause of neuronal inflammation, oxidative stress, mitochondrial malfunction, and cell death, according to research.
Arrangement
The following is a typical diabetic neuropathy staging scale:
- N0: Neuropathy-free.
- N1a: Neuropathy-related signs but no symptoms.
- N2a: Patient able to heel walk; sensory, motor, or autonomic problems; moderate diabetic polyneuropathy.
- N2b: The patient has severe symptomatic diabetic polyneuropathy and is unable to walk on her heels.
- N3: Diabetic polyneuropathy: Disabling.
Classification
Four subgroups of diabetic neuropathy can be differentiated:
- Proximal neuropathy/ diabetic amyotrophy.
- Diabetic nerve discomfort, distal polyneuropathy, and peripheral neuropathy.
- autonomic neuropathy.
- Mononeuropathy and focal neuropathy
What causes Diabetic Nerve Pain?
Increased blood sugar levels cause diabetes-related nerve discomfort over time. It’s unclear what causes diabetic nerve discomfort, however specific findings point to many problems, including:
- Hyperglycemia. Because this type of nerve pain is caused by high blood sugar levels, a condition such as hyperglycemia, which generates higher blood sugar, may affect nerve transmission impulses, resulting in chronic discomfort.
- Inflammation. Diabetes is often accompanied by chronic inflammation. Over time, it can damage nerves and damage their capacity to carry signals, causing neuropathic pain.
- Poor blood circulation. High blood pressure reduces blood supply to the nerves. This decrease in blood supply can harm nerves and increase chronic pain.
- Autoimmune diseases. Different immune system problems can allow the body to accidentally target nerves, resulting in long-term harm. Damage to the nerves affects the normal flow of pain signals, resulting in chronic pain.
- Genetics. According to some studies, hereditary factors may play a role in the development of diabetic nerve pain, causing certain people more sensitive to it.
- Lifestyle. Unhealthy lifestyle choices can increase blood pressure and contribute to diabetic nerve pain. These habits include smoking, excessive alcohol intake, poor exercise levels, obesity, and an unhealthy diet.
Symptoms of Diabetic Nerve Pain
In almost 50% of the cases, distal symmetric polyneuropathy is present. The remainder is accounted for by asymmetrical or localized disorders, such as cranial neuropathies, radiculopathies/plexopathies, and carpal tunnel syndrome (14–30%).
The most typical signs and symptoms are:
- Hand or foot numbness, frequently on both sides, characterized by a distribution of stockings and gloves
- Foot pain that feels like burning, tingling, or “pins and needles”
- discomfort in the legs, feet, or hands
- Calluses or dry, cracked skin on the foot.
- weakness in the proximal, distal, or more focal areas, such as frequent tripping or foot drop
There are four major forms of diabetic neuropathy. One or more neuropathy kinds may be present in you.
Your symptoms will vary depending on the type and nerves affected. Typically, symptoms emerge gradually. You may not realize anything is wrong until significant nerve damage has happened.
1. Peripheral neuropathy.
This form of neuropathy may also be known as distal symmetric peripheral neuropathy. This is the most prevalent kind of diabetic neuropathy. It first affects the hands and arms, then the feet and legs. Signs and symptoms of peripheral neuropathy are frequently severe at night, and may include:
- Numbness or a decreased ability to sense pain or changes in temperature.
- Tingling or burning sensation.
- Sharp pains or cramps.
- Muscular weakness.
- Extreme sensitivity to touch—for some people, even the weight of a bedsheet can be uncomfortable.
- Ulcers, infections, and bone and joint damage are all serious foot disorders.
2. Autonomic neuropathy.
The autonomic nerve system regulates blood pressure, heart rate, sweating, vision, bladder function, digestion, and sexual organs. Diabetes can disrupt nerves in any of these regions, which may cause signs and symptoms such as:
- Hypoglycemia unawareness is the absence of knowledge regarding low blood sugar levels.
- Blood pressure drops after rising from sitting or lying down, which can produce dizziness or fainting (orthostatic hypotension).
- Bladder or bowel issues.
- Slow stomach emptying (gastroparesis) causes nausea, vomiting, feelings of fullness, and loss of appetite.
- Swallowing is difficult.
- Changes in how the eyes adjust from light to dark, or from far to near.
- Sweating can be increased or decreased.
- Sexual response issues include vaginal dryness in women and erectile dysfunction in men.
What you should do: You may need to eat smaller meals and take medicine to manage the condition.
In blood vessels:
Symptoms include:
- Blacking out when you stand up rapidly.
- A faster heartbeat
- Dizziness
- Low blood pressure.
- Nausea
- Vomiting
- Feeling full sooner than usual.
If you have it, avoid standing up too rapidly. You may also need to wear special stockings (see your doctor about them) and take medication.
In Men:
Symptoms may include an inability to achieve or maintain an erection, as well as “dry” or decreased ejaculations.
What you should do: Consult your doctor, as there are other probable causes besides diabetes. Treatment includes:
- Treatment options include counseling, genital implants or injections, vacuum erection devices, and medication for women.
- Symptoms include reduced vaginal lubrication and fewer or no orgasms.
What you should do: Visit your doctor. Treatments include:
- Treatment options include vaginal estrogen creams, suppositories, and rings, as well as medications to reduce pain during sex.
- Lubricants for the urinary system:
Symptoms include:
- Have trouble emptying your bladder.
- Symptoms include bloating and urinary incontinence.
- More bathroom trips at night.
- What you should do is tell your doctor. Treatments can include:
- Medication
- Self-catheterization involves inserting a catheter into one’s bladder to release pee.
- Surgery
3. Diabetic polyradiculopathy (proximal neuropathy)
This form of neuropathy typically affects nerves in the thighs, hips, buttocks, and legs. It can also affect the abdomen and chest areas. Symptoms normally appear on one side of the body but can progress to the other. Proximal neuropathy can include:
- Serious pain in the buttock, hip, or thigh.
- The thigh muscles are weak and decreasing.
- Difficulty rising from a seated position.
- Chest or abdominal wall pain.
4. Mononeuropathy (Focal Neuropathy)
Mononeuropathy is defined as an injury to a single, unique nerve. The nerve could be in the face, torso, arm, or leg. Mononeuropathy could lead to:
- Difficulty focusing or double vision
- Paralysis of one side of the face
- Weakness in the hand might lead to dropping things.
- Pain in your shin or foot
- Weakness leading to trouble elevating the front half of the foot (foot drop)
- Pain in the front of the thigh
What you should do is tell your doctor about your problems. Focal neuropathy is painful and unexpected. However, it usually improves on its own for several weeks or months. It often does not create long-term damage.
Other Diabetes Nerve Damage.
Diabetics may also develop other nerve-related diseases, such as nerve compressions (entrapment syndromes).
Carpal tunnel syndrome is a common form of entrapment syndrome. It produces numbness and tingling in the hands, as well as muscle weakness or pain.
If you suspect you have a nerve problem, consult your doctor to determine the cause.
There is no cure for diabetic nerve pain, but there are therapies that can help relieve symptoms and prevent additional damage.
This includes:
- Tight blood sugar control: This is the most important phase in treating diabetic nerve pain. Maintaining blood sugar levels as near to normal as possible will help prevent more nerve damage.
- Scrambler therapy uses a modest electrical current to activate the nephron and relieve pain.
- Spinal cord stimulation devices use moderate electrical pulses to inhibit pain signals from reaching the brain.
- Plasma exchange: This therapy removes harmful chemicals from the blood.
- Surgery: In some circumstances, surgery may be required to remove dead or dying tissue or repair foot abnormalities.
What are the main symptoms of diabetic neuropathy?
If you suspect that you or a loved one has diabetic neuropathy, evaluate the following significant symptoms:
- Numbness and decreased ability to sense pain
- A tingling or burning feeling
- Sharp aches or cramps?
- Muscle weakness.
- Extreme sensitivity to touch.
If one or more of these symptoms are present, consult your primary care physician for a proper diagnosis. It is important to diagnose diabetic neuropathy early on so that treatment can begin before the symptoms increase.
Patients frequently talk about burning, tingling, and numbness in their feet, but it is not uncommon to experience symptoms in their hands as well. As podiatrists, we primarily treat diseases affecting the lower extremities, specifically the feet and legs. This technique can be quite risky because patients frequently lose sensation in their feet, particularly the soles, increasing the chance of unintentionally causing major harm.
Consider the individual walking on a hot pool of Chattahoochee or stepping on sharp affected things such as glass or nails and being unable to feel the searing hot Chattahoochee or pain from a puncture. These events can be disastrous, resulting in numerous doctor visits, hospitalization with intravenous antibiotics, and possibly surgery to remove infected tissue and bone (and, in some cases, limb loss)If the condition improves and the patient’s circulation becomes restricted.
Diagnosis
Diabetic neuropathy is frequently diagnosed by a physician through a physical examination and a thorough evaluation of your medical history and symptoms.
Usually, your healthcare provider looks at your:
- Overall tone and strength of the muscles
- Tendon responses
- Touch, pain, temperature, and vibration sensitivity
Your healthcare provider can perform or recommend specific tests in addition to the physical examination to aid in the diagnosis of diabetic neuropathy, including:
- Testing of filaments. To measure your sensitivity to touch, patches of your skin are brushed with a soft nylon fiber (monofilament).
- Sensory evaluation. This non-invasive test determines how your nerves react to temperature fluctuations and vibration.
- Testing for nerve conduction. The speed at which electrical signals are conducted by the nerves in your arms and legs is measured by this test.
- Electromyography. A test known as needle testing is frequently performed in conjunction with examinations of nerve conduction. Your muscles’ electrical discharges are measured by it.
- Testing using autonomic processes. To find out whether your sweating falls within the normal range and how your blood pressure fluctuates while you are in different situations, you may undergo special testing.
Your doctor will do a thorough examination to determine the prevalence and severity of DPN in your case. To test your level of sensation, a Semmes-Weinstein probe (a soft fine nylon thread) is inserted into locations on the ball of your foot. If everything is okay, you should be able to feel the filament’s pressure against your skin.
More complex tests, such as a nerve conduction test, may also be used. In addition, if your DPN causes balance problems, an MRI or brain scan may be carried out to evaluate brain function. In some advanced cases, a nerve biopsy may be performed and forwarded to a pathologist for a final diagnosis.
Procedures for Diagnosis
subjective history of symptoms, recent trauma to the foot, and past lesions or ulcerations.
Physical assessment of vascular perfusion, foot architecture, and skin condition.
Gross light touch and pinprick sensation are tested by using basic hand-held tools (cotton wool, stick pins, or monofilament, for example).
A 128-Hz tuning fork is positioned at the base of the great toenail to evaluate the feet’s vibratory sensibility.
Usually, deep tendon reflexes are either absent or hypoactive.
investigations of nerve conduction or needle electromyogram
Differential Diagnosis
Additional possible causes for neuropathy include:
- Autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus, and Guillain-Barré syndrome.
- Diseases that are inherited, such as Charcot-Marie-Tooth disease.
- Infections (such as Lyme disease, HIV, hepatitis C, and chicken pox).
- Alcoholism.
- Insufficiency of specific vitamins, such as niacin, B1, B6, B12, and E.
- Trauma.
- Toxins (such as industrial chemicals and heavy metals).
- Medications (such as chemotherapy or some antibiotics).
- Insufficient thyroid function.
- Problems of the veins.
Treatment of Diabetic Nerve Pain
Medical Management / Interventions
Effective glycemic control and lifestyle modifications are the cornerstones of medical care, particularly for type 1 diabetes. Losing weight and engaging in physical activity are examples of lifestyle interventions.
Neuropathic pain is frequently treated with tricyclic antidepressants, anticonvulsants (such as pregabalin and gabapentin), and serotonin-norepinephrine reuptake inhibitors (such as duloxetine). Although there aren’t any well-recognized disease-modifying medications at the moment, these are being investigated and produced.
Moreover, the care and prevention of diabetic foot problems require collaborative efforts between professionals.
The Pain with diabetes in managing pain and neuropathy so that it does not become a chronic illness. The first step is to keep blood glucose levels within a specific range. Excessive blood sugar levels are harmful because they damage nerves and impair circulation. Diabetic nerve pain is often treated with medication, steroid injections, and lifestyle changes.
The cause of diabetic neuropathy is unknown. The therapy’s aim is to:
- Slowly progressing
- Relieve pain
- Manage problems and get everything back to normal.
- Reducing the rate at which the illness advances
The secret to avoiding or postponing nerve damage is to consistently maintain your blood sugar levels within your goal range. Some of your current symptoms might even get better with proper blood sugar management. Your age, the duration of your diabetes, and your general health will all be taken into account when determining the ideal target range for you.
Blood sugar levels must be tailored for each person. the following target blood sugar levels for the majority of diabetics:
- Before meals, 80–130 mg/dL (4.4–7.2 mmol/L) should be consumed.
- Less than two hours after meals, 180 mg/dL (10.0 mmol/L).
- For the majority of individuals with diabetes, the American Diabetes Association (ADA) generally advises an A1C of 7.0% or below.
Most younger diabetics have slightly lower blood sugar levels, while older adults with various medical issues and those who may be especially susceptible to the effects of low blood sugar have slightly higher levels. typically advises aiming for the following blood sugar levels before meals:
- Between 80 and 120 mg/dL (4.4 and 6.7 mmol/L) in healthy individuals 59 years of age and under.
- Between 60 years of age and older, or for those with additional medical issues such as heart, lung, or renal disease, between 100 and 140 mg/dL (5.6 and 7.8 mmol/L).
- A healthy weight, regular physical activity, and controlling your blood pressure are all important methods to help halt or stop neuropathy from getting worse.
Relieving pain
For nerve pain associated with diabetes, there are numerous pharmacological options, but not everyone responds well to them. Speak with your doctor about the benefits and possible negative effects of any medicine before selecting which might be best for you.
Prescription painkillers may be used for:
Medications that prevent epilepsy. Certain drugs that are used to treat epilepsy are also used to relieve nerve pain. Starting with pregabalin (Lyrica) is advised by the ADA. Another choice is gabapentin (Gralise, Neurontin). Swelling in the hands and feet, lightheadedness, and drowsiness are possible side effects.
Drugs that fight depression. Even in the absence of depression, some antidepressants can reduce nerve pain. The mild to moderate nerve discomfort may be reduced by tricyclic antidepressants. Amitriptyline, nortriptyline (Pamelor), and desipramine (Norpramin) are among the medications in this class. Some unpleasant side effects include dry mouth, constipation, fatigue, and trouble concentrating. When shifting from one posture to another, such as from lying down to standing, these drugs may also make you feel lightheaded (orthostatic hypotension).
Serotonin and norepinephrine reuptake inhibitors (SNRIs) represent an additional class of antidepressants with fewer pharmacological side effects that may be beneficial for nerve pain. First-line treatment with duloxetine (Cymbalta, Drizalma Sprinkle) is advised by the ADA. Another option is venlafaxine, often known as Effexor XR. Constipation, decreased appetite, fatigue, nausea, and dizziness are possible adverse effects.
An anti-seizure medication and an antidepressant may occasionally be taken together. Additionally, these drugs can be used alongside over-the-counter pain relievers or prescription medications. For instance, acetaminophen (Tylenol, etc.), ibuprofen (Advil, Motrin IB, etc.), or a skin patch containing lidocaine (a numbing agent) may provide you with relief.
Drug Therapy
If a patient’s neuropathy creates excessive pain, drug therapy may be an option. Anti-seizure medicine (frequently used to treat nerve pain and seizures) and antidepressants are two types of drugs. Antidepressants modify the chemical pathway by which the brain understands pain.
Steroid injections.
Diabetic neuropathy therapies include steroid injections and nerve blocks, which target specific areas of pain rather than administering medication in the body. Because they typically last a few months, further injections may be required.
These injections operate by preventing the pain signal from the nerve from reaching your brain. As a result of not getting any pain signals, your brain will no longer perceive those places as uncomfortable. The injections are not painful since the patient receives a numbing shot near the injection site before the drug is administered. Steroid injections and nerve blocks typically have no side effects other than minor discomfort at the injection site.
Lifestyle Changes
A diabetic patient may want to try a few at-home remedies in addition to the therapy. These include eating a healthier diet with fewer junk foods and exercising. Although it may be unpleasant at first, exercise strengthens the muscles surrounding the nerve, reducing pressure on the injured nerve. Our doctors can guide patients through a safe workout plan that targets specific muscles surrounding the nerve.
Alternative medicine
Numerous alternative and complementary treatments can be used alone or in conjunction with prescription drugs to help relieve pain. To be sure there are no possible interactions, consult your doctor before beginning any alternative therapy or taking any dietary supplements.
You may want to try: diabetic neuropathy
- Capsaicin. Some patients find that using capsaicin cream topically helps lessen their pain perception.
- Lipoic acid alpha. Some foods contain a powerful antioxidant, which may aid some people with their symptoms of nerve pain.
- Acetyl-L-carnitine. This nutrient can be gained as a supplement and is produced by the body naturally. In particular situations, it could relieve nerve discomfort.
- TENS transcutaneous electrical nerve stimulation. This medication-assisted treatment may aid in blocking the brain’s perception of pain. Through tiny electrodes positioned on the skin, transcutaneous electrical nerve stimulation (TENS) sends tiny electrical impulses to particular pathways in the brain. Doesn’t work for everyone or for all forms of pain, while being safe and painless.
- Acupuncture. Acupuncture often has no negative side effects and may help reduce neuropathy discomfort. Remember that acupuncture might not provide you with relief right away and that you could need more than one session.
Physiotherapy for the Treatment of Diabetic Neuropathy Pain
Evidence has been provided for:
- TENS stands for transcutaneous nerve stimulation.
- Massage.
- Static magnetic field therapy.
- Low-intensity laser therapy.
- Infrared monochromatic light.
- Acupuncture.
Research has indicated that strength training can assist individuals with diabetic neuropathy manage their blood sugar levels, lessen neuropathic pain, and moderately improve muscle function. As a result, for this patient group, exercise may improve their quality of life. Patients with diabetes need to take extra care, such as checking their blood sugar levels before exercising and eating a snack to avoid large changes.
- Programs of exercise that focus on flexibility (including self- and progressive stretches) should be included.
- Strengthening of muscles (using a range of modalities as needed, such as isometric, open and closed chain, and graded weight development).
- aerobic exercise.
- Training in posture and balance (for stability and fall prevention).
- Gait: In individuals with diabetic neuropathy, gait patterns and proprioception can be improved.
- Splinting for muscular weakness (such as ankle-foot orthoses) or mononeuropathies (such as carpal tunnel syndrome).
- The greatest side effect of diabetic neuropathy was a higher chance of falling. Thus, balance and fall prevention training and programs are helpful, especially for senior diabetic clients.
Exercise for Diabetic Nerve Pain
Types of Exercise for Diabetic Nerve Pain:
- Aerobic Exercise: Try to get in at least 150 minutes a week of moderate-to-intense exercise, such as dancing, walking, swimming, or cycling.
- Strength Training: To increase strength and balance, use workouts that focus on all major muscle groups two or three times each week.
- Exercises for Flexibility: Stretching reduces stiffness and discomfort by preserving joint mobility and range of motion.
- Low-Impact workouts: Pilates, yoga, and water workouts are great ways to get the benefits of movement without overloading your joints.
Aerobic Exercise
Walking

Benefit of walking
Blood sugar control
Walking regularly improves insulin sensitivity, helps cells to use glucose more effectively, and lowers blood sugar levels. Because of this, there is no need to produce excessive amounts of insulin, which helps regulate diabetes.
Control of weight
Walking helps weight loss or maintenance by assisting in the reduction of extra body fat. As a result, this improves blood sugar regulation and lowers the possibility of complications caused by obesity in individuals with diabetes.
Improved cardiovascular health
Any type of physical activity is known to have numerous positive effects on the body and mind, including improved cardiovascular health.
Improved flow of blood
Walking improves circulation by increasing blood flow, which is important for diabetics since the condition may cause their circulation to decrease.
Lowering of stress
Regular physical activity, such as walking, helps to maintain mood stability, releases endorphins to reduce stress, and may even lower cortisol levels, which affect blood sugar levels.
Strength and flexibility of joints
Walking is good for people with diabetes who may be more susceptible to joint problems because it increases flexibility and strength, which supports joint health.
Increased sensitivity to insulin
Walking regularly improves glucose absorption by cells and the body’s sensitivity to insulin, which in turn leads to better diabetes management, according to the expert.
Swimming

advantage of swimming
One of the advantages of swimming is that the water’s current reduces the effects of gravity. Yes, you can stand straight in shallow water, but your whole body feels the pressure. You can practice light leg movements while floating in the water if you know how to swim a little.
Simple foot movements can improve blood flow to your feet. You can burn a lot of calories by swimming a few strokes in the pool without straining your feet. Swimming in pools with room temperature water is advised by experts. Warm water stimulates blood circulation, while cold water typically aggravates our nerves, making it painful for a diabetic neuropathy patient.
Cycling
Anyone of any age can enjoy cycling as it’s a low-impact, healthful activity, from toddlers to seniors. In addition, it’s affordable, entertaining, and eco-friendly.
One of the most practical ways to incorporate regular exercise into your daily routine is to ride your bike to work or the store.

benefit of cycle
- Low impact: Compared to most other forms of exercise, it causes less strain and injury.
- As you pedal, cycling works all of the major muscle groups, making it an excellent form of exercise for your muscles.
- Unlike other sports, cycling does not require a high level of physical ability, making it an easy sport to play. The majority of people know how to ride a bike, and once you do, you never forget it.
- Cycling increases power, stamina, and cardiovascular fitness.
- increased flexibility and strength of the muscles.
- increased flexibility of the joints.
Strengthening training
Squats
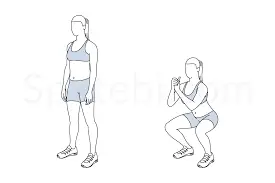
For a simple squat:
- Toes turned slightly out, start with feet slightly wider than hip-width apart.
- Push your hips back while contracting your abdominals, keeping your chest outward, and applying regular pressure to your feet.
- Once your heels begin to grow off the floor or your upper body begins to round or bend, lower yourself into a squat. Your form should decide how deep you go.
- To get back to your starting position, push through your heels with your chest out and your core tight. Tighten your glutes at the top of the mountain.
- Do ten to fifteen repetitions. Work with three sets maximum.
The benefits of squats
- Are killing calories
- Improves the strength of your lower body muscles, Some of your biggest, strongest muscles are found in your lower body.
- Your glutes, quadriceps, hamstrings, adductors, hip flexors, and calves are involved in nearly every movement you make, from getting out of bed to sitting in a chair.
- Squats are one type of strength training exercise that can help tone and strengthen the muscles in your lower body. You might discover that everything from walking to bending to exercising is easier to perform when these muscles are in good health. You might also be able to move more easily and more comfortably.
Lunges
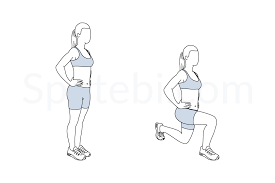
How to perform a lunge
- When standing, place your feet hip-width apart.
- Take a longer step forward than a walking stride, placing one leg in front of your body and the other behind. When your foot touches the ground, it should land and stay flat. You’ll lift your back heel off the floor.
- As you go down, bend your knees to about a 90-degree angle. Keep in mind to maintain your core engaged and your trunk upright.
- Then, to get back to where you were initially, forcefully push off with your front leg.
Benefits of Lunges
- A multi-joint exercise that can help tone and strengthen various lower body muscles is the lunge. The front of the thighs, the back of the thighs, the buttocks, the quadriceps, and the calves are all included in this (back of the lower leg).
- During the lunge, your hip flexors are stretched. This increases their range of motion and counteracts the effects of prolonged sitting, which can shorten and tighten the muscles. To maintain stability and avoid injuries, you also contract your core muscles.
- Lunges are a functional exercise, which is an additional advantage. This means that they imitate activities you engage in daily, like picking something up off the ground. Lunges may even increase your metabolism because they engage a lot of the major lower-body muscle groups.
- The split stance used in lunges changes the load on your body, allowing you to work each leg more independently than with other lower-body exercises like squats.
Push-ups

How to do it
- Starting on all fours, place your hands slightly wider than your shoulders and perform a push-up on the floor. Stretch your legs back until your hands and toes are in balance and your feet are hip-width apart. From here on out, this is how you perform a push-up.
- To tighten your core and compress your abs, pull your belly button towards your spine.
- Breathe in while lowering yourself to the ground and bending your elbows gradually until your elbows are at a 90-degree angle.
- Maintain your core tight during the entire push-up. Also, avoid bending over or arching your back; instead, maintain a straight body from head to toe.
Advantages of Push-Ups
The strength required to complete these movements comes from the functional fitness that push-ups help you develop. By strengthening the muscles that surround the shoulders, you may reduce your risk of rotator cuff injuries.
The rectus abdominis and the internal and external obliques are the abdominal muscles that are used to keep the body rigid during a push-up. The push-up is a compound exercise because it uses multiple joints.
Planks

How to do
- Choose a posture that allows you to fully extend your upper body. You can have enough cushioning to feel comfortable on all fours if you use an exercise mat. As seen in the video, you have the option of performing a plank on your forearms or palms. Numerous wrist wraps offer joint support.
- With your face down and your forearms and toes on the ground, begin in the plank position. Your forearms are pointing forward, and your elbows are exactly under your shoulders. You should be staring at the floor, but your head is relaxed.
- Pull your navel toward your spine by using your abdominal muscles. Maintain a rigid and upright torso, and maintain a straight body from your ears to your toes, without bending or sagging. The neutral spine position is this. Determine that your shoulders are lowered and not situated toward your ears. Your heels should be supported by the balls of your feet.
- For ten seconds, maintain this posture. Let go to the ground.
- Work for 30, 45, or 60 seconds at a time over time.
Advantages
- Planking has numerous health advantages. Core strengthening is an important part of any exercise program. It feels and looks good to have a strong, solid core. More importantly, though, it supports the body’s ability to power, balance, and stabilize itself during almost all other activities.
- All powerful and well-coordinated athletic movements start with core strength. You can achieve better posture and less joint stress by strengthening your core.
- An exam of core muscle strength and stability can also be based on the plank exercise. Although the plank is more of a strength-training than a cardio exercise, it can increase your calorie burn by using a variety of muscles.
Side plank

Instructions
- Lie on your right side, legs straight, feet placed on top of each other. Place your right elbow under your right shoulder, forearm pointing away, and hand balled into a fist. The pinky side of your hand should make touch with the ground.
- Breathe out while keeping your neck neutral. Brace your core.
- Lift your hips off the mat, supporting your weight with your elbow and the side of your right foot.
- Your ankles to your head should make a straight line in your body.
- For the duration of the exercise, stay in this position. Aim for 15 to 60 seconds, depending on your level of fitness.
- Repeat on the left side.
What are the advantages of a side plank?
The following are some of the primary benefits of including the side plank in your fitness routine:
- Strengthens three muscular groups equally. To maintain stability in a side plank position, the muscles in your shoulders, hips, and core sides must all fire and function together.
- Protects your spine. Keeping this muscle strong will help you avoid a back injury.
- Strengthens your core without straining your back. Unlike crunches and situps, side planks do not strain your lower back. However, this exercise does an outstanding job of increasing core strength.
- It improves your balance. A side plank exercise can assist improve your sense of balance and coordination.
Bodyweight exercise
chair dips

How To Do A Chair Dip
To try this exercise at home, you’ll need to find a stable chair or bench. A stairway or other stable elevated surface may also perform in a pinch.
- Sit in your chair or bench, arms at your sides and feet flat on the floor, hip distance apart.
- Position your palms down beside your hips. Your fingers should be gripping the front of the chair seat.
- Move your torso forward from the chair, arms extended. Your buttocks should be hovering over the floor, with your knees slightly bent. Your heels should be a couple of inches in front of your knees.
- Breathe in as you slowly lower your body, bending your elbows until they form a 90-degree angle.
- Breathe out as you push up to your starting posture, arms fully extended.
- Complete the exercise 10 to 15 times during the first set. Then finish another set. As you gain strength, you can gradually increase the number of repetitions or sets you undertake with this exercise.
Advantage
- Chair dips work the muscles at the rear of the upper arms. While the front biceps receive a lot of attention, you should work on the entire arm for maximum strength and tone.
- The triceps play an important part in everyday movements that include extending the elbow and forearm. You use them to lift objects like supermarket bags or to reach for goods that are higher up.
Chair dips are also effective in:
- Pectoralis major. This is the primary muscle of the upper chest and is sometimes referred to as the “pecs.”
- Trapezius. This triangle muscle runs from the neck to the shoulder to the middle back.
wall push-ups
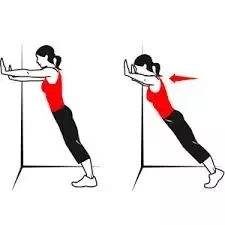
How to do
- Pushups are one of the most effective bodyweight workouts you may include in your program.
- When performing several reps correctly, you must have sufficient power in your arms, chest, back, and shoulders.
- If you have trouble performing normal pushups on the ground, wall pushups are an excellent place to start. Using a wall reduces some of the stress, allowing you to strengthen your muscles, improve your form, and prepare you for traditional pushups.
- Wall pushups are a complete body workout. While you may think of pushups as an upper-body exercise, they involve several muscles throughout the body to stabilize the position and movement.
The primary muscles involved during wall pushups are :
- The pectoralis major and minor
- The serratus anterior
- The triceps
- The deltoids
- Upper and lower back muscles (e.g., trapezius, rhomboids, spinal stabilizers)
- Core muscles include the transversus abdominis, multifidus, obliques, and rectus abdominis.
- This exercise also uses your lower body muscles, such as glutes, quadriceps, and calves, for stability. These muscles help improve your postural stability, balance, and upper-body mobility.
Crunches
Then crunches are the ideal way to build and tone your abs. There are numerous variants of the exercise you may attempt to mix up your workout and target all of the muscles in your core. Continue reading, and we’ll coach you through how to properly perform crunches and other popular alternatives to acquire those rock-hard abs.

how to do it
- With your feet flat on the ground and your legs bent, lie on your back. Cross your arms across your chest, palms positioned directly below your shoulders.
- Engage your abs, lift your head and shoulders off the floor, and hold for 1-2 counts. Then slowly lower yourself back down.
Perform 2-3 sets of crunches with 10-15 reps. - Try reverse crunches by elevating your legs right over your hips. Lift your hips and tailbone off the ground for 1-2 counts before lowering them back down.
Resistance bands
shoulder rows with Resistance bands
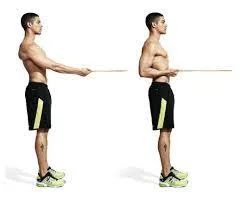
Set Up: Secure the door anchor at chest height.
Bands: Thread the band(s) through the hooks.
Body Positioning: Hold an end of the band in each hand and stand 3 to 4 feet away from the door, facing it. Stand with your feet hip-width apart, chest raised, and head straight. Position your arms straight out in front of you (parallel to the ground), palms down.
Movement
Pull straight back with your elbows at shoulder height until they are even with your shoulders and your upper and lower arms form a 90-degree angle. return and do it again.
Tips for Pulling: Keep your upper arms and forearms parallel to the floor and hold the bands lightly.
Plank with Resistance bands

How to Perform a Resistance Band Plank Front Row
- A resistance band can be attached to an anchor point, like the underside of a squat rack.
- As you turn to face the anchor point, maintain a high plank stance with the band in your right hand. Make sure the band is kept straight. Ideally, your left wrist and left shoulder are directly underneath one another. To have a neutral spine, your back should be flat. For more support and stability, expand your foot position and push your hips toward the ground if your butt is higher than your back.
- Pull the band with control, then push your right elbow back towards your chest. Your right arm is the only limb that ought to be moving. Refrain from twisting your hips. Reduce the number of reps you do or expand your foot placement if they are moving. After holding the band at your ribs for one second, go back to your beginning posture. One rep gets paid for this.
- One set consists of 10 reps on the right side and 10 reps on the left. Make three sets in total.
Lunges with Resistance bands

Here are the instructions to complete the Resistance Band Stationary Lunge With Overhead Press.
- 1) Place your right foot in the center of the band on the floor, and grasp the handles near your shoulders.
- 2) Place your left foot behind you, heel off the ground.
- 3) Lower to the ground, bending both knees at a 90-degree angle.
- 4) Slowly press back up while pushing your arms straight overhead.
- Repeat for the appropriate amount of reps, then switch legs.
- Targets include the legs, glutes, and shoulders.
Squats with Resistance bands

How to Perform Resistance Band Squats. Here are the steps to learn the Resistance Band Squat.
- Stand on the band with your feet shoulder-width apart, holding the handles next to your shoulders so that the band is behind your arms.
- Slowly sit down and return to the squat position, maintaining abdominals tight and chest lifted.
- Push back up through heels, squeezing glutes.
How to do a proper resistance band squat:
- Stand on the band with your feet shoulder-width apart, holding the handles next to your shoulders so that the band is behind your arms.
- Slowly sit down and return to the squat position, maintaining abdominals tight and chest lifted.
- Push back up through heels, squeezing glutes.
Benefits of Resistance Band Squats
- Resistance band squats are a unique approach to strengthen and tone the glutes. Many people report that a standard lunge and squat workout does not activate their glutes. Using the resistance band provides the necessary power while allowing you to sit back on your heels and focus on firing your glute muscles for the motion.
- Strengthens leg muscles. In addition to using your glutes, the resistance band squat works your quadriceps and hamstrings. Your leg muscles become involved as you press up to stand against the resistance of the band.
Triceps extension with Resistance bands

How to perform it
- To perform Resistance Band Tricep Extensions, stand with one foot slightly in front of the other and position the center of the band beneath the back foot.
- Bring the grips together directly above the top of your head.
- Slowly lower the handles behind the back of your head until your elbows are bent 90 degrees, keeping your elbows close to your side.
- Slowly press your hands back up overhead.
Advantage
Strengthens your arms Resistance band tricep extensions are a unique approach to increasing arm strength. Instead of lifting up dumbbells or barbells, the band generates strength in a unique method. Instead of using a dumbbell, the muscles work against the strength of the tight band. It’s a great and effective method to use the band for strength!
Free weight
Plank with weight

How to carry it out
- Put yourself in a quadruped, or tabletop, posture by bending down on your hands and knees and placing your hips over your knees and your shoulders over your wrists.
- With the assistance of a partner, carefully lay a weight on your upper back, such as a weight plate or sandbag.
- Assume a push-up position by slowly extending one leg behind you while maintaining your core engaged. Ensure that your head is neutral and your body is straight.
- With your shoulders perfectly above your elbows, extend onto your forearms while keeping proper form.
- Hold until you’re about to become tired, then slowly release the grip. With a partner, take the weight off.
Advantages of the Balanced Plank
- Increases muscle mass, but longer bodyweight planks increase endurance.
- Allows you to target different muscle groups according to where the stress is placed.
- Can, because of the increased core strength, improve posture and form in other workouts.
Dumbbell rows
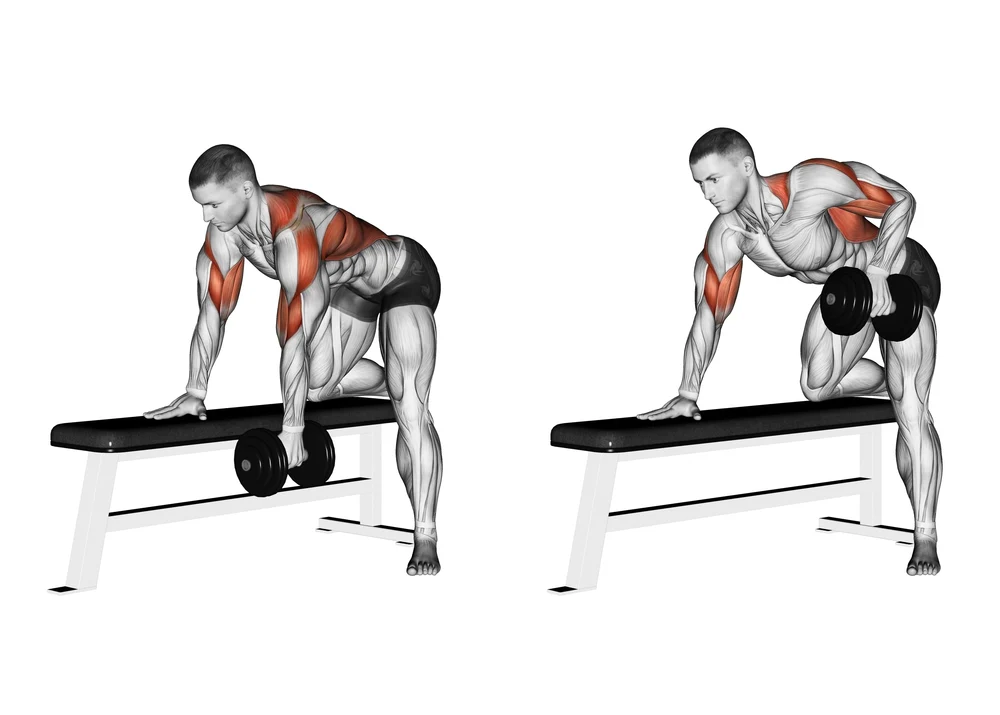
How to do it:
- Maintain a hip-width distance between your feet while grasping a dumbbell in each hand.
- Slightly bend your knees, then maintain a straight back while rotating at the hips.
- Row the dumbbells up to your chest while pressing your shoulder blades together.
- Slowly lower the dumbbells back down.
- Do 10 to 12 repetitions.
squats with dumbells
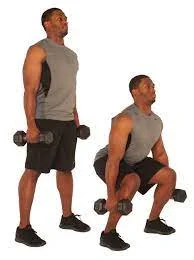
how to do it
- Hold one dumbbell close to your chest.
- Sink your hips back and squat down.
- Your elbows should be in between or just above your knees at the bottom.
- Drive back up, tightening your glutes at the top.
- Repeat. Push yourself through these; you can probably do more than you realize.
lunges with dumbbells
how to do it
It’s simple to do the lunge wrong, and there are lots of variations; here’s how to master the forward dumbbell lunge technique:
- Begin standing tall, feet under hips, chest high, core tight, weights in each hand, arms hanging at your sides. To improve your equilibrium, concentrate on the surface 2 meters in front of you.
- Lift one foot off the floor and take a long step forward, placing it in line with your hips. Consider walking on ‘train tracks’ rather than a ‘tightrope’.
- Sink the back knee till it hovers just above the floor. Your front quadriceps and back shins should be parallel to the floor, with right angles at each knee.
- Keep your core engaged and return to standing by pushing through the front heel.
- Repeat on the same side for the specified number of reps before switching to the opposite side.
Dumbbell lunges work the following muscles:
- Quadriceps: Dumbbell lunges primarily target the quads during the eccentric and concentric portions of the exercise. Shortening the gait and keeping the body upright allows you to use the quads more effectively.
- The glutes are another key muscle group involved in the dumbbell lunge. You can make the most of your glutes by taking a longer step and bending forward throughout the exercise.
- During the rising part of the exercise, the hamstrings contract to return you to standing.
- Calves: The calves aid to stabilize the dumbbell lunge.
- Secondary muscular groups include abductors, core, trapezius, and grip strength.
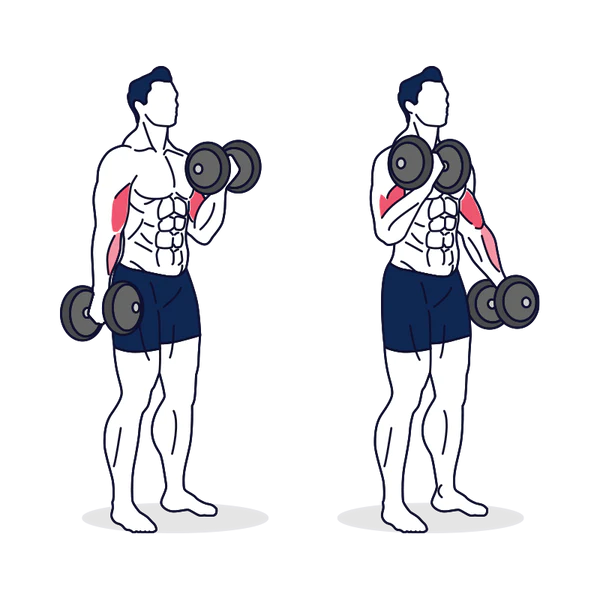
Biceps curls

How to do it
- Stand in the center of a looped resistance band.
- Loop both ends of the band around the inside of the dumbbells while holding them palm up.
- Brace your core and curl the dumbbells up to about shoulder level.
- Form tip: To recruit more muscle fibers, curl slowly, calmly, and fully with your hands up.
Additional tips for treating diabetic nerve pain with resistance bands:
- Select a band with resistance that is between light and medium. Each exercise should be able to be performed 10–12 times with proper form.
- Set goals for form over weight. Proper performance of the exercises is more important than using a larger band.
- Take regular, deep breaths while working out.
- When necessary, give yourself a break.
- Avoid exercising when you’re hurt.
Additional suggestions for using resistance bands to treat diabetic nerve pain:
- Warm up before beginning your workout. Do 5-10 minutes of gentle aerobics to get your blood flowing and muscles warmed up.
- After you’ve finished your workout, cool down. Perform some static stretches for 5-10 minutes to help reduce muscle soreness.
- Do not overdo it. Begin cautiously, then progressively increase the intensity and duration of your workouts over time.
- Listen to your body. If you experience any pain, stop exercising and rest.
- contact to physician This is particularly important if you have any other medical issues.
Overhead press
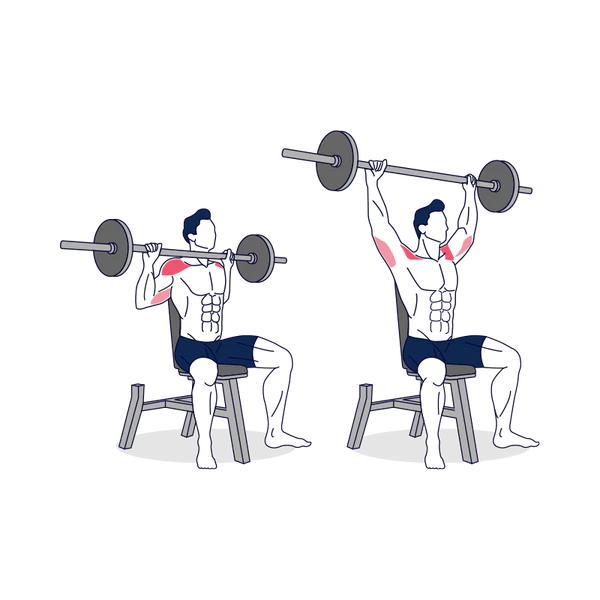
How to Do it
- Starting position: Stand shoulder-width apart, holding a barbell with a pronated (overhand) grip at upper-chest height.
- At the top of the exercise, shrug your shoulders to raise the barbell even higher.
- Inhale as you reverse the actions and carefully drop the barbell to its starting position.
- Repeat.
Biceps curls
Additional guidance for using free weights when experiencing diabetic nerve pain:
- Select weights that are comfortable to hold and manage.
- Apply a spotter if necessary.
- Make sure your shoes are supportive and easy.
Flexibility and Balance Exercise
Neck roll
Principal muscles: cervical spine and neck
Shoulders are secondary muscles.
Tools: Nothing to use
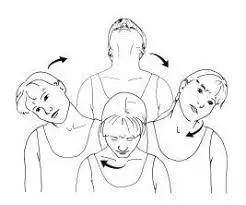
Instructions for Neck Rolls
- Look forward and maintain a straight head to start.
- Start rotating your head back while inclining it gently to the right.
- Continue to roll your head down and then leave.
- Return your head to the beginning position and repeat the process in the other way.
Proper Form and Breathing Sequence
Keep your shoulders loose and your motions large, think about, and flow. Inhale deeply and slowly extend your neck, being careful not to let it drop too far back. You can begin with a semicircular movement if your neck is too weak or if it causes you any discomfort. Bend your head to the left, then back to the front, and finally to the right shoulder, lowering your chin towards your chest.
Benefits of Exercise
The cervical spine and the muscles in the neck are stretched and relaxed with the neck roll, a dynamic stretching exercise. This exercise can help avoid neck pain and injuries as well as relieve any pain or stiffness caused by a strain on the neck.
Arm circles

How to do arm circles: a step-by-step guide
This is how arm circles should be done correctly.
- With your hands out and parallel to the ground, and your feet shoulder-width apart, maintain a straight posture.
- Keep your back straight and use your entire arm to make little circles.
- Start moving your arm in bigger circles while maintaining control over your motion. You should begin to feel something in your triceps, which are located at the lower part of your upper arm, as the circles get bigger.
- Hold on for ten to fifteen seconds, then change course.
Tandem stance

The purpose
This exercise narrows your base of support, which tests your balance.
Set up
Place your feet hip-width apart as you stand up.
Motion
Make sure the toes of your back foot are touched by the heel of your front foot as you carefully place one foot in front of the other. Take up this role. Then carry out the same action with the front foot.
Advice
- To help you keep your balance, you can extend your arms to the sides.
- Keep your eyes focused on something upfront.
- Try this exercise in front of a doorway, table, or countertop if you feel unsteady so you can place one hand on a surface to support yourself as needed.
Heel to walk

Step By Step
- This is an outstanding balance exercise.
- Just walk straight forward, but with each step, make sure you touch the toes of your opposite foot with your heel.
- Next, you can alternate a single arm movement out to the side to make this harder to set straight ahead rather than down.
- The goal is to increase to one minute, and you can do this twice a day.
One leg stand

Perform the single-leg stance balance exercise. As with the test, situate yourself against a chair or near something stable.
- Hold on to the chair’s back with both hands.
- Lift one leg off the ground slowly.
- Keep your balance while standing on one leg for 5 seconds.
- Return to the starting location and repeat five times. Try to spend more time standing on one leg.
- Perform with the other leg.
Benefits
The capacity to stand on one leg is important. When walking, you spend roughly 40% of your time with one foot on the ground while the other leg moves in the air. The single-leg stance is a basic yet effective exercise for improving balance.1
Improving your balance can help improve sports performance and may help you avoid falls that can cause serious injury.
Remember to:
- As you gain strength, start slowly and progressively increase the duration and intensity of your workouts.
- When you feel any pain, pay attention to your body and stop.
- Take regular, deep breaths while working out.
- Before beginning your workout, warm up, and then cool down.
- If you need support, especially when performing balance exercises, think about using a chair or wall.
Yoga
Supta Matsyendrasana

Supta Matsyendrasana, also known as Spinal Twist
The best exercise for diabetic neuropathy is the spinal twist, despite it being difficult. With your hands supporting the stance, take a seat on the floor with one knee crossed over the other. The muscles are warmed up with this gentle stretch, and then you can advance to the full position.
Make sure your right hand and right foot touch the floor and your left elbow is on your right knee after you have crossed your right foot over on your left thigh. After a while, switch the legs and try to get into the pose as many times as you can. Try extending your back a little for better outcomes. To stretch the muscles in the neck region, move the head.
The many benefits of this yoga position for peripheral neuropathy include improved blood circulation and comfort of the neurological system.
Balasana, or Child’s Pose

One of the simplest exercises you may use to manage peripheral neuropathy is the balasana. This is one of the most important exercises for curing peripheral neuropathy since it is simple and stimulates the body and nerves.
To begin, kneel and tuck your tummy in towards your thighs. Then, bend forward until your forehead makes contact with the yoga mat.
Breathing in Three Parts, or Dirgha Shwasan

The yoga position known as Dirgha Shwasan doesn’t take much work. This pose relieves neuropathic pain by stretching the back muscles and aiding in the discharge of toxins. Backaches can also be relieved by doing this stance. It improves healthy blood and oxygen circulation through breathing. To perform this pose, just sit up straight and focus on taking deep, rapid breaths.
Bending Bend or Dhanurasana

Back discomfort can be relieved, muscles can be stretched and strengthened and overall muscular strength can be increased with the help of the yoga pose Dhanurasana. To provide enough oxygenation and blood circulation, this yoga stance enables inhalation and exhalation.
Start by stretching while lying on your back. Then, raise your legs fully to create a full curve.
keeping your feet with your legs and keeping that position for a brief period will also help you extend your legs. To achieve the desired stretch for your body, repeat this pose multiple times.
how to perform the legs-up-the-wall standing correctly.
- Place your shoulder and hip on the wall while you sit next to an open wall.
- After lowering your back to the floor, raise your legs gradually and press them up against the wall.
- There should be a perfect angle between your back and your legs. Put a folded blanket or cushion under your hips if you experience any lower back pain.
- Take a few deep breaths and hold this position for five minutes.
- When you’re finished, take your feet off the wall and bend your knees. Give yourself a moment before exerting yourself.
- Just so you know, avoid doing this posture immediately after eating because it can slow down your digestion and cause you to feel queasy and lightheaded.
Corpse Pose or Savasana

The complex causes of peripheral neuropathy can be managed using Corpse Pose or Savasana. This yoga stance aids in restoring the energy expended throughout other yoga poses. This is a nice resting pose that can be included in the middle or conclusion of your yoga practice, as it doesn’t need much effort on your part.
To practice this stance, you must lie on your back like a corpse. Ensure that your hands are by your sides and that no part of your body touches another. Hold this posture for at least fifteen minutes.
Benefits of Yoga for Diabetes-Related Neuropathy
Here are some of the biggest advantages of yoga for neuropathy:
- The nerve fibers connecting the brain and nerves are strengthened by yoga. As a result, it slows the condition’s progression while also assisting in managing the symptoms of neuropathy.
- Yoga not only calms the body and mind, but it also builds resilience by regularly attending to the mind. By assisting in the acceptance of neuropathy, deep breathing increases strength and reduces tension.
- Improved blood flow: Mild yoga positions can improve blood flow, which may aid in delivering nutrients and oxygen to injured neurons and could even help in the healing process.
- Pain relief: The body’s natural analgesics, endorphins, are released when specific yoga stretches and poses gently activate the nerves.
- Reduction of stress: Pain from chronic illness can be difficult, and stress causes pain. Indirectly decreasing pain perception, yoga breathing exercises and meditation practices can aid in stress and anxiety management.
- Improved balance and flexibility: Yoga helps increase balance and flexibility, which is particularly beneficial for those with neuropathy who might have trouble standing or walking.
- Improved sleep: Poor sleep can exacerbate pain. The relaxing methods of yoga may improve the quality of sleep, which helps with pain management.
Tree pose

how to do it
- Perform the Tadasana position. Firm your leg muscles, spread your toes, and press your feet into the mat. To carefully elevate your lower abdomen, raise the points of your front hips towards your lower ribs.
- As you lift your chest and inhale deeply, push your shoulder blades down your back and exhale. Look at a stable point directly ahead.
- Raise your right foot onto your left leg or shin while placing your hands on your hips. Avoid touching the knee.
- Press your left leg and right foot together.
- Verify that your pelvis is squared off to the front and level.
- Once you are steady, extend your arms above you like branches reaching towards the sun, or position your hands in the Anjali Mudra at the heart.
- After holding for a few breaths, return to Mountain Pose and change sides.
Tia chi
A series of slow, delicate physical postures and motions, a meditative state of mind, and controlled breathing are all part of the practice of tai chi. In ancient China, tai chi was developed as a martial art. The focus has shifted throughout time to include rehabilitation and health promotion.

benefit
Tai chi may benefit persons with low back pain, fibromyalgia, and osteoarthritis in their knees, according to a small body of research. Tai chi may help with diabetic nerve pain, but its effects on rheumatoid arthritis pain are unknown. For those with Parkinson’s disease and older people, tai chi may help with balance and fall prevention. Tai chi’s potential to prevent falls in those who have experienced strokes, individuals with osteoarthritis, and those suffering from heart failure remains unknown.
Stretching
Hamstring

Start with a simple hamstring stretch. If you have low back discomfort or sciatica, diabetic nerve pain this exercise may put a strain on your back, so use caution.
- With both legs straight, take a seat on the floor.
- Extend your arms and extend forward, bending your waist as far as possible while keeping your knees straight.
- Hold this position for 15–30 seconds.
- Relax back into the beginning position.
- Repeat three times.
- Stretch until you feel a mild tug on the back of your thighs. If you experience severe discomfort, you should discontinue the workout.
Safety and precautions
A wide hamstring flexibility program can help your hamstrings move more effectively. Before beginning this or any other fitness program, contact a medical professional or a physical therapist to ensure that the exercise is safe and effective for you.
Quadriceps stretch
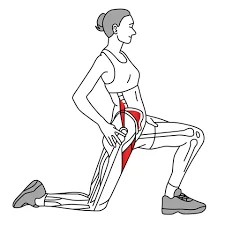
The Kneeling Lunge is a traditional hip flexor stretch. However, because the knee is flexed, the stretch tends to favor the rectus femoris muscle.
As long as the patient is comfortable putting pressure on the knee, this is my go-to quad stretch. It not only provides an amazing stretch but also teaches the patient how to move through the hip. It also acts as an excellent warm-up for the lunge exercise, which is frequently dysfunctional and requires rehabilitation when the quads are tight.
To complete the stretch correctly, make sure the action originates from the hip. The two most typical mistakes patients make when trying to get around the hip are tilting the pelvis anteriorly and hyper-extending the lumbar spine, or leaning forward with their entire trunk. Having the patient undertake a posterior pelvic tilt and wear an abdominal brace will help to prevent the first problem. The second issue can be addressed by instructing the patient to keep the shoulder stacked over the hips.
The patient should shift forward until they feel a light pressure on the front of their leg, then back to release the stretch.
I have them do 10-15 reps.
A different method is to ask them to hold the last stretch for 15-30 seconds.
Calf Stretch

how to do it
- Stretch against a wall.
- Throughout this exercise, keep a straight posture.
- Stand in a stride, with the leg to be stretched behind you.
- Lunge forward while keeping your knee straight on the leg you’re stretching until you feel stretch tension in your calf or knees.
What are the advantages of this exercise?
This exercise mainly stretches the major calf muscle and also extends the front of your hip. The calf might be tight as the tissues in the rear of the leg relax due to hip mobility failure.
Important Tips for Working Out While Getting Diabetic Nerve Pain:
- Start Gradually and Gently Increase but don’t go excessive. Short, easy sessions should be started, and when tolerance allows, length and intensity should be gradually increased.
- Pay Attention to Any Pain or Discomfiture That Your Body May Be Feeling. If you feel a lot of pain, stop what you’re doing and see a doctor.
- Wear Suitable Footwear: Opt for well-fitting, supportive, cozy shoes that will shield your feet.
- Warm Up and Cool Down: To avoid injuries, always warm up before exercising and cool down afterward.
- Keep Hydrated: To maintain nerve function and stay hydrated, drink lots of water before, during, and after activity.
- Keep an Eye on Your Blood Sugar: If you see any deviations from your typical patterns, make sure to check your blood sugar levels both before and after exercise.
Benefits of Physical Activity for Diabetic Nerve Pain:
- Pain Reduction: Exercise increases circulation and blood flow, which stimulates nerves and reduces the feeling of pain.
- Improved Nerve Function: Exercising in physical exercise helps promote nerve regeneration and improve the transfer of signals from your nerves, which may reduce tingling and numbness.
- Improved Mobility and Balance: Regular physical activity increases muscle strength and coordination, which improves stability and balance while reducing the chance of falls, which is a significant concern for people with diabetic neuropathy.
- Blood Sugar Control: Exercise has an important function in controlling blood sugar levels, which is important for both managing current symptoms and preventing more nerve damage.
- Mental Health Boost: Training in physical activity produces endorphins, which are organic mood enhancers that can help fight anxiety and depression that are frequently caused by long-term pain.
Self-care
By taking these steps, you can lower your chance of developing diabetic neuropathy and feel better overall:
- Maintain optimal blood pressure regulation. You run an even higher risk of problems if you have both diabetes and high blood pressure. Make an effort to maintain your blood pressure within the range that your physician recommends, and make sure that it is measured at each visit.
- Make wholesome food selections. Consume a healthy, well-balanced diet rich in a range of nutritious foods, particularly fruits, vegetables, and whole grains. To help you reach or stay at a healthy weight, keep your portion proportions in check.
- Be active every day. Exercise maintains your heart healthy, increases blood flow, and lowers blood sugar. Aim for 150 minutes per week of moderate aerobic activity, 75 minutes per week of strong aerobic activity, or a mix of both. Taking a break from sitting every thirty minutes to get a few short bursts of activity is also a good idea.
- Before you begin exercising, see your physician or physical therapist. Some exercises, like walking, may be safer than others if you have limited feeling in your legs. Choose exercises that don’t force you to place weight on your damaged foot if you have a sore or injured foot.
- Give up smoking. Any kind of tobacco use increases the risk of developing impaired foot circulation, which could delay the healing process. If you smoke, discuss strategies to stop with your healthcare physician.
- Support and dealing. It might be difficult to live with diabetic neuropathy at times. Encouragement and guidance on coping with diabetic neuropathy can be found in support groups. Find out from your medical professional if there are any nearby therapists or if they can recommend one. By way of its website, the ADA provides online assistance. Speaking with a therapist or counseling professional could be beneficial if you’re experiencing depression.
Can You Reverse Diabetic Neuropathy?
Diabetic neuropathy cannot be reversed. Thankfully, there are solutions for managing the symptoms and preventing future damage. Diabetic neuropathy discomfort is mostly caused by high blood pressure, which can destroy nerves.
The key to decreasing the symptoms of diabetic neuropathy is to control blood and glucose levels. Different forms of medication, therapy, and surgery can be used to address pain and other symptoms of neuropathy.
Diet for Diabetic nerve pain
What foods should I avoid if I have neuropathy?
Certain meals might aggravate neuropathy by increasing blood sugar levels, causing inflammation, and harming nerves. Heavy alcohol consumption is known to cause nerve damage and increase pre-existing neuropathy symptoms. Other foods to avoid if you suffer from neuropathy include:
- Gluten in processed foods.
- High-sodium
- Refined grains
- Added sugar
- Trans and saturated fats.
Remember to keep hydrated and eat foods rich in vital vitamins, minerals, and antioxidants, such as fruits, vegetables, and whole grains, which help to reduce inflammation and stabilize blood sugar.
When to visit a doctor
If you have the following symptoms, schedule an appointment with your doctor:
- A cut or sore on your foot that has become infected or will not heal
- Burning, tingling, weakness, or discomfort in your hands or feet that affects everyday activities or sleep
- Changes in digestion, urination, and sexual function
- Dizziness and fainting.
- The American Diabetes Association (ADA) recommends that diabetic neuropathy screening begin immediately when a person is diagnosed with type 2 diabetes or five years after being diagnosed with type 1. Following that, screening is suggested once a year.
Prevention
A smart preventative measure is to keep your blood sugar under control using a mix of food and medications. It is also important to never go barefoot, even within your home, to avoid issues. Visit your primary care physician frequently to monitor your blood sugar levels, and if required, consult an endocrinologist. See your podiatrist regularly and avoid undertaking any ‘bathroom surgery’.
- Blood Sugar Management Is Important: The key to avoiding diabetic nerve damage is to keep your blood sugar levels within the desired range. Controlling blood sugar is important because high blood sugar destroys nerves over time.
To effectively manage your diabetes, check your blood sugar levels regularly and follow your doctor’s advice. This might include taking medicine, altering one’s diet, and exercising often. - Take good care of your feet by checking them every day for cuts, sores, and blisters. Put on appropriate, well-fitting footwear that will protect your feet. Regularly moisturize your feet to keep them from drying out and cracking.
- Keep up a healthy diet by selecting a well-balanced meal high in whole grains, fruits, vegetables, and lean protein. Steer clear of processed foods, sugar-filled drinks, and bad fats. A balanced diet improves general health and aids in blood sugar regulation.
- Give up smoking: Smoking increases circulation and nerve damage, which raises the risk of diabetic neuropathy.
- Get moving regularly: Try to get in at least 150 minutes a week of moderate-intensity exercise. Exercise protects against nerve damage by improving nerve function and blood sugar metabolism.
Risk factor
- Risk Factors
- Poor glycemic control.
- High blood pressure
- Smoking.
- Advance age.
- Diabetes disease with an extended duration.
- Excessive consumption of alcohol.
- Tall architecture
- High Blood Sugar:
Diabetes is primarily caused by chronically elevated blood sugar levels, which destroy nerve tissue. Neuropathy is more likely to occur the longer and more often your blood sugar is above your goal range.
It is important to maintain proper blood sugar control through food, exercise, and medication to avoid or minimize nerve damage.
2. Length of Diabetes:
The likelihood of developing nerve pain increases with the length of time you have diabetes. Exposure to high levels of sugar in the blood gradually deteriorates the nerves and raises the risk of injury.
Diabetes must be diagnosed and treated early to lower the risk of nerve problems.
3. Age
Compared to younger people, diabetics over 40 have a higher risk of developing nerve discomfort. Exposure to elevated blood sugar levels exacerbates the effects of aging on nerve function.
When you have diabetes, proactive care, and routine examinations become even more important as you age.
4. Additional Health Issues:
Obesity, hypertension, hypercholesterolemia, and kidney illness are a few medical disorders that might exacerbate nerve injury and raise the risk of neuropathy.
Taking care of these illnesses in addition to diabetes is necessary for complete protection against nerve problems.
5. Way of Life Practices:
Smoking raises the risk of diabetic neuropathy by dramatically impairing nerve and blood circulation. Reducing your risk requires quitting smoking.
Drinking alcohol can also harm nerve function. For those with diabetes, moderation or abstinence is advised.
Insufficient physical activity has been linked to impaired nerve and blood sugar function. Exercise regularly is important for preventing nerve injury.
6. Genetics:
Some persons are more prone to developing diabetic neuropathy because they have a hereditary tendency to nerve damage.
Even though you have little influence over your genetic makeup, knowing your family history can help you manage your diabetes and risk factors more effectively.
Complication
You may require treatment from several doctors to manage issues. These could include a urologist (who addresses issues with the urinary tract) and a cardiologist (who can assist cure or prevent heart-related issues).
Your level of neuropathy-related problems will determine what kind of treatment you require:
Urinary tract issues. Depending on how some medications influence bladder function, your doctor might advise stopping or switching to a different prescription medication. Some bladder issues can be resolved by following a strict routine or timing your urine and gently pressing the area under your belly button. If the bladder’s nerves are destroyed, further techniques like self-catheterization could be required to remove the urine.
Digestive problems. Eating smaller, more frequent meals may help ease mild symptoms of gastroparesis, such as indigestion, belching, nausea, or vomiting. Gastroparesis, diarrhea, constipation, and nausea may be relieved with diet modifications and medicines.
I am standing with low blood pressure (orthostatic hypotension). Simple lifestyle modifications like quitting drinking, consuming lots of water, and gradually moving from a seated to a standing position are the first steps in treatment. Elevating the head of the bed by 4 to 6 inches during sleep will help avoid excessive blood pressure during the night.
Sexual dysfunction. While not everyone finds oral or injectable medications to be safe and beneficial, some men may see an improvement in their sexual function. The penis may receive more blood flow thanks to mechanical suction devices. Women could find vaginal lubricants useful.
- Amputations and Foot Ulcers: It might be challenging to feel cuts or injuries in the foot due to diabetic nerve discomfort, which can also produce numbness and reduced feeling. This may cause tiny cuts or blisters that go unnoticed to turn into dangerous, non-healing ulcers.
- If left untreated, ulcers can develop infected and require hospital stays and antibiotics. In severe cases, the afflicted toe or foot may need to be amputated.
To avoid ulcers and amputations, routine foot examinations, suitable footwear, and correct wound management are important. - Accidents and Falls: Nerve damage-related weakness and balance issues might make you more at risk for falls, which can result in fractures, sprains, and other injuries.
Additionally, your doctor could advise compression support for your thighs and abdomen (such as an abdominal binder and compression stockings or shorts). Treatment options for orthostatic hypotension include some drugs, used separately or in combination.
Your quality of life may be adversely affected by this, as it may greatly limit your freedom and movement.
Your gait and stability can be improved with physical therapy and balancing exercises, which lowers your chance of falling.
- The Charcot Foot: The loss of sensation and repeated pressure cause damage to the bones and joints of the feet, resulting in this serious effect. It may result in amputations, instability, and abnormalities.
To stop the progression and maintain foot function, early diagnosis, and suitable treatment—including bracing and protective footwear—are important. - Mental Health Problems: Anxiety, despair, and a lower quality of life can result from chronic pain and worry about issues.
Holistic well-being requires not just pain management but also seeking emotional support and stress management.
Issues with Digestion:
- The digestive tract may be affected by nerve injury, resulting in symptoms such as bloating, constipation, diarrhea, and nausea.
- Management of blood sugar levels, medication, and dietary modifications can help control these digestive problems.
Dysfunction of the Sexual Organs: Nerve injury may affect a person’s ability to awaken, experience orgasm, and discharge in both men and women.
Maintaining closeness can be achieved by managing these problems with your partner and seeking medical advice.
Important Points:
- Cause: Chronically high blood sugar that damages nerves all over the body, most commonly affecting the feet and hands. This damage to your nerves disrupts the impulses that go from your nerves to your brain, causing pain, numbness, and other problems.
- Symptoms: Although they differ from person to person, symptoms can include:
Pain: Often characterized as being worse at night, pain might be burning, tingling, stabbing, or shooting.
Lack of feeling, especially in the fingers and toes, is called numbness.
Weakness: Having trouble holding or moving objects.
Constipation, diarrhea, nausea, and bloating are examples of digestive issues.
Treatment: The goals are to control blood sugar, reduce discomfort, and stop more nerve damage.
Successful Management Techniques:
The basic principle of treating diabetic nerve discomfort is blood sugar regulation. Stabilizing blood sugar levels can potentially reduce symptoms and decrease the progression of nerve damage. Exercise, diet, and medicine can help achieve this.
- Medications: Topical analgesics, antidepressants, anticonvulsants, and over-the-counter drugs are useful in the management of pain.
- Lifestyle modifications: Pain and general well-being are greatly impacted by quitting smoking, regular exercise, proper foot care (including routine examinations for wounds and infections), and a nutritious diet.
- Physiotherapy: Exercises, manual therapy, and other methods can help with gait stability, pain perception, and pain management.
- Alternative therapies: For some people, acupuncture, spinal cord stimulation, and plasma exchange (PLEX) therapy may provide extra improvement.
Prognosis
Diabetic neuropathy’s mechanisms are not well understood. Currently, available treatments can reduce pain and manage some related symptoms, but they usually take time to take effect.
As a side effect, the loss of feeling in the feet increases the risk of injury (see diabetic foot).
Conclusion
Painful Tingling, Numbness, and More:
Diabetic nerve pain, a common and often debilitating complication of diabetes, affects over half of those living with the condition. It arises from high blood sugar damaging the nerves, leading to various unpleasant symptoms. While there’s no cure, fortunately, effective management strategies can significantly improve your quality of life
When combined with medical therapy, yoga can significantly reduce pain while improving the quality of life in people with peripheral neuropathy. Nevertheless, before attempting yoga for diabetic neuropathy, always get medical advice.
FAQs
How may diabetic nerve pain be relieved?
Diabetic neuropathy can be safely and naturally relieved with certain physical therapy exercises. The best low-impact workouts are mind-body exercises, swimming, strength training, and work on balance and stability. Steer clear of high-impact workouts like cardiovascular exercise because they may cause numbness in the nerves.
Do episodes of diabetic nerve pain occur?
Usually, within a few weeks or months, the symptoms start to get better on their own. Depending on the nerve that is affected, symptoms can include: Having trouble focusing or observing double vision. One side of your face paralysed
Is nerve discomfort from diabetes severe?
Some, however, may find diabetic neuropathy to be extremely painful and incapacitating. Up to 50% of diabetics may develop diabetic neuropathy, a dangerous side effect of the disease. However, with regular blood sugar control and a healthy lifestyle, you may frequently prevent diabetic neuropathy or limit its progression.
What is the home treatment for foot nerve pain?
The main goals of at-home therapy are usually pain relief and preventing future injury to the injured foot.
Soak in Epsom Salts and Warm Water.
Compression socks/neuropathy socks, rest, ice the pain, check your feet every day, etc.
Avoid Alcohol. …
Lidocaine is a pain reliever. Rub your feet
Which fruits are beneficial for nerve injury?
Six Outstanding Plant-Based Diets for Dealing with Neuropathic Pain…
Antioxidants found in berries, peaches, cherries, red grapes, oranges, and melons, among other fruits, aid in lowering inflammation and minimizing nerve damage. Furthermore, it has been discovered that resveratrol, a powerful anti-inflammatory molecular structure, is abundant in grapes, blueberries, and cranberries. Zucchini
Is it beneficial for diabetic neuropathy to walk?
Avoid repetitive, weight-bearing exercises like jogging, prolonged walking, and step aerobics if you have nerve damage in your feet. On neuropathy-affected feet, repetitive stress can cause fractures, joint issues, and ulcers. Select activities that won’t strain your feet, like swimming.
When do diabetics have nerve pain?
In conclusion, diabetic peripheral neuropathy is a common difficulty associated with diabetes. It becomes increasingly prevalent in over 50% of Type 2 diabetic individuals over 60 years of age as a result of increasing age and length of diabetes.
Does hydration make nerve pain go away?
Drink a lot of water.
Any diet should include plenty of water, but those trying to reduce nerve discomfort should include it even more. Drinking enough water throughout the day is important for lowering inflammation and preventing the activation of pain receptors. Eight 8-oz glasses of water should be taken daily.
Which medication relieves nerve pain the best?
One of the best drugs for treating nerve pain is an anticonvulsant. Pregabalin (Lyrica) and gabapentin (Neurontin) are two examples. Although these drugs usually work wonders for relieving nerve pain, they can sometimes have unfavorable side effects like fatigue.
Why does nighttime nerve pain aggravate?
The degree of warmth. Your peripheral nerves may tingle more during the night when the temperature drops and you may feel a scorching or stabbing pain. Furthermore, being in the cold may cause your heart rate to decrease, which could restrict blood flow and exacerbate uncomfortable symptoms. Reduced delays
How may my neuropathy be relieved right away?
Over-the-counter nerve Pain Treatments
and topical analgesics. For the treatment of nerve pain, numerous over-the-counter lotions and ointments are available.
medications that reduce pain. Certain individuals suffering from neuropathic pain resort to well-known over-the-counter medications such as ibuprofen, aspirin, and acetaminophen.
vitamins and supplements
Which symptoms indicate nerve damage?
The following are the most typical signs of a nerve condition:
a sensation in your limbs or extremities of burning, tingling, numbness, or pain.
weakness, paralysis, or loss of muscle strength that is not explained.
a chronic headache that develops unexpectedly or feels “different”
issues relating to coordination.
pain shooting down one leg
References
- Diabetic Neuropathy. (n.d.). Physiopedia. https://www.physio-pedia.com/Diabetic_Neuropathy
- 1mg.com. (n.d.). https://www.1mg.com/diseases/diabetic-nerve-pain-107
- Siwek, S. (2023, December 19). Diabetic Nerve Pain Treatment. The Pain Center. https://www.thepaincenter.com/blog/diabetic-nerve-pain-treatment/
- Ankle, C. F. A. (2024, January 19). Why Do You Get Diabetic Nerve Pain? Certified Foot & Ankle Specialists. https://certifiedfoot.com/why-do-you-get-diabetic-nerve-pain/
- Diabetic neuropathy – Symptoms & causes – Mayo Clinic. (2022, April 29). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/diabetic-neuropathy/symptoms-causes/syc-20371580
- Log In ‹ Mobile Physiotherapy Clinic — WordPress. (n.d.). https://mobilephysiotherapyclinic.in/wp-admin/post.php?post=72198&action=edit
- Diabetic neuropathy – Diagnosis & treatment – Mayo Clinic. (2022, April 29). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/diabetic-neuropathy/diagnosis-treatment/drc-20371587
- Sharon, A. (2023, September 18). Tips for Treating Diabetic Nerve Pain. Healthline. https://www.healthline.com/health/tips-treating-diabetic-nerve-pain#capsaicin-crea
- Diabetic neuropathy. (2023, December 1). Wikipedia. https://en.wikipedia.org/wiki/Diabetic_neuropathy
- S. (2020, December 12). Does Swimming Reduce Diabetic Neuropathy | Syounaa. Syounaa. https://syounaa.in/does-swimming-soothe-diabetic-neuropathy/
- Kalra, P. (2023, December 4). 8 benefits of walking for diabetics to keep health in check. Health shots. https://www.healthshots.com/preventive-care/self-care/benefits-of-walking-for-diabetics/
- Tadvi, D. (2024, January 22). Nerve Pain In The Feet : A Guide to Managing Foot Nerve Pain. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/nerve-pain-in-the-feet/#Cycling
- Cpt, P. W. (2022, November 25). How to Do Lunges: Proper Form, Variations, and Common Mistakes. Verywell Fit. https://www.verywellfit.com/how-to-lunge-variations-modifications-and-mistakes-1231320
- Mpt, T. E. P. (2023, April 14). What Muscles Do Lunges Work? Healthline. https://www.healthline.com/health/fitness-exercise/lunges-muscles-worked#how-to
- Lindberg, S. (2023, May 26). 7 Benefits of Doing Squats and Variations to Try. Healthline. https://www.healthline.com/health/exercise-fitness/squats-benefits#What-benefits-can-you-get-from-squat-variations?
- Ms, E. Q. (2022, September 15). How to Do a Plank: Proper Form, Variations, and Common Mistakes. Verywell Fit. https://www.verywellfit.com/the-plank-exercise-3120068
- Ms, E. Q. (2022, August 2). How to Do Push-Ups: Proper Form, Variations, and Common Mistakes. Verywell Fit. https://www.verywellfit.com/the-push-up-exercise-3120574
- Ajani, L. (2023, August 17). How to Do Crunches: Proper Exercise Form & Variations. wikiHow. https://www.wikihow.com/Do-Crunches
- Cpt, K. D. M. R. (2023, May 30). Wall Pushup Variations for a Strong Chest, Shoulders, and Back. Healthline. https://www.healthline.com/health/fitness-exercise/wall-pushups#are-they-easier
- Marcin, A. (2023, July 24). How to Do Chair Dips. Healthline. https://www.healthline.com/health/chair-dips#muscles-worked
- The Benefits of a Side Plank and How to Do It Safely. (2020, November 10). Healthline. https://www.healthline.com/health/side-plank#benefits
- Pt, L. I. (2021, July 5). How to Do a Single Leg Stance. Verywell Fit. https://www.verywellfit.com/single-leg-stance-exercise-for-better-balance-2696233
- Tai Chi: What You Need To Know. (n.d.). NCCIH. https://www.nccih.nih.gov/health/tai-chi-what-you-need-to-know#:~:text=Tai%20chi%20is%20a%20practice,on%20health%20promotion%20and%20rehabilitation.
- A., & A. (2023, January 6). Tree Pose. Yoga Journal. https://www.yogajournal.com/poses/tree-pose-2/
- Heel-toe walking – Hawkes Physiotherapy. (2020, April 16). Hawkes Physiotherapy. https://hawkesphysiotherapy.co.uk/exercise/heel-toe-walking/
- How to do Tandem Stance. (n.d.). https://www.getwellen.com/exercises/tandem-stance
- How to Do Arm Circles | Step-by-Step | Stretching and Warmups Exercises | The Gym Group. (n.d.). https://www.thegymgroup.com/exercises/stretching-and-warmups-exercises/how-to-do-arm-circles/
- D. (2021, June 8). Neck Rolls | Illustrated Exercise Guide. SPOTEBI. https://www.spotebi.com/exercise-guide/neck-rolls/
- Millard, E. (2023, September 15). How to Do Weighted Planks Safely and Effectively. BODi. https://www.beachbodyondemand.com/blog/weighted-planks
- Pridgett, T. (2019, July 29). How to Do a Plank With a Resistance Band Front Row | POPSUGAR Fitness. POPSUGAR Fitness. https://www.popsugar.com/fitness/how-do-plank-resistance-band-front-row-46384143
- Fathima, S. (2022, June 12). Best Yoga Poses for Managing Diabetic Neuropathy – Sugar.Fit. sugar.fit – Your Path Back From Diabetes. https://www.sugarfit.com/blog/yoga-for-diabetic-neuropathy/
- Miller, A. (2018, May 4). Types of Exercises with Resistance Bands – Fabrication Enterprises Retail Sales Corp. Fabrication Enterprises Retail Sales Corp. https://www.feiretail.com/types-exercises-resistance-bands/
- Gaule, C. (2017, May 23). How To Do Resistance Band Tricep Extensions For Arm Strength. Pinterest. https://www.pinterest.com/pin/333125703676755808/
- Cpt, C. F. (2016, October 24). How To Do Resistance Band Lunge With Overhead Press. Get Healthy U | Chris Freytag. https://gethealthyu.com/exercise/resistance-band-lunge/
- Alexander, A., & Alexander, A. (2022, July 14). How to Sculpt Your Body with Resistance Bands – Brick Bodies. Brick Bodies – More Than a Gym. We’re a Fitness Community. https://www.brickbodies.com/sculpt-your-body-resistance-bands/
- Lee, J. (2010, March 8). The Ultimate Resistance Band Workout. Shape. https://www.shape.com/fitness/workouts/ultimate-resistance-band-workout
- Kriplani, M. (2023, October 30). Manage your diabetes by doing the legs-up-the-wall pose for 15 minutes daily. Health shots. https://www.healthshots.com/fitness/staying-fit/yoga-for-diabetes-do-legs-up-the-wall-pose-for-15-minutes-daily/

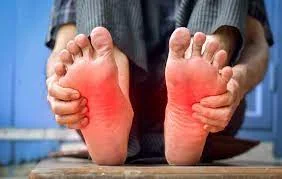
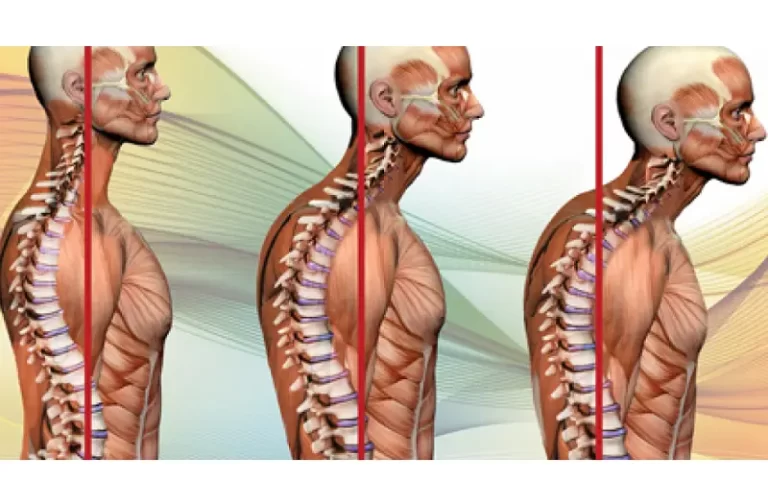




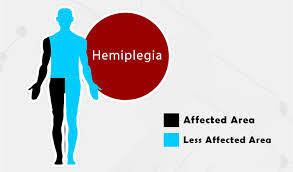
5 Comments