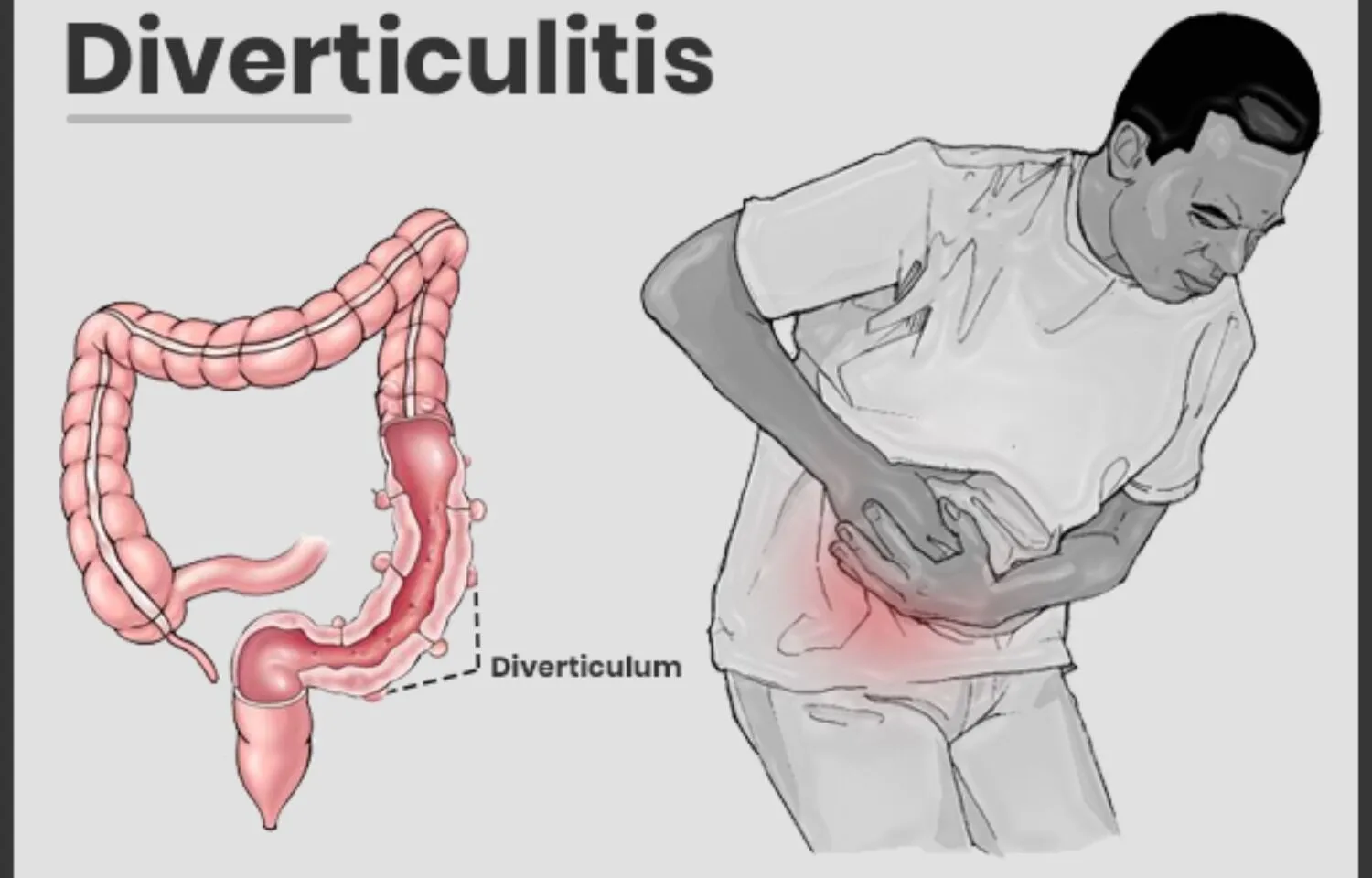
Diverticulitis
Diverticulitis can induce digestive symptoms and abdominal pain. Some individuals may develop difficulties that require urgent medical maintenance. Although it was rare before the 20th century, diverticular illness is a very common health issue in the Western world. It is a collection of disorders that can have an impact on your digestive system.
The most dangerous type of diverticular illness is diverticulitis. It can generate uncomfortable symptoms and, in some circumstances, serious complications. If left untreated, these difficulties can generate long-term health issues.
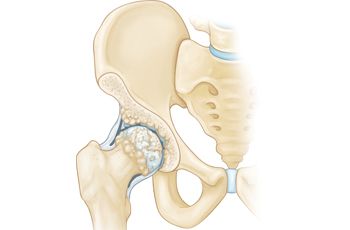
Diverticulitis is a difficulty that can impact people with diverticulosis, small pockets on the interior of their colon. If one of the pockets becomes injured or infected, it can generate inflammation inside. Diverticulitis may be the origin of a sharp pain in the lower left quadrant of your abdomen.
What is Diverticulitis?
Diverticulitis is defined as an inflammation in your diverticula, which are little pockets that can start on the inside of your colon. Having diverticula is named diverticulosis. As you age, it is to be expected, and the majority of people never experience any issues with it. On the other hand, if one of your diverticula becomes inflamed, it may cause intense pain in addition to other symptoms. It might indicate that it needs medical attention because of an infection.
Although diverticulosis is expected, diverticulitis is an uncommon complication. In 4% of persons with diverticulosis, it occurs. Once you’ve had it, your chances of having it again are 20%.
Types of Diverticulitis
Diverticulitis is categorized by practitioners as acute, chronic, complicated, or uncomplicated.
Acute/chronic
Diverticulitis starts as an acute problem, It means that it arrives on shortly and goes away shortly with medicine. However some people have frequent (repeat) episodes of diverticulitis, and some individuals experience chronic inflammation. Several theories exist regarding why this occurs. It may be because an acute episode did not recover completely, or it may be related to another chronic disease in your colon.
Complicated/uncomplicated
Many of the time, diverticulitis is uncomplicated, which means that inflammation and potential infection are the size of the issue. It recovers easily with the proper treatment. Diverticulitis becomes complicated when the inflammation starts to generate secondary issues. For illustration, severe acute inflammation may induce a diverticulum (singular of diverticula) to rupture. Chronic inflammation may cause scarring.
Causes of Diverticulitis
Inflammation in your diverticula frequently involves a tear in the lining and infection, though it is not consistently clear which came first. On one hand, diverticula make excellent hiding places for bacteria to set up camp and multiply. This can happen if, some poop gets stuck in one of them. A bacterial infection can trigger inflammation, and inflammation might generate a diverticulum to swell and tear.
In addition, if diverticulum tears for another cause, it can easily evolve infected by typical levels of bacteria living in your colon. It might tear if hard poop stretches it while passing through, or if it has been influenced by general colitis (inflammation in your colon). Diverticulitis may be caused by cytomegalovirus (CMV) infection in your colon, according to some analyses.
Although there is no single known cause of diverticular disease, many factors can enhance the risk of developing diverticulitis, including the Source:
- Genetics
- Diet
- Decreased immune function
- Having obesity
- Physical inactivity
- Smoking
- Changes in the gut microbiome
- Certain medications, such as steroids
Is Diverticulitis hereditary?
Diverticulitis seems to happen incidentally (by chance). But genetics may be partly involved in getting diverticulosis. Although you are not born with diverticulosis, you are more likely to develop it in a certain part of your colon if you are of European or Asian descent. It is also possible that genetics could influence your likelihood of creating chronic inflammation.
Symptoms of Diverticulitis
Diverticulitis can induce symptoms varying from mild to severe. These symptoms can occur suddenly, or they can develop slowly over several days.
Potential symptoms of diverticular illness include
- Bloating
- Constipation
- constant or severe pain in your abdomen
- Nausea and vomiting
- fever and chills
- Blood in your stool
- Bleeding from your rectum
- Palpable colon or an enlarged abdomen (you can feel it with your hand).
- Constipation or, less commonly, diarrhea.
Abdominal pain is the most typical symptom of diverticulitis. It will most likely appear in the lower left side of your abdomen. It can also grow on the right side of your abdomen.
If you develop any of the above symptoms, it may be a sign of serious difficulty from diverticulitis or another condition.

How does Diverticulitis feel when it attacks or flares up?
The discomfort will be the same whether you are experiencing an acute diverticulitis attack or a flare-up of chronic diverticulitis. An acute episode may come on short, while a chronic flare-up may build up over a few days. You should be able to find it in the exact spot where your diverticulum has become inflamed. It could have a burning sensation or feel biting and sharp. The discomfort is typically mild to severe.
Where is Diverticulitis pain located?
In people of European descent, diverticula most usually occurs in the last part of the colon, named the sigmoid colon. This region originates on the lower left side of your body and curves just a bit to the right to meet your rectum. The lower left quadrant of the abdomen is where most people experience pain from diverticulitis due to this reason. Sometimes, lower abdominal pain may also extend to your pelvis or radiate to your back.
However, in people of Asian descent, it is more common to have diverticulosis in the first part of the colon, which is in the upper right quadrant. Diverticulitis here might generate upper abdominal pain.
Possible complications of Diverticulitis:
Diverticulitis is uncomplicated 85% of the time. But severe or constant diverticulitis can lead to difficulties such as:
- Gastrointestinal bleeding: Bleeding from diverticula can be severe and guide to anemia.
- Intestinal obstruction: Painful swelling might cause your colon to temporarily narrow. Chronic swelling might cause scarring (stricture), which can generate more permanent narrowing.
- Fistulas. An inflamed and eroded colon wall might fuse to another body canal (such as your small intestine, bladder, or vagina), making an inappropriate tunnel between the two.
- Bladder inflammation: Diverticulitis that is close to your bladder may cross it. A fistula to your bladder may also extend an infection there.
- Abscess: An abscess is a pocket of infected pus that may require to be drained. It may rupture and cause peritonitis, an infection of the peritoneal cavity. This is an emergency.
- Gastrointestinal perforation: If a diverticulum swelled enough to rupture (tear), it could allow intestinal bacteria to leak into your peritoneal cavity. Peritonitis can lead to sepsis.
What are the signs of complicated diverticulitis?
You may have created complications if you notice:
- Fresh blood in your stool.
- Paleness in your face or you feel lethargy.
- You feel like you need to pee repeatedly or irritation when you urine.
- Your belly is rigid and susceptible to touch.
Diagnosis and tests:
To analyze diverticulitis, your physician will likely ask about your symptoms, fitness history, and any medicines you take. They will likely perform a physical exam to check your abdomen for tenderness.
A digital rectal exam could be used if more information is required to look for the following things:
- Stool bleeding
- Pain
- Masses
- Other issues
Several other diseases can generate symptoms that are similar to diverticulitis. To lead out other conditions and check for signs of diverticulitis, your doctor might order one or more tests.
Tests can include:
- abdominal ultrasound, abdominal MRI scan, abdominal CT scan, or abdominal X-ray to take pictures of your gastrointestinal (GI) tract
- colonoscopy to inspect the inside of your GI tract; although this takes place after a bout of diverticulosis
- stool test to scan for infections, such as Clostridium difficile (C. diff)
- urine test to scan for diseases
- Blood tests to inspect for signs of inflammation, anemia, or kidney or liver issues
- pelvic exam to rule out gynecological issues in people assigned female at birth
- Pregnancy test to rule out pregnancy in those who were born with a female gender.
If you have diverticulitis, these exams and tests can assist your doctor in learning if it’s uncomplicated or complicated.
Using a colonoscopy to diagnose diverticulitis
If you have signs of diverticulitis, your physician may encourage you to have a colonoscopy once the acute attack resolves. This technique can assist in establishing a diagnosis of diverticulitis or another disease that generates similar symptoms, such as ulcerative colitis or Crohn’s disease.
During a colonoscopy, your physician will thread a flexible scope into your rectum and colon. They can utilize this scope to investigate the interior of your colon. They can also utilize it to collect tissue specimens for testing.
To help you feel more comfortable during this procedure, you will be sedated before the procedure.
In certain cases, a normal colonoscopy can identify diverticula to your doctor. If the diverticula is not inflamed, contaminated, or inducing symptoms, you likely would not require therapy.
Treatment of Diverticulitis
The medicine that your doctor prescribes for diverticulitis will depend on how severe your situation is.
Uncomplicated diverticulitis can generally be treated at home. Your physician might encourage you to make changes to your diet. In some cases, they might specify medications, including antibiotics.
If you create complications from diverticulitis, you may be required to visit a hospital for treatment. Through an intravenous (IV) line, fluids and antibiotics may be administered to you. Depending on the type of complication, you might be required to undergo surgery or another method.
- Diet and diverticulitis
There are no particular meals that everyone with diverticulitis has to ignore. However, you may find that particular foods make your condition better or more dangerous.
As your symptoms enhance, your physician might stimulate you to eat more high-fiber foods. Some studies have linked high-fiber diets to reduced risk of diverticulitis. Other studies have examined the possible benefits of dietary or supplemental fiber for diverticular disease but are still unsure of the role fiber should play.
Your physician might also encourage you to limit your consumption of red meat, high-fat dairy items, and refined grain products. According to a significant cohort study, those who consume a diet packed with such foods had a higher risk of developing diverticulitis than those who consume a diet high in fruits, vegetables, and whole grains.
Diverticulitis management and your general digestive health can also be influenced by your diet. Learn more about some of the foods that may have an impact on your symptoms.
Your doctor might advise avoiding eating solid foods and sticking to a clear liquid diet for a few days to give your digestive system a chance to relax and recover.
You might be allowed to attempt eating low-fiber foods up until your condition improves if your symptoms are mild or have started to get better. Your doctor might advise you to include additional high-fiber foods in your meals and snacks as your situation gets better.
- Medication
Your doctor may advise taking acetaminophen (Tylenol) or other over-the-counter pain relievers to lessen diverticulitis-related pain or discomfort.
The most likely course of action if they think you have an infection is for them to recommend antibiotics. These may consist of:
- metronidazole (Flagyl, Flagyl ER)
- amoxicillin
- moxifloxacin
Even if your symptoms disappear after the first few doses of your recommended antibiotics, it’s essential to finish the entire course.
Other procedures
Your doctor can suggest one of the following treatments if you have a serious case of diverticulitis that can’t be cured with diet and medicine alone:
- Needle drainage. A needle is placed into your abdomen during the procedure to drain a pus-filled abscess.
- Surgery. Surgery may implicate the removal of infected sections of the colon, the closure of a fistula, or the drainage of a pus-filled abscess.
Surgery
Your doctor may advise surgery if you get diverticulitis multiple times and the disease cannot be properly treated with changes to your diet and medicines. Diverticulitis-related problems can sometimes be treated surgically.
Diverticulitis is frequently treated with one of two different forms of surgery.
Bowel resection with anastomosis
A surgeon performs a bowel resection with anastomosis during which contaminated colon parts are cut out and healthy segments are sewn back together.
Bowel resection with colostomy
A bowel resection with colostomy includes surgeons cutting out the infected portions of your colon and joining the healthy portion of the colon to an incision in your belly called a stoma.
Both treatments can be carried out laparoscopically or openly.
Can Diverticulitis go away on its own?
If the illness is simple and moderate, it might go away by itself. However, you should still have it assessed by a medical professional. If you have an infection, they could need to give you antibiotics, and some people might require prescription painkillers. During your recovery, your healthcare professional will also instruct you on how to take care of yourself at home. It requires roughly a week. Throughout this time, they’ll want to stay in touch with you.
Home remedies for Diverticulitis
The majority of home treatments for diverticulitis focus on diet modifications, but there are a few other approaches that may help with symptoms and digestive health.
Several natural treatments for diverticulitis include:
- Probiotics. Although additional research is required, several studies have suggested that specific probiotic strains may aid in reducing or preventing diverticulitis symptoms.
- Aromatherapy. It has been demonstrated that some essential oils can lessen pain, which may help you manage your symptoms.
- Acupuncture. Acupuncture can help with Source’s chronic pain as well as digestive problems including constipation, according to certain studies.
- Herbs. Several herbs such as rosemary, ginger, and turmeric, have potent anti-inflammatory qualities. To explicitly assess these herbs’ effects on diverticulitis, more study is required.
- A liquid diet. Your bowels will have a chance to rest and heal from the sickness if you stay away from solid foods. You can receive more detailed advice on when and what to eat from your healthcare professional
- Prescription antibiotics. Although it’s possible that you won’t require any, if you do, your provider will give you some to take home with you. Your infection’s type will determine the type.
- Acetaminophen. The best choice for over-the-counter (OTC) pain management is acetaminophen (Tylenol®). Your risk of gastrointestinal (GI) bleeding may rise if you also take other common painkillers.
Drugs to avoid in Diverticulitis
When you have diverticulitis, medical professionals advise against taking NSAIDs since they can increase your risk of bleeding.NSAIDS is an abbreviation for nonsteroidal antiinflammatory drugs.
for example.
Aspirin (Bayer® or St. Joseph®), for example.
Advil® or Motrin® (ibuprofen).
sodium naproxen (Aleve®).
What happens if Diverticulitis goes untreated?
If your condition is minor and simple, therapy might not be necessary. To get help for diverticulitis, however, you need to visit a doctor. If you don’t, your situation can worsen and become more problematic. Antibiotics or antivirals might be necessary to cure some infections. Chronic inflammation may start to result in further issues. Another possibility for pain is an increase.
How do you get Diverticulitis to go away?
You might need to stay in the hospital for treatment if conservative at-home treatment has failed, or if you have severe, persistent, or complicated diverticulitis. Treatment options include:
- IV medication. Your doctor may provide antibiotics or antivirals intravenously (IV) so that the medication enters your bloodstream immediately. You might also get pain alleviation in this method. Opioids are powerful analgesics that certain people may require.
- Blood transfusion. A blood transfusion may be required in an emergency if you have lost a significant amount of blood due to bleeding from a diverticulum.
- Endoscopic procedures. To cure mild issues, your doctor might employ a colonoscope or sigmoidoscope, two endoscope varieties that look into your colon. For instance, they frequently use equipment delivered via the endoscope to stop active bleeding, drain an abscess, or widen a narrowed portion of your colon.
- Surgery. To treat an abscess, ongoing bleeding, perforation (tear), or fistula, certain patients may require surgery. Rarely, persons with chronic diverticulitis may require a colectomy, which involves removing the painful portion of the colon. This might necessitate a transient colostomy.
Risk factors for Diverticulitis
- To determine the causes of diverticular disorders like diverticulitis, more research is required. Currently, analysts think several elements are involved. It is to Age is a significant risk factor for diverticulitis. Men under 50 and women between the ages of 50 and 70 are both at risk.
- Compared to younger persons, older adults have a greater risk of diverticulitis. In addition, younger people are more likely than older persons to be hospitalized for diverticulitis.
- Other possible risk factors for diverticulitis include the following, according to a review of research published in 2018:
Family history
To determine the causes of diverticular disorders like diverticulitis, more research is required. Currently, analysts think several elements are involved. It is to Diverticular disease is genetically predisposed, according to studies; some estimates place the hereditary component of the chance of developing diverticular disease at between 40 and 50 percent.
Low levels of vitamin D
Some investigations indicate that people with higher levels of vitamin D might have a lower risk of acquiring diverticulitis. More study is required to understand the potential link between vitamin D and diverticula.
Obesity
Diverticulitis risk increases with higher body mass index (BMI) and wider waists, according to several studies. To Calculate BMI Click Here.
More research is required to fully understand how obesity affects the balance of bacteria in the gut and how this affects diverticulitis risk.
Physical inactivity
Diverticulitis is less common in physically active people than in inactive people, according to certain research. Research on this connection is still needed, though.
Using nonsteroidal anti-inflammatory drugs (NSAIDs) or smoking
Your risk of diverticulitis may increase if you regularly take aspirin, ibuprofen, or other NSAIDs.
Smokers have a higher risk of developing diverticular disease, including diverticulitis, than non-smokers do.
There isn’t sufficient evidence that drinking alcohol increases your likelihood of developing this condition, according to a 2017 Research Source study.
If you use alcohol, your doctor probably advises you to do so only occasionally and in moderation. Even though diverticulitis may not be caused by alcohol, drinking excessively might increase your risk for a variety of other health issues.
Diverticulitis vs. diverticulosis
Diverticulosis is the medical term for diverticula that aren’t diseased or inflamed.
Diverticulosis sometimes manifests as symptoms including abdominal pain and bloating. The term “symptomatic uncomplicated diverticular disease” (SUDD) is used to describe this situation.
Diverticulitis is defined as an inflammation in your diverticula, which are little pockets that can start on the inside of your colon. Having diverticula is named diverticulosis. It is expected as you get older, and most people never have any problems with it.
Other forms of Diverticulitis
Your bladder has a risk of developing diverticula. This occurs when weak places in the bladder wall are penetrated by pouches formed by the bladder lining.
Diverticula in the bladder may be seen at birth. Other times, they come into being later in life. When your bladder outlet is obstructed or your bladder isn’t functioning properly as a result of a disease or accident, they may form.
Bladder diverticulitis is the medical term for an irritated bladder diverticulum. Your doctor might suggest antibiotics and painkillers to treat bladder diverticulitis. They might advise having the diverticula repaired surgically as well.
Diverticulitis in your colon may also have an impact on your bladder. In extreme circumstances, a fistula between your colon and bladder may form.
Your esophagus has the potential to develop diverticula as well. When pouches form in the lining of your esophagus, this happens.
Diverticula in the esophagus are uncommon. When they do develop, it usually takes a long time and is done slowly. As they mature, they may result in signs or issues like:
- Problem swallowing
- Discomfort when swallowing
- Halitosis, or foul breath
- Regurgitation of meals and saliva
- Pulmonary aspiration: breathing reiterated food or saliva into your lungs
- Aspiration pneumonia: acquiring a lung infection after breathing in food or saliva
Esophageal diverticulitis is the medical term for a diverticulum that has become inflamed.
Your doctor may advise antibiotics and analgesics to treat esophageal diverticulitis. They might advise having the diverticula repaired surgically.
Here we describe other different types of diverticulitis:
Meckel’s Diverticulitis
Adults are generally affected by diverticular illness. Diverticula are sometimes present at birth in newborns. It is referred to as Meckel’s diverticulum when this occurs.
Meckel’s diverticulum occasionally has no apparent effects. It can result in symptoms in other situations.
- stomach discomfort
- Nausea
- Bleeding from the rectum
- vomiting
- Bloody stool
Make an appointment with their doctor if you think your child may have diverticulitis.
Preventing Diverticulitis
- By altering one’s lifestyle, several possible risk factors may be reduced.
- To determine the causes of diverticular disorders like diverticulitis, more research is required.
- Currently, analysts think several elements are involved.
- Try to keep a moderate body weight
- Eat a diet that is high in fiber to help bulk up stools (however, in acute diverticulitis, you may like to avoid fiber)
- Restrict your consumption of saturated fat
- Get sufficient vitamin D
- Get routine exercise if possible
- Try to avoid cigarette smoke
These prevention techniques can also help facilitate good overall health.
Prognosis
Fewer than 1% of patients will have complex diverticulitis, and fewer than 1% of those will require surgery. Even complicated diverticulitis usually gets better quickly and completely with treatment. Your total life expectancy shouldn’t be impacted by diverticulitis. You wouldn’t be that danger of developing potentially fatal complications unless your gut were to rupture or you experienced a perforation.
What should I do if my Diverticulitis recurs?
There may be more factors at play that increase your risk if dietary and lifestyle changes haven’t stopped diverticulitis from recurring. Immune systems that are compromised are more vulnerable to infections and heal more slowly in patients. Chronic inflammation is more common in those who suffer from autoimmune illnesses. Your gut immunity may even be impacted by the diversity of bacteria that live there.
Diverticulitis may return in certain patients for unknown reasons, according to healthcare professionals. However, if it comes back more than once and causes issues at least once, they may suggest an elective intestinal resection to fix it. That involves getting rid of the brief problematic segment of your colon. You can likely perform this surgery in one stage without a colostomy if there is not an emergency.
Note on diverticulitis:
In Western countries, diverticulitis is a common condition. Most of the time, it is curable with short-term dietary adjustments and medicines.
If problems arise, they can be very serious. In the case that you have complicated diverticulitis, your doctor will probably suggest that you receive care in a hospital. If your colon has been damaged, surgery may be required to repair it.
Consult your doctor if you have diverticulitis or concerns about your risk of getting it. They can support your digestive health and assist you in learning how to address this illness.
FAQ
What is the main cause of diverticulitis?
Diverticula, known as tiny bulges in the large intestine, can form and enlarge to produce diverticular illness. Diverticulitis symptoms appear if any of the diverticula get infected. The exact reason why diverticula develop is not known, but they are associated with not eating enough fiber.
What does a diverticulitis attack feel like?
The most typical sign of diverticulitis is abdominal or stomach pain. The most typical symptom of it is feeling sensitive or sore on the left side of your lower abdomen. If an infection is the root of your symptoms, you may also have a high body temperature, chills, nausea, vomiting, cramps, and constipation.
Do people with diverticulosis or diverticulitis have to follow any dietary restrictions?
In the past, people with diverticulosis were told to avoid seeds and nuts, in case they might get stuck in a diverticulum and cause diverticulitis. Today, most people believe that this worry is unnecessary. As excellent sources of fibre and plant-based protein, seeds, and nuts frequently exist in balanced diets. Your bowels should maintain a healthy diet overall rather than worrying about the rare chance of seed going wrong.
How is diverticulitis diagnosed?
The most accurate method used by clinicians to identify diverticular illness is an abdominal CT scan. Cross-sectional, two-dimensional, and three-dimensional pictures of the structures in the gastrointestinal system are provided by a CT scan.
How can I cure diverticulitis?
Dietary and lifestyle changes are the most effective method to cure diverticulitis. Here are some tips: Eat more fiber by adding whole-grain bread, oatmeal, bran cereals, fibrous fresh fruits, and vegetables to your diet. But be sure to incorporate fiber gradually.
Is diverticulitis curable without surgery?
Many people who experience these symptoms delay seeking care because they’re embarrassed, or they fear that gastrointestinal surgery with a colostomy pouch will be their only therapy option. However, with the right medications and dietary modifications, the majority of diverticulitis patients can manage their symptoms.
What is the most suitable antibiotic for diverticulitis?
If antibiotics are given for uncomplicated diverticulitis, consider amoxicillin/clavulanic acid or an oral cephalosporin plus metronidazole if the patient can take oral treatment. If intravenous therapy is needed cefazolin, cefuroxime, or ceftriaxone, all plus metronidazole or ampicillin/sulbactam alone can be used.
What deficiency causes diverticulitis?
Low levels of serum vitamin D (25-OH D) are a risk factor for diverticular disease, which may contribute to the emergence of diverticulitis. Similar links exist between low vitamin D levels and other inflammatory diseases like Crohn’s disease.
What is the earlier noticed symptoms of diverticulitis?
Common signs of diverticulitis include Abdominal cramping. Abdominal bloating, pain, and tenderness. Chills and/or fever.
Is diverticulitis permanent or temporary?
Diverticulitis typically reacts well to non-invasive therapies, such as short changes in diet as well as antibiotics. Most people with diverticulitis recover completely. At its worst, a pouch could rupture and leak feces directly into a person’s bloodstream.
References
- Professional, C. C. M. (n.d.-b). Diverticulitis. Cleveland Clinic.
- Persons, L. (2023b, February 7). Everything you need to know about diverticulitis. Healthline.
- Diverticulitis – Symptoms and causes – Mayo Clinic. (2022, April 19). Mayo Clinic.
- Diverticulitis. (2001, December 31). WebMD.