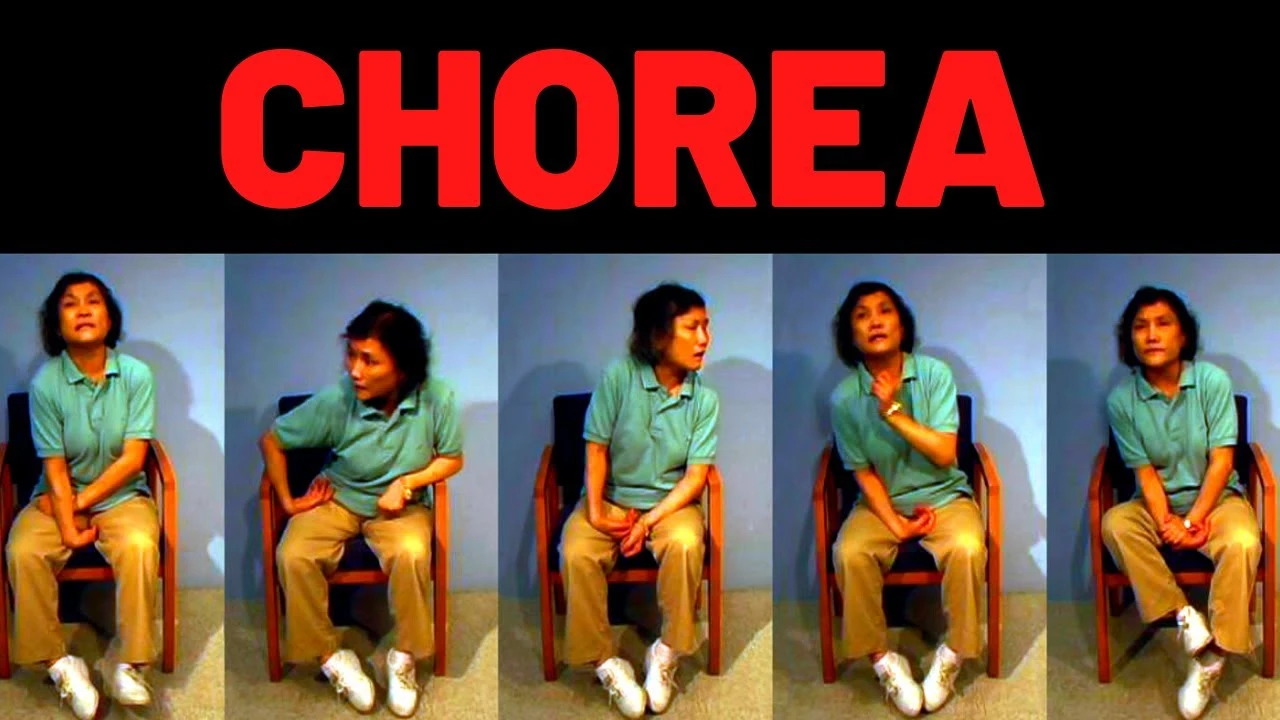
Chorea
What is Chorea?
Chorea stands as a distinctive movement disorder characterized by involuntary, irregular, and unpredictable muscle movements. This condition can give rise to a semblance of dancing (the term ‘chorea’ is derived from the Greek word for ‘dance’) or manifest as restlessness and fidgetiness.
Chorea, essentially a motor malfunction, finds its manifestation across various diseases and conditions. While chorea itself might not pose an immediate threat to life, it could potentially serve as a red flag for an underlying neurological ailment, such as Huntington’s disease. Medical practitioners have the capacity to prescribe medications that aim to regulate these abnormal muscle movements. The persistence and progression of chorea depend on the root cause, which might result in either transient or chronic symptoms.
In addition to chorea, two other movement anomalies often correlate with neurological disorders.
Athetosis involves an unceasing flow of slow, contorted, and writhing-like motions, primarily affecting the hands and feet.
Ballismus, on the other hand, tends to manifest as more vigorous movements, including sudden and forceful flinging of an arm or leg. These movements typically impact only one side of the body (known as hemiballism).
How common is Chorea?
The exact prevalence of chorea remains elusive. Typically, chorea presents itself as a symptom intertwined with other underlying disorders. Within the United States, approximately 30,000 individuals grapple with Huntington’s disease an inherited genetic condition notorious for inciting choreic movements. An additional 200,000 individuals are believed to carry a risk of developing Huntington’s disease due to their parental genetic inheritance. Remarkably, chorea stands as the prevailing symptom associated with Huntington’s disease.
In the context of the United States, the emergence of Sydenham chorea is observed in roughly 4,000 children each year, subsequent to their battle with rheumatic fever. Rheumatic fever, a grave complication stemming from untreated strep throat, serves as the precursor to this choreiform condition. Notably, rheumatic fever tends to affect girls more frequently than boys, with its occurrence typically falling within the age range of 5 to 15 years.
Who is affected by the Chorea?
Chorea can manifest across all age groups, although specific demographics carry an elevated risk, including:
Individuals with a familial history of Huntington’s disease: In cases where a parent has Huntington’s disease, there exists a 50% likelihood of inheriting the condition. Typically, symptoms of Huntington’s disease emerge between the ages of 40 and 50. This ailment stands as the most prevalent hereditary form of chorea.
Children and adolescents who have experienced rheumatic fever: Following an episode of untreated strep throat, young individuals are susceptible to developing Sydenham chorea. This condition arises as a complication of rheumatic fever.
Individuals with other medical conditions: Autoimmune disorders like lupus, hormonal imbalances such as hyperthyroidism, and metabolic irregularities like hypoglycemia can all trigger chorea. Notably, a diverse range of disorders exists within this category, capable of inducing choreiform movements.
Symptoms and Causes of Chorea
How do people get chorea?
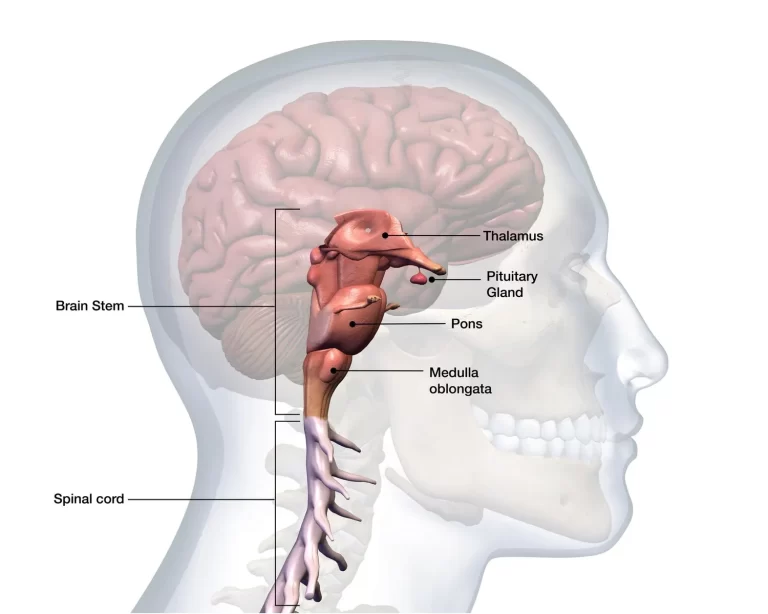
Chorea emerges as a neurological manifestation rooted in a region of the brain known as the basal ganglia, a cluster of nerve cells located deep within the brain responsible for regulating movement. An array of genetic disorders, autoimmune conditions, metabolic anomalies, infections, and medications can impinge upon the basal ganglia, thus precipitating the onset of choreic movements.
Predominant catalysts of chorea encompass:
- Huntington’s Disease: Inherited genetically, this disorder brings about not only chorea but also changes in personality, speech impairment, coordination difficulties, and memory issues. Symptoms of Huntington’s disease progressively worsen over a span of 10 to 20 years.
- Rheumatic Fever: Following rheumatic fever, Sydenham chorea, colloquially known as St. Vitus dance, can arise within one to eight months. Rheumatic fever, a complication of group A streptococcal infection like untreated strep throat, underpins this condition. In most instances, children with Sydenham chorea experience spontaneous recovery within two years.
- Infectious Diseases (Rarely): Lyme disease, toxoplasmosis, HIV/AIDS, endocarditis, syphilis, encephalitis, meningitis, Legionnaire disease, and Creutzfeldt-Jakob disease are among the infectious triggers capable of inducing chorea.
- Autoimmune Diseases: Chorea can materialize in individuals with systemic lupus erythematosus (lupus), multiple sclerosis, sarcoidosis, Sjogren syndrome, and Behcet disease, representing only a subset of autoimmune conditions capable of engendering choreic movements.
- Stroke: Some individuals may develop chorea subsequent to experiencing a stroke or when confronted with a basal ganglia-adjacent tumor.
- Pregnancy: A rare manifestation named chorea gravidarum can manifest during pregnancy, typically within the initial three months, and tends to abate shortly after childbirth.
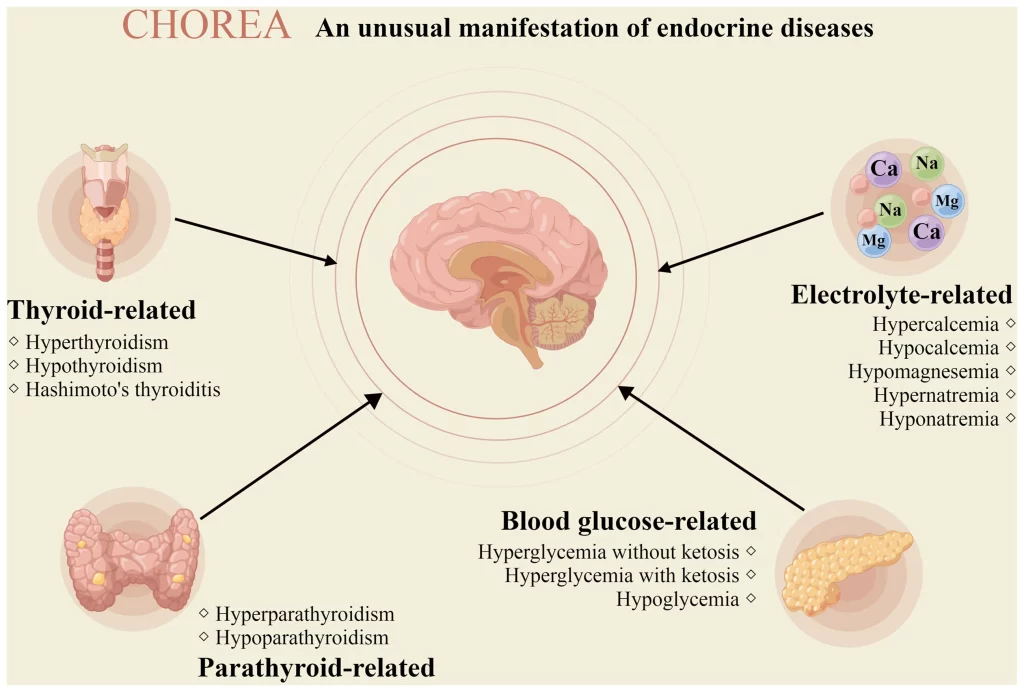
- Endocrine and Metabolic Disorders: Hypoglycemia, hyperglycemia, hyperthyroidism, hypoparathyroidism, hyperparathyroidism, hyponatremia, hypernatremia, hypocalcemia, hypomagnesemia, polycythemia vera, and hepatic failure are among the conditions with the potential to trigger chorea.
- Medications: Chorea might be a damaging consequence of medications for example levodopa, antihistamines, neuroleptics, tricyclic antidepressants, amphetamines, anticonvulsants, cocaine, & oral contraceptives. Antipsychotic drugs can also lead to chorea as a component of tardive dyskinesia.
- Toxins: Chorea can result from exposure to toxins such as carbon monoxide, mercury, and alcohol.
- Advanced Age: Senile chorea, which primarily affects the muscles around the mouth, may occur in older individuals without a discernible cause.
These myriad factors contribute to the intricate tapestry of chorea’s origins and manifestations within the realm of neurological health.
Acquired Causes
| Levodopa Cocaine Amphetamine Anticonvulsants Lithium Anticholinergics Neuroleptic withdrawal | Vascular causes Tumors Demyelinating lesion |
| Metabolic | Nonketonic hyperglycemia Hypoglycemia Hypocalcemia Hyponatremia Uremia Hyperthyroidism Acquired Hepatocarebral degeneration Hypoparathyroidism/Hyperparathyroidism |
| Infectious | Toxoplasmosis HIV encephalopathy Prion disease |
| Drug Included | Levodopa Cocaine Amphetamine Anticonvulsants Lithium Anticholinergics Neuroleptic withdrawal |
| Autoimmune | Sydenham chorea Rheumatologic disease Autoimmune neurologic syndromes |
| Others | Polycythemia vera Postpump chorea |
Genetic Causes
| Huntington disease | |
| C9orf72 disease | |
| SCA17 (HDL-4) | |
| Huntington disease like-2 | |
| Neuroacanthocytosis syndroms | Chorea acanthocytosis McLeod syndrome |
| Dentatorubral Pallidolusian palsy | |
| Neurodegeneration with brain accumulation | Neuroferritinopathy Aceruloplasminemia |
| Choreoathetoid cerebral palsy | |
| Benign hereditary chorea syndrome | Classic benign hereditary chorea syndrome ADCY5-related dyskinesia |
| Wilson disease | |
| Autosomal recessive ataxia | Friedreich Ataxia Ataxia with oculomotor apraxia type-1 (AOA-1) Ataxia with oculomotor apraxia type-2 (AOA-2) |
| Metabolic disorder | |
| Mitochondrial disorder |
What are the symptoms of chorea?
The symptoms of chorea remain largely consistent regardless of the underlying cause of this movement disorder. The primary indications of chorea encompass:
- Involuntary Muscle Movements: Characterized as fidgety or dance-like motions, these movements predominantly manifest in the hands, feet, and facial regions. They can impact your gait, swallowing, and speech patterns. The movements may exhibit a fluid quality or display a slightly jerky nature. They can give the appearance of dancing, playing a musical instrument, or even experiencing discomfort. Stress or anxiety can exacerbate these movements, whereas they tend to subside during sleep.
- Milkmaid’s Grip: When attempting to shake someone’s hand, you might repeatedly grip and release your fingers, rather than maintaining a steady hold. This phenomenon is termed milkmaid’s grip due to its resemblance to milking actions.
- Jack-in-the-Box Tongue: Your tongue may exhibit a sliding in-and-out motion when you try to extend it, akin to a jack-in-the-box mechanism. This particular sign of chorea is occasionally referred to as jack-in-the-box tongue or harlequin tongue.
- Speech Impediments: Both children and adults could experience slurred speech as the coordination among the muscles involved in articulation becomes compromised.
- Headaches and Seizures: In the context of children who develop chorea subsequent to rheumatic fever, seizures, and headaches can emerge. Behavioral and emotional challenges might also arise in some cases.
These telltale signs collectively paint a picture of Chorea’s distinctive presence, regardless of its causal origins. The intricate dance of involuntary movements, coupled with distinctive speech anomalies, provides a window into this intricate neurological phenomenon.
Phenomenological Features of Chorea
- Randomness
- Flowing Quality
- Parakinesia: Individuals intertwine their chorea-induced movements with their inherent regular movements.
- Motor Instability: The patient encounters difficulty in maintaining continuous motor actions.
- Ballism: A distinctive chorea subtype marked by expansive, forceful flinging movements involving the proximal limbs.
- Athetosis: Gradual, undulating motions affecting the distal extremities, occasionally displaying a contorted aspect.
- Variability in Movement Speed: Oscillation between rapid, low-amplitude movements and sudden jerks, forming a unique dynamism.
Diagnosis
The mentioned phenomenological attributes serve as key criteria for diagnosing chorea.
Given the diverse range of conditions and disorders that can potentially trigger chorea, your physician will delve into a comprehensive inquiry encompassing your family medical history, ongoing medication regimen, and any concurrent symptoms beyond uncontrollable movements. A thorough physical examination will be conducted, coupled with inquiries about the frequency, duration, and potential exacerbation of involuntary muscle movements during periods of stress.
To pinpoint the underlying cause of chorea, your healthcare provider might recommend:
- Blood Tests: These assessments can reveal infections, lupus, thyroid irregularities, or other endocrine/metabolic anomalies.
- Imaging Studies: Utilizing techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, clinicians can scrutinize brain changes that might correlate with chorea.
- Genetic Testing: In cases where Huntington’s disease is suspected, genetic testing can ascertain the presence of the disease-associated gene.
Differential Diagnosis:
Distinct diagnoses can be established based on the unique symptomatology and clinical characteristics exhibited by the patient. Notable differential diagnoses encompass:
- Huntington’s Disease
- Lyme Disease
- Multiple System Atrophy
- Neuroacanthocytosis
- Pediatric Torticollis Syndrome
- Ramsay Hunt Syndrome
- Striatonigral Degeneration
- Tourette Syndrome
- Viral Encephalitis
Multimodal Management
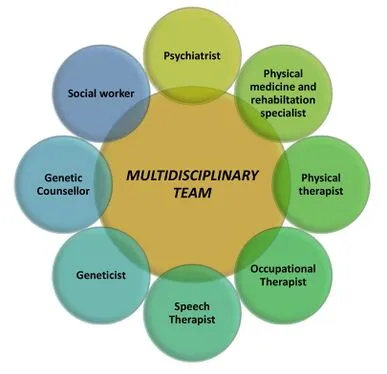
Effectively managing chorea demands a comprehensive multidisciplinary approach, uniting an array of specialists:
- Psychiatrist
- Specialist in Physical Medicine and Rehabilitation
- Physical Therapist
- Occupational Therapist
- Speech Therapists
- Geneticist
- Genetic Counselor
- Social Worker
Medical Management
While a definitive cure remains elusive, the disease can be managed through symptom control. An integral aspect involves evaluating and establishing a robust support network for the patient. As the condition advances, specialized care becomes increasingly vital. Nutrition management assumes particular significance due to difficulties in swallowing.
To address the symptoms, various medical interventions can be employed:
- Dopamine-Depleting Agents: Notable examples include Tetrabenazine and Deutetrabenazine.
- Dopamine D2 Receptor-Blocking Agents: Options such as Haloperidol, Clozapine, and Olanzapine.
- Anticonvulsants: Valproic Acid, Carbamazepine, Benzodiazepines, and Levetiracetam.
- Anti-Glutamatergic Agents: Utilizing substances like Amantadine and Riluzole.
- Cannabinoids: Incorporating compounds like Nabilone.
- Deep Brain Stimulation: A treatment modality that holds promise in managing chorea’s effects on the brain.
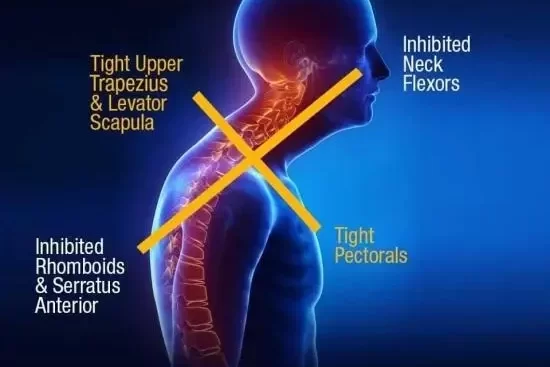
Physiotherapy Management
The approach to management closely mirrors that employed for Huntington’s Disease.
Objectives of Management
- Gait Rehabilitation: Re-educating and refining gait patterns.
- Balance Retraining: Enhancing balance control and stability.
- Fall Prevention and Management: Strategies to minimize and address falls.
- Enhancing Aerobic Capacity: Focusing on cardiovascular fitness.
- Muscle Strengthening: Targeted exercises to bolster muscle strength.
- Wheelchair Prescription and Training: Customizing wheelchair solutions and imparting necessary training.
- Optimizing Respiratory Function: Strategies to improve respiratory capacity.
- Task-Specific Reach, Grasp, and Manipulation: Tailored interventions to enhance fine motor skills and manipulation abilities.
Prognosis of Chorea?
The prognosis hinges upon the underlying cause of the involuntary muscle movements. For those grappling with Huntington’s disease, life expectancy post-symptom onset spans between 15 to 25 years. Over time, this condition undergoes a gradual deterioration, significantly impeding routine tasks such as dressing, bathing, and eating.
Children afflicted with Sydenham chorea following rheumatic fever generally witness recovery within a span of two years. Nonetheless, certain individuals might contend with persistent behavioral or emotional challenges, including conditions like obsessive-compulsive disorder (OCD), which could extend throughout their lifetime.
Remarkably, chorea itself typically lends itself to effective management through currently available treatments. This provides hope for improved symptom control and enhanced quality of life for affected individuals.
FAQ
What are the symptoms of chorea?
Activity signs contain non-suppressible, jerky, non-rhythmic, involuntary motions (chorea), & maintained spontaneous contractions conducting to abnormal postures (dystonia). Mental signs contain a deficiency of stimulation management, which can result in explosions/a decrease in reasoning capabilities.
What are the types of chorea?
Chorea is generally categorized as existing primary (idiopathic, hereditary)/secondary (acquired). Genetic choreiform disorders supervise to evolve insidiously & are commonly symmetrical, whereas acquired chorea are more probable to be acute and subacute & can be asymmetrical/unilateral.
What is the difference between chorea and ataxia?
Chorea & ataxia can both impact muscle activities, but chorea provokes involuntary motions, while ataxia induces inadequate coordination. The spontaneous gestures associated with ataxia frequently result in slurred speech, stumbling, lack of coordination, & falling.
What is the first-line treatment for chorea?
The most largely utilized agencies in the remedy of chorea are neuroleptics. The basis of their mechanism of movement is considered to be connected to the blockade of dopamine receptors. Neuroleptics can be categorized as typical & atypical. Typical neuroleptics contain haloperidol & fluphenazine.
What is the difference between chorea and tremor?
Chorea is determined from tremor by it is absence of rhythmicity & predictability. Chorea is defined from myoclonus by the validity that in myoclonus all the actions are quick, whereas in chorea.