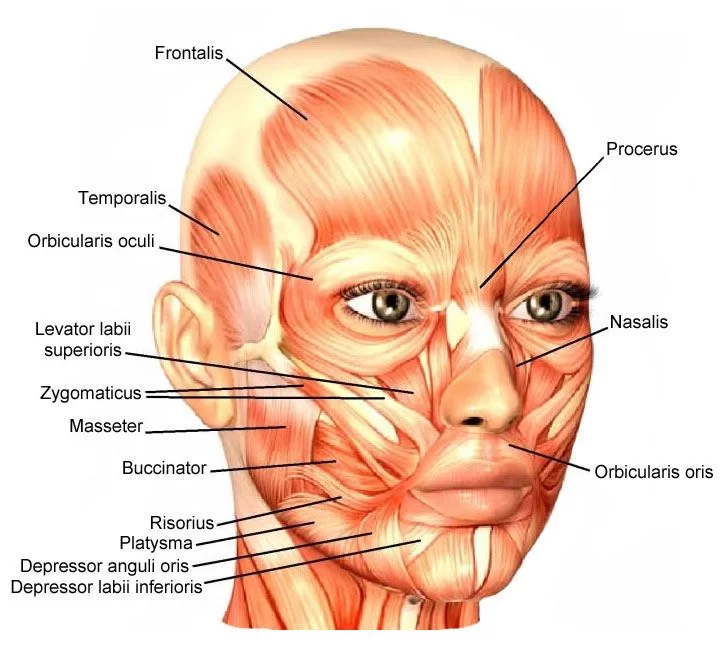
Facial Muscle List
Facial Muscle Anatomy
The facial muscles, also called craniofacial muscles, are a group of about 20 flat skeletal muscles, lying underneath the skin of the face and scalp.
The muscles of facial expression (also known as the mimetic muscles) can generally be divided into three main functional categories: orbital, nasal, and oral. Contrary to the other skeletal muscles they are not surrounded by a fascia, with the exception of the buccinator muscle.
The facial muscles are positioned around facial openings ( mouth, eye, nose, and ear ) or stretch across the skull and neck.
These muscles are all innervated by the 7th Cranial nerve – facial nerve (CN VII).
The facial muscles have different characteristics compared to muscles in the trunk and limbs:
- They have a more complex pattern of innervation of extrafusal fibres
- They have a larger percentage of slow-type nerve fibres
- Many facial muscles insert not into bone or fascia, but into the skin
- Many facial muscles are very thin in structure and are poorly differentiated, merging with other facial muscles
There is a total of eleven facial muscles that create movement at the mouth and their functions include:
Lifting up and everting the upper lip: levator labii superioris, levator labii superioris alaeque nasi, risorius, levator anguli oris, zygomaticus major and zygomaticus minor muscles.
Lowering and everting the lower lip: depressor labii inferioris, depressor anguli oris and mentalis muscles.
Closing the lips: orbicularis oris muscle.
Compacting the cheek: buccinator muscle.
The bulk of the mouth muscles are joined by a fibromuscular hub where their fibers insert. This structure is called the modiolus, it is founded at the angles of the mouth and it is primarily formed by the buccinator, orbicularis oris, risorius, levator anguli oris, depressor anguli oris and zygomaticus major muscles. The precise position of the modiolus varies, contributing to the variety of smile shapes which are seen in humans.
Facial muscle List:
- Occipitofrontalis
- Orbicularis oculi
- Corrugator supercilii
- Nasalis
- Depressor septi nasi
- Orbicularis oris
- Buccinator
- Depressor anguli oris
- Levator anguli oris
- Risorius
- Zygomaticus major
- Zygomaticus minor
- Levator labii superioris
- Levator labii superioris alaeque nasi
- Depressor labii inferioris
- Mesntalis
- Platysma
Structure and Function:
The facial muscles have 2 major functions for the body: mastication and facial expressions. The muscles of mastication include the temporalis, medial pterygoid, lateral pterygoid, and the masseter (buccinator muscle is an important accessory of chewing). Another important function is facial expression.
Muscles (origin, insertion, nerve supply)
Orbital Facial Muscles: The orbital facial muscles comprise of three main muscles:
Occipitofrontalis (frontalis contributes to this functional group)
Orbicularis oculi
Corrugator supercilii
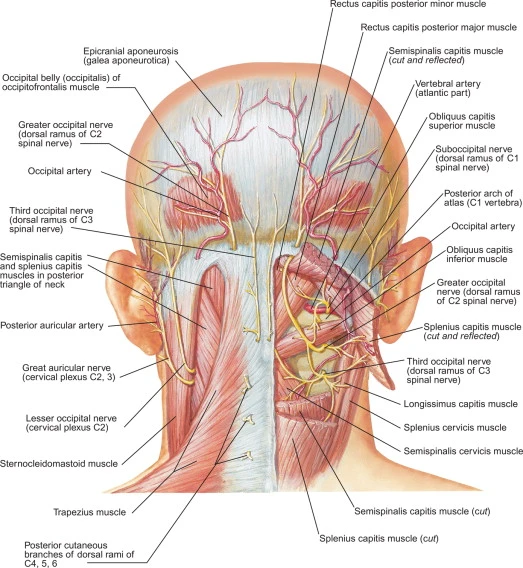
Occipitofrontal muscle:
Occipitofrontalis is one of the muscles of the scalp. It consists of 2 separate bellies:
Origin:
- Occipital part – which originates from occipital bone (lateral part of the upper nuchal line) and from the mastoid aspect of the temporal bone.
- Frontal part – originates from the superior fibres of the other upper facial muscles (ie. orbicularis oculi, corrugator supercilii and procerus
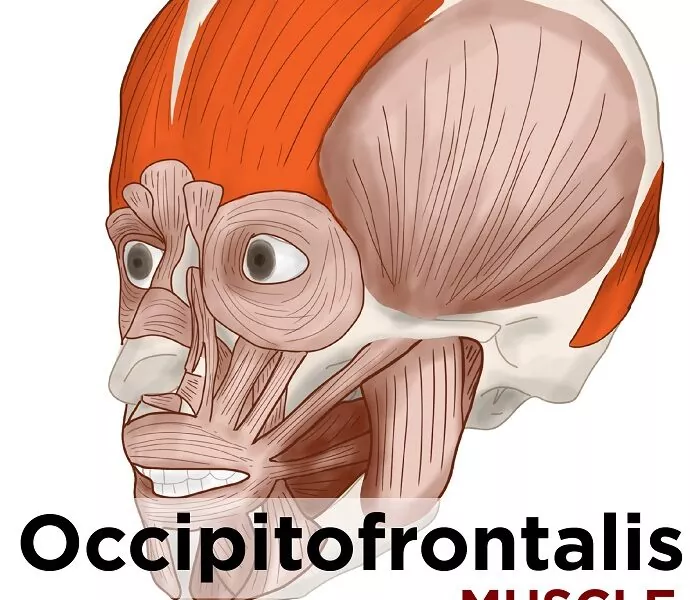
Insertion
The occipital part inserts into the epicranial aponeurosis and the frontal belly inserts into the fascia of the facial muscles surrounding the eyes and the skin above the eyes.
Action
Contraction of this muscle raises the eyebrows and wrinkles the forehead.
The frontalis portion elevates the eyebrows, which causes horizontal wrinkles in the forehead.
It also weakly moves the skin of the scalp anteriorly
The occipital part weakly moves the scalp skin posteriorly.
Nerve supply:
The temporal branch of the facial nerve innervates the frontalis and the posterior auricular branch of the facial nerve innervates the occipitalis.
Blood supply
The occipital belly is supplied by the occipital artery and the frontal belly is supplied by the supraorbital and supratrochlear arteries.
Orbicularis oculi
Origin
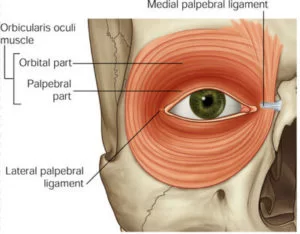
This muscle originates from the nasal portion of the frontal bone, frontal process of the maxilla, the medial palpebral ligament, as well as the lacrimal crest and lacrimal bone
Insertion
The insertion site of this muscle includes the skin overlying the circumference of the orbit, the orbital septum, the temporal aspect of the orbit and inferiorly towards the cheek.
Action
This muscle mainly functions to close the eye. The palpebral section functions voluntarily, as well as involuntarily during such actions as in blinking. The orbital section requires conscious effort.
The lacrimal section controls the tear pump mechanism that filters into the lacrimal sac.
Nerve supply
The temporal and zygomatic branches of the facial nerve.
Blood supply
Branches of the facial, superficial temporal, maxillary and ophthalmic arteries.
Corrugator supercilii
Lying above the orbicularis oculi muscle and below occipitofrontalis, Corrugator Supercilii is a small muscle which is located at the medial end of the eyebrow. The Latin name means “Wrinkler of the Eyebrows”: Corrugator from the Latin verb to wrinkle, corrugo, and the Latin word for eyebrow is supercilium, which in the plural becomes supercilii.
Origin
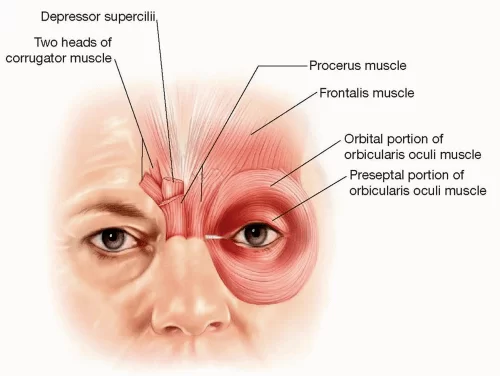
This muscle originates at the medial end of the supraorbital ridge.
Insertion
The skin of the forehead near the eyebrow acts as the insertion site for this muscle.
Action
Contraction of this muscle assists in wrinkling the forehead and drawing the eyebrows downwards and medially to assist in shielding the eyes from bright light.
Nerve supply
The temporal branch of the facial nerve.
Blood supply
The ophthalmic artery and branches from the superficial temporal artery.
Nasalis
This is the largest of the nasal facial muscles that comprises of two main groups. These two groups include the transverse and alar sections.
Origin
The nasalis muscle originates from the incisive fossa of the maxilla.
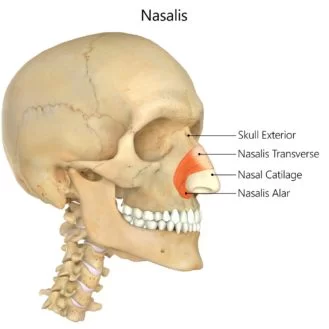
Insertion
Insertion occurs at an aponeurosis over the bridge of the nose (which blends with its counterpart), as well as at the skin around the alar part of the nose.
Action
Compression of the nasal bridge
Depression of the corners of the nostrils
Depression of the tip of the nose
Nerve supply
The buccal branch of the facial nerve.
Blood supply
The superior labial branch of the facial artery.
The infraorbital branch of the maxillary artery
Depressor septi nasi
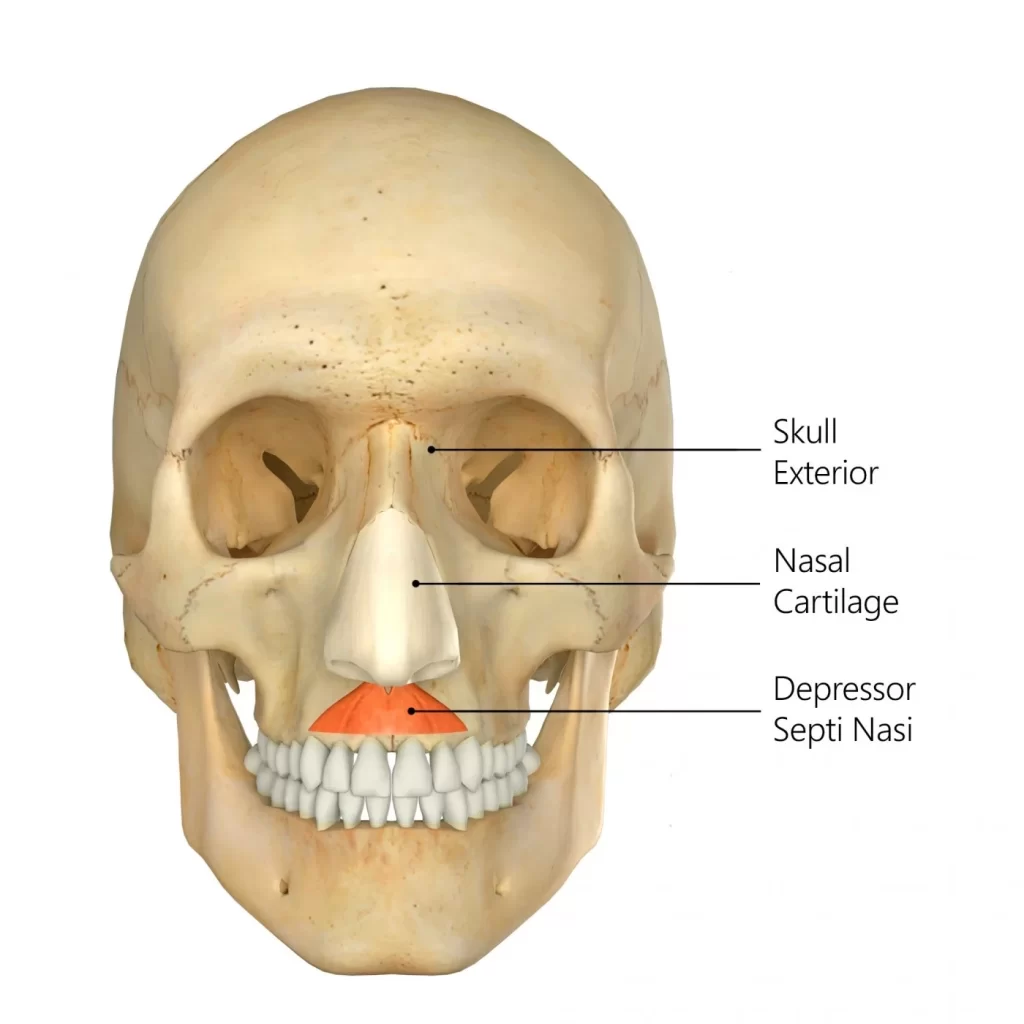
Depressor Septi Nasi, this muscle is sometimes absent or present only in rudimentary form.
Origin
The incisive fossa of the maxilla is the site of the origination of this muscle.
Insertion
The nasalis muscle and nasal septum.
Action
Contraction of this muscle widens the nasal aperture.
Nerve supply
The buccal branch of the facial nerve.
Blood supply
The superior labial branch of the facial artery
Orbicularis oris
This sphincter-like muscle is located around the circumference of the mouth.
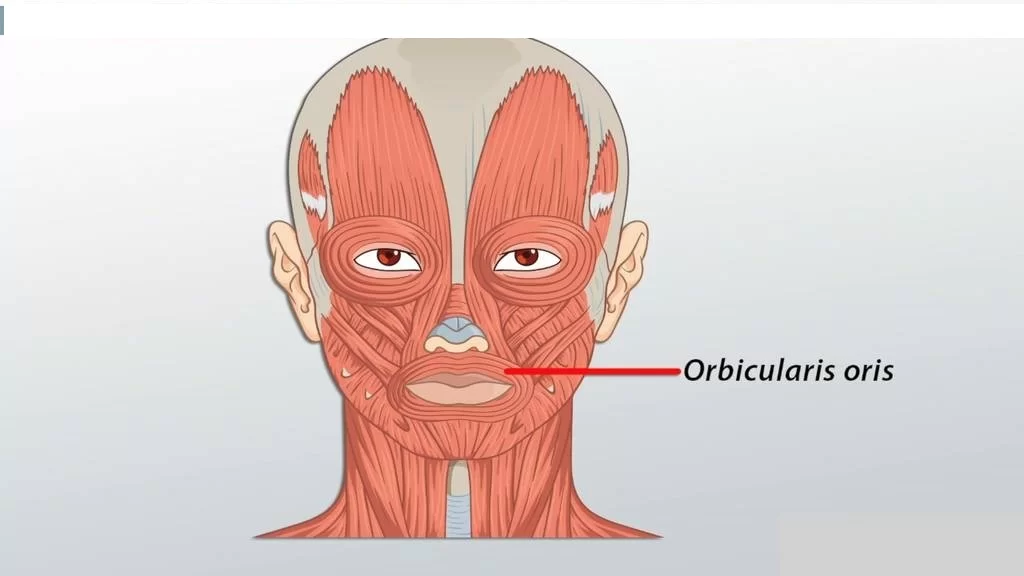
Origin
The medial aspect of the maxilla and mandible and the modiolus.
Insertion
The skin surrounding the lips is the insertion site of the orbicularis oris muscle.
Action
The contraction of this muscle puckers the lips and closes the mouth.
Nerve supply
The buccal branch of the facial nerve.
Blood supply
The superior and inferior labial branches of the facial artery.
Buccinator
The buccinator is located between the maxilla and mandible. The buccinator forms the anterior aspect of the cheek and the lateral aspect of the oral cavity. Several structures penetrate the buccinators, including the parotid duct, molar glands of the cheeks, as well as the buccal branch of the mandibular nerve.
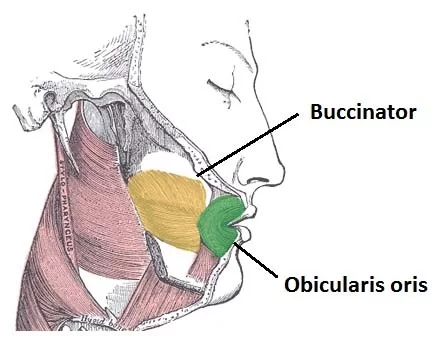
Origin
The outer surfaces of the alveolar processes of the mandible and maxilla, and the pterygomandibular raphe.
Insertion
The orbicularis oris muscle and modiolus act as the insertion site for this muscle.
Action
Contraction of this muscle compresses the cheeks against the teeth (this action is especially useful in mastication and whistling).
Nerve supply
The buccal branch of the facial nerve.
Blood supply
The buccal branch of the maxillary artery.
Depressor anguli oris
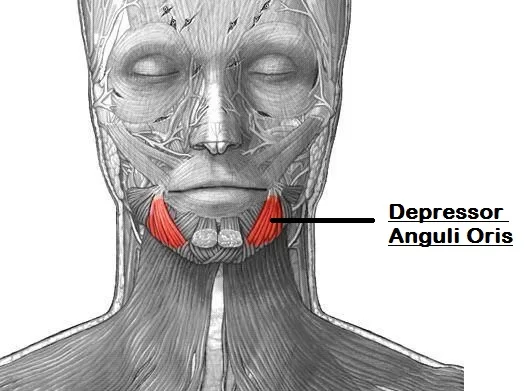
Origin
The mental tubercle of the mandible.
Insertion
The modiolus and angle of the mouth.
Action
Contraction of this muscle causes depression of the angle of the mouth which contributes to frowning.
This muscle is in direct opposition to the actions of the levator angulioris muscle.
Nerve supply
The buccal and mandibular branches of the facial nerve.
Blood supply
The inferior labial branch of the facial artery and mental branch of the maxillary artery.
Levator anguli oris
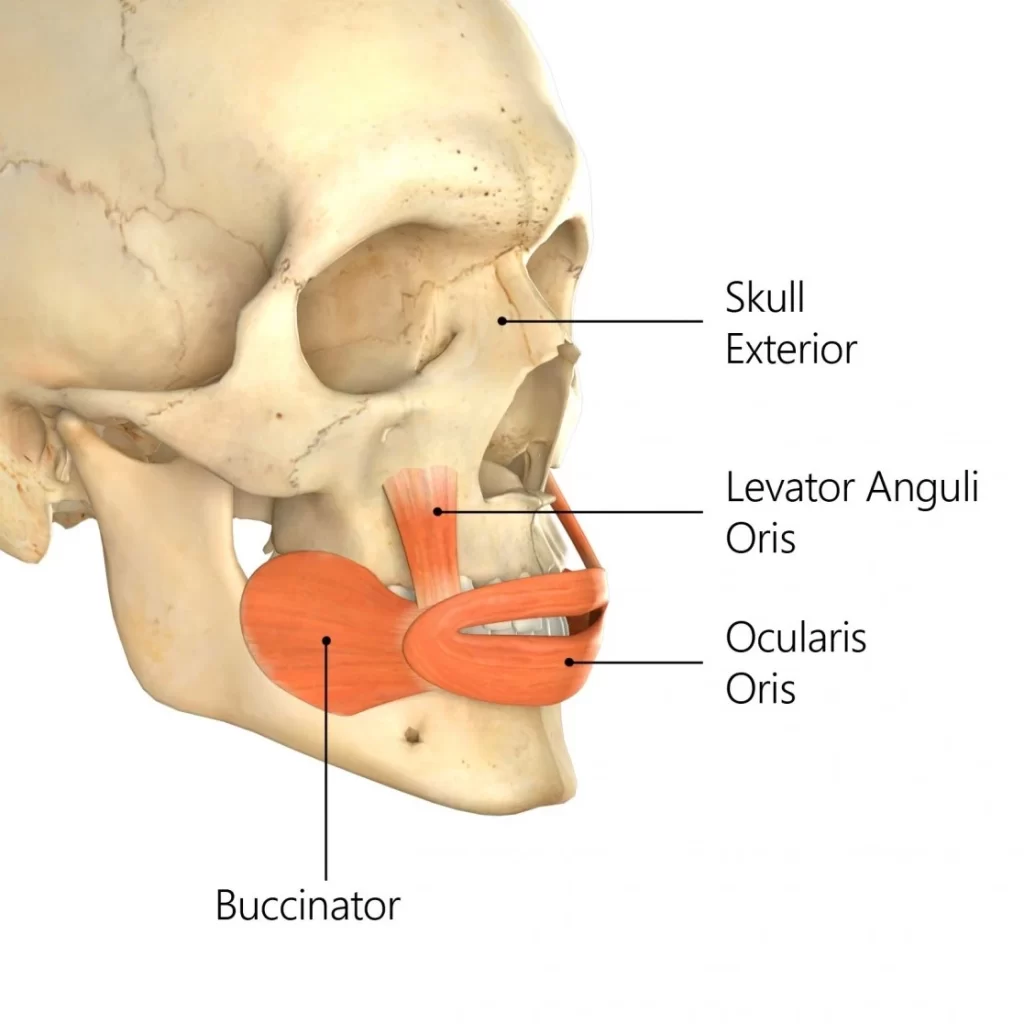
Origin
The canine fossa of the maxilla.
Insertion
The modiolus and angle of the mouth.
Action
Contraction of this muscle elevates the angle of the mouth contributing to smiling.
Nerve supply
The zygomatic and buccal branches of the facial nerve.
Blood supply
The superior labial branch of the facial artery and the infraorbital branch of the maxillary artery.
Risorius
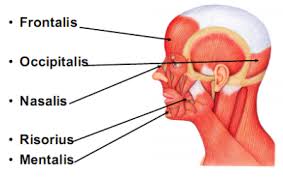
Origin
The parotid fascia.
Insertion
The modiolus of the mouth.
Action
This muscle draws the angle of the mouth backward.
Nerve supply
The buccal branch of the facial nerve.
Blood supply
The superior labial branch of the facial artery.
Zygomaticus major
Origin
The zygomatic bone.
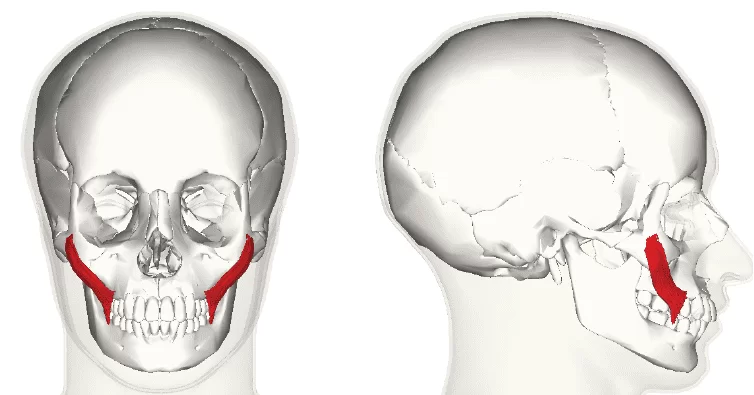
Insertion
The modiolus of the mouth.
Action
This muscle helps to facilitate smiling by pulling the angles of the mouth superiorly and laterally.
Nerve supply
The zygomatic and buccal branches of the facial nerve.
Blood supply
The superior labial branch of the facial artery.
Zygomaticus minor
Origin
The zygomatic bone.
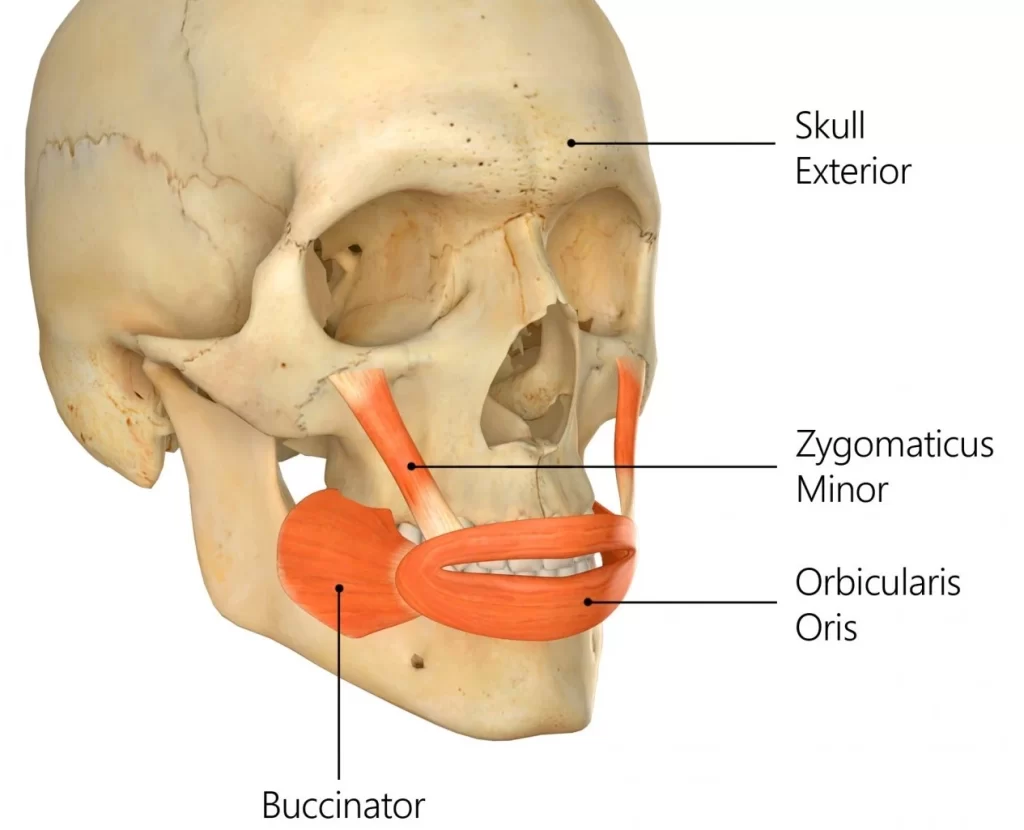
Insertion
This muscle inserts into the skin of the lateral upper lip.
Action
Contraction of this muscle aids in the elevation of the upper lip.
Nerve supply
The zygomatic and buccal branches of the facial nerve.
Blood supply
The superior labial branch of the facial artery.
Levator labii superioris
(also known as the quadratus labii superioris)
Origin
The maxilla and zygomatic bone superior to infraorbital foramen.
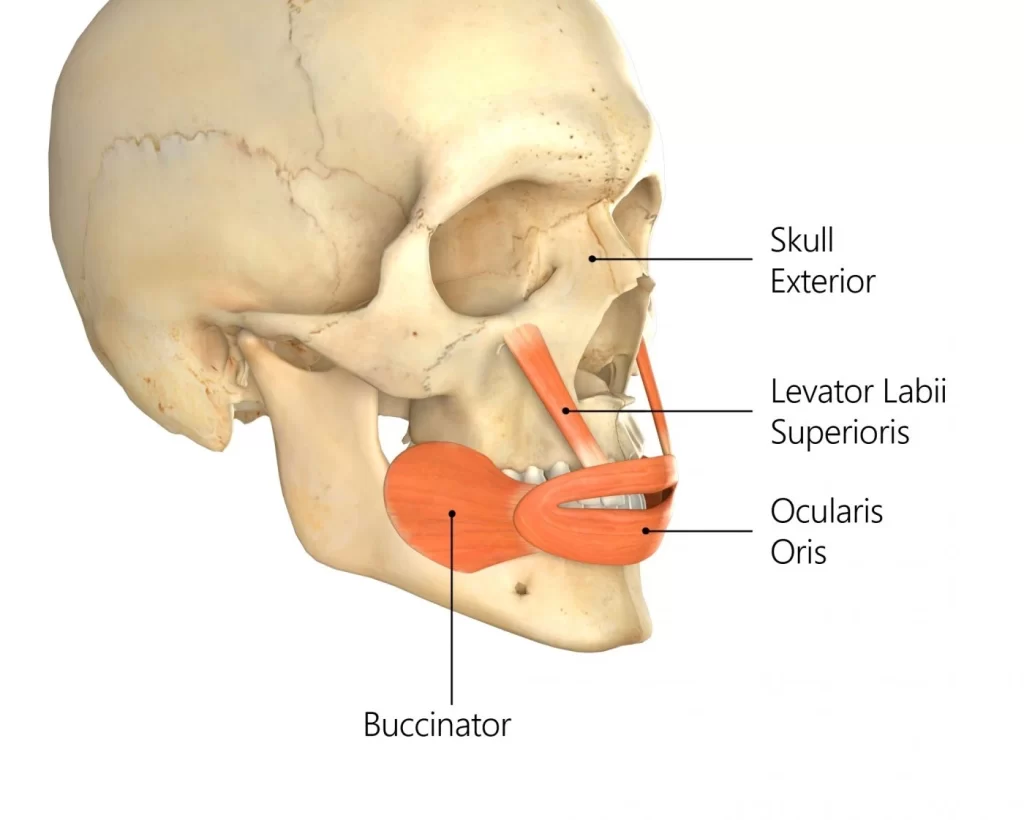
Insertion
This muscle inserts into the skin and muscle of the upper lip.
Action
The contraction causes elevation of the upper lip.
Nerve supply
The zygomatic and buccal branches of the facial nerve.
Blood supply
The facial artery and the infraorbital branch of the maxillary artery.
Levator labii superioris alaeque nasi
Origin
The frontal process of the maxilla.
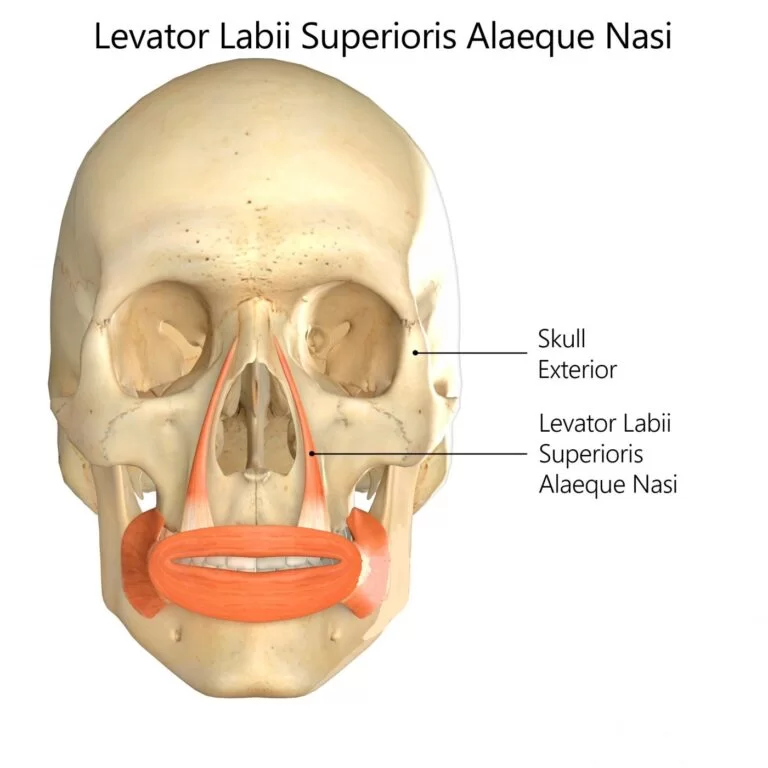
Insertion
Skin of the alar cartilage of nose and skin of the upper lip.
Action
This muscle facilitates the expression of ‘snarling’ by causing dilation of the nostrils, as well as elevation of the wings of the nose and upper lip.
Nerve supply
The zygomatic and buccal branches of the facial nerve.
Blood supply
The facial artery and the infraorbital branch of the maxillary artery.
Depressor labii inferioris
Origin
The mandible (specifically between the mental foramen and the symphysis).
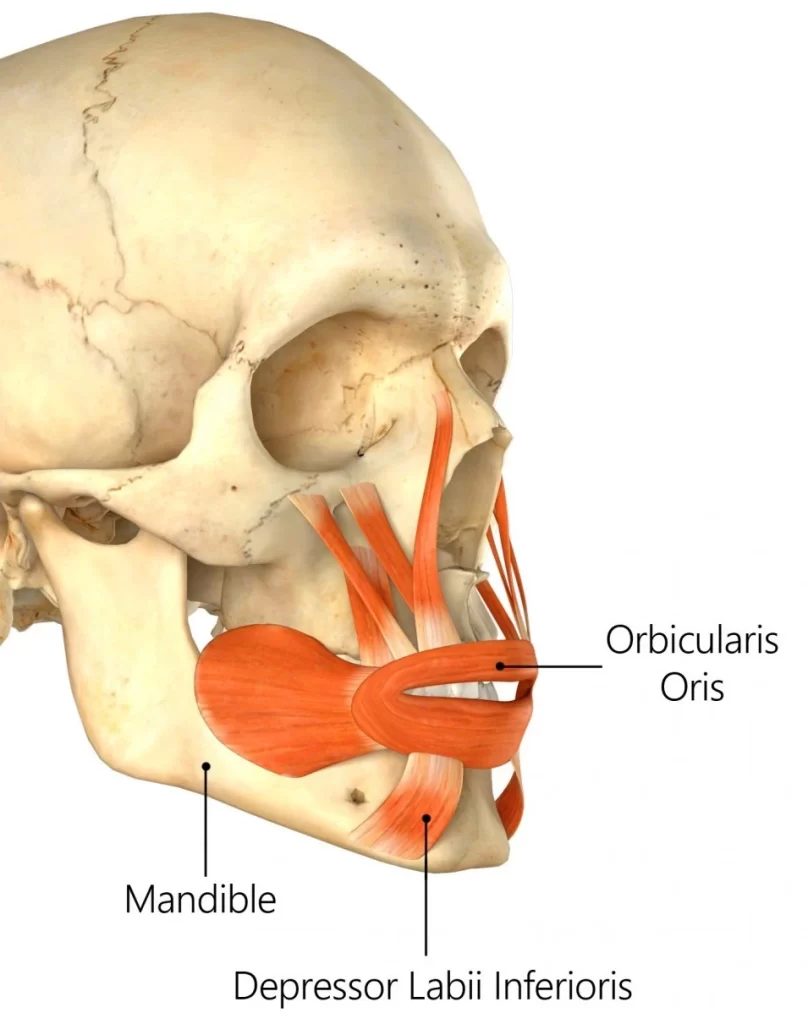
Insertion
The skin of the lower lip. Its fibres blend with the fibres of the orbicularis oris muscle at the insertion point.
Action
Contraction of this muscle depresses the lower lip.
Nerve supply
The mandibular branch of the facial nerve.
Blood supply
The inferior labial branch of the facial artery and the mental branch of the maxillary artery.
Mentalis
Origin
The anterior aspect of the mandible.
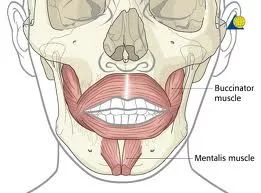
Insertion
The skin of the chin.
Action
Contraction of this muscle causes protrusion of the lower lip, as well as elevation and wrinkling of the skin of the chin.
Nerve supply
The mandibular branch of the facial nerve.
Blood supply
The inferior labial branch of the facial artery and the mental branch of the maxillary artery.
Platysma
Origin
The skin and fascia of the infraclavicular and supraclavicular regions.
Insertion
The base of the mandible, skin of the cheek and lower lip, angle of the mouth, as well as the orbicularis oris muscle.
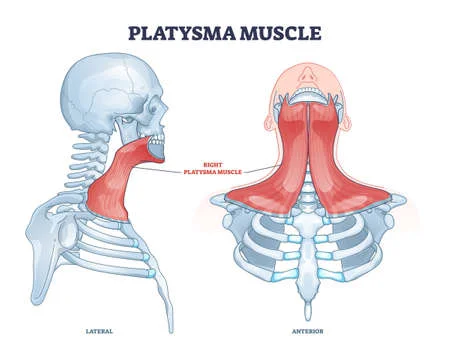
Action
Draws the corners of the mouth downwards which assists in creating the expression of melancholy.
Tenses the skin of the neck when the teeth are clenched.
Depresses the lower jaw.
Nerve supply
The cervical branch of the facial nerve.
Blood supply
Branches of the submental and suprascapular arteries.
Clinical Significance
FACIAL PALSY
Introduction
Facial palsy is due to damage in the facial nerve that supplies the muscles of the face. It can be categorized into two based on the location of casual pathology:
- Central facial palsy- due to damage above the facial nucleus
- Peripheral facial palsy due to damage at or below the facial nucleus.
Clinically Relevant Anatomy
The VIIth cranial Nerve has its nucleus in the Pons and takes a rather winding route before exiting the skull through the stylomastoid foramen. It then passes through the parotid gland, splitting into 5 branches: Temporal, zygomatic, buccal, mandibular, and cervical.
Causes of Peripheral Facial Palsy
There are several causes of Facial Palsy:
- Idiopathic or Bell’s Palsy – Cause not known but likely to be linked to Herpes Simplex infection. This is the most common cause of facial paralysis.
- Tumour – A tumour compressing the facial nerve can result in facial paralysis, but more commonly the facial nerve is damaged during the surgical removal of a tumour. The most common tumour to result in facial palsy during surgical removal is the Acoustic Neuroma (AKA Vestibular Schwannoma). Less commonly, cholesteatoma, hemangioma, Facial Schwannoma or parotid gland tumours (or the surgery to remove them) are the cause.
- Infection
- Ramsay Hunt Syndrome – Caused by Herpes Zoster infection = a syndromic occurrence of facial paralysis, herpetiform vesicular eruptions, and vestibulocochlear dysfunction. Patients presenting with Ramsay Hunt syndrome generally have a greater risk of hearing loss than do patients with Bell palsy, and the course of the disease is more painful. Moreover, a lower recovery rate is observed in these patients.
- Lyme Disease – Infection with Borrelia burgdorferi via tick bites is another cause of facial paralysis. Of patients affected with Lyme disease, 10% develop facial paralysis, with 25% of these patients presenting with bilateral facial palsy.
- Iatrogenic Facial Nerve Damage – Iatrogenic facial nerve injury occurs most commonly in temporomandibular joint replacement, mastoidectomy, and parotidectomy.
- Congenital
- Rare causes – These include:
- Neurosarcoidosis, Otitis media, Multiple Sclerosis, Moebius Syndrome, Melkersson-Rosenthal syndrome, Guillain-Barre Syndrome, Millard-Gubler Syndrome AKA Ventral Pontine Syndrome (Ipsilateral facial palsy with contralateral hemiplegia caused by involvement of the corticospinal tract along with paralysis of lateral rectus on the ipsilateral side due to the involvement of the abducent nerve), Foville Syndrome AKA Inferior Medial Pontine Syndrome (ipsilateral facial palsy, contralateral hemiplegia with ipsilateral conjugate gaze effects), Eight-and-a-half syndrome (facial palsy with Internuclear ophthalmoplegia and horizontal gaze palsy)
- Trauma, especially temporal and mastoid bone fractures.
Risk factors
- Diabetes
- Pregnancy – might be due to hypercoagulability, elevated blood pressure, increased fluid load, virus infection, and suppressed immunity
- Infection of ear
- Upper respiratory tract infection
- Obesity
Clinical Presentation
Paralysis of the muscles supplied by the Facial Nerve presents on the affected side of the face as follows:
Appearance and Range of Movement:
- Inability to close the eye
- Inability to move the lips eg. into a smile, pucker
- At rest, the affected side of the face may “droop” although if the person is in Synkinesis, the affected side of the mouth may sit higher than the other side
- The lower eyelid may drop and turn outward – “ectropion”
Functional Effects:
- Difficulty eating and drinking as lack of lip seal makes it difficult to keep fluids and food in the oral cavity
- Reduced clarity of speech as the “labial consonents” (ie. b, p, m, v, f) all require lip seal
- Dryness of the affected eye – see the Dry Eye page for more details
Somatic Effects:
- The facial nerve supplies the lachrymal glands of the eye, the saliva glands, and to the muscle of the stirrup bone in the middle ear (the stapes). It also transmits taste from the anterior 2/3 of the tongue.
Facial palsy often involves:
- Lack of tear production in the affected eye, causing a dry eye, with a risk of corneal ulceration.
- In Facial Nerve palsy there are 2 problems that contribute to making the eye dry:
- The greater petrosal nerve, derived from the facial nerve, supplies the parasympathetic autonomic component of the lacrimal gland. – controlling the production of moisture/tearing in the eyes.
- The zygomatic branch of the Facial Nerve supplies Orbicularis Oculi, and the resulting paralysis causes inability(or reduced ability) to close the eye or blink, so the tears (or indeed artificial lubrication in the form of drops, gel or ointment) are not spread across the cornea properly.
- Hyperacusis = sensitivity to sudden loud noises
- Altered taste sensation.
Bell’s Phenomenon
Bell’s phenomenon (also known as the palpebral oculogyric reflex) is a medical sign that allows observers to notice an upward and outward movement of the eye, when an attempt is made to close the eyes. The upward movement of the eye is present in the majority of the population, and is a defensive mechanism.
Differential Diagnosis
If the forehead is not affected (ie the patient is able to raise fully the eyebrow on the affected side) then the facial palsy is likely to be a result of a lesion in the Upper Motor Neuron (UMN). Paralysis which includes the forehead, such that the patient is unable to raise the affected eyebrow, is a Lower Motor Neuron (LMN)lesion.
However, caution is advised in using preservation of forehead function to diagnose a central lesion. Patients may have sparing of forehead function with lesions in the pontine facial nerve nucleus, with selective lesions in the temporal bone, or with an injury to the nerve in its distribution in the face. It is worth remembering that a cortical lesion that produces a lower facial palsy/paresis is usually associated with a motor deficit of the tongue and weakness of the thumb, fingers, or hand on the ipsilateral side.
Physiotherapy Management
In the early stages of facial palsy, the most important thing to do is to check that the patient is caring for the affected eye in an appropriate way. As the facial nerve is responsible for the production of lubrication to the cornea, the patient is highly likely to suffer from Dry Eye in the early weeks and months for facial palsy, which puts them at risk of developing a corneal ulcer, which can lead to damage to vision in that eye.
The therapist should educate the patient in the management of a dry Eye if this has not been done by other medical personnel. If the eye is looking red or the patient reports frequent episodes of redness, an urgent referral to ophthalmology (or advise the patient to attend an Eye Hospital Emergency Department) is required. Please see the Dry Eye page for more detailed information, including the presentation of dry eye, risks of corneal ulcer, and management including taping and use of artificial lubrication.
Neuromuscular Retraining (NMR)-
Electromyography (EMG) and mirror biofeedback
Trophic Electrical Stimulation (TES)
Proprioceptive Neuro Muscular Facilitation Techniques
Evidence of Physiotherapy Treatments
According to clinical practice guidelines, physiotherapy is recommended (“weak recommendation”) in Bell’s palsy, and Neuromuscular Retraining techniques are effective in increasing facial range of movement and symmetry, as well as reducing/minimizing synkinesis.
The therapy consists of exercises with mirrors.
The effect of electrical stimulation is controversial.
One study found that the PNF technique is more effective than conventional exercises.


6 Comments