Facial Nerve: Anatomy, Physiology, Function and Clinical Importance
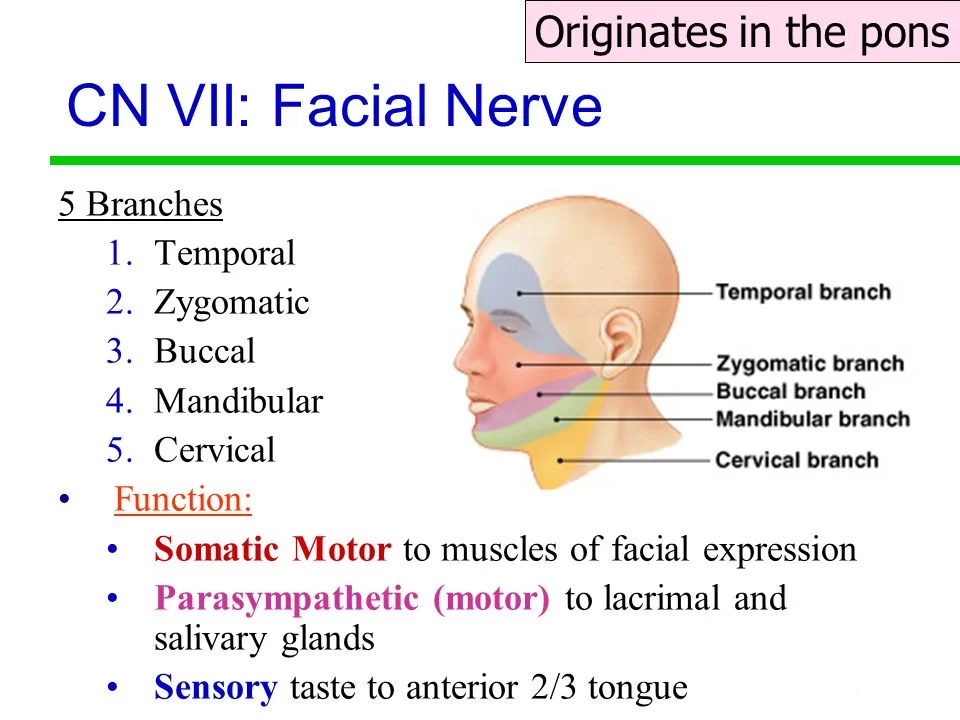
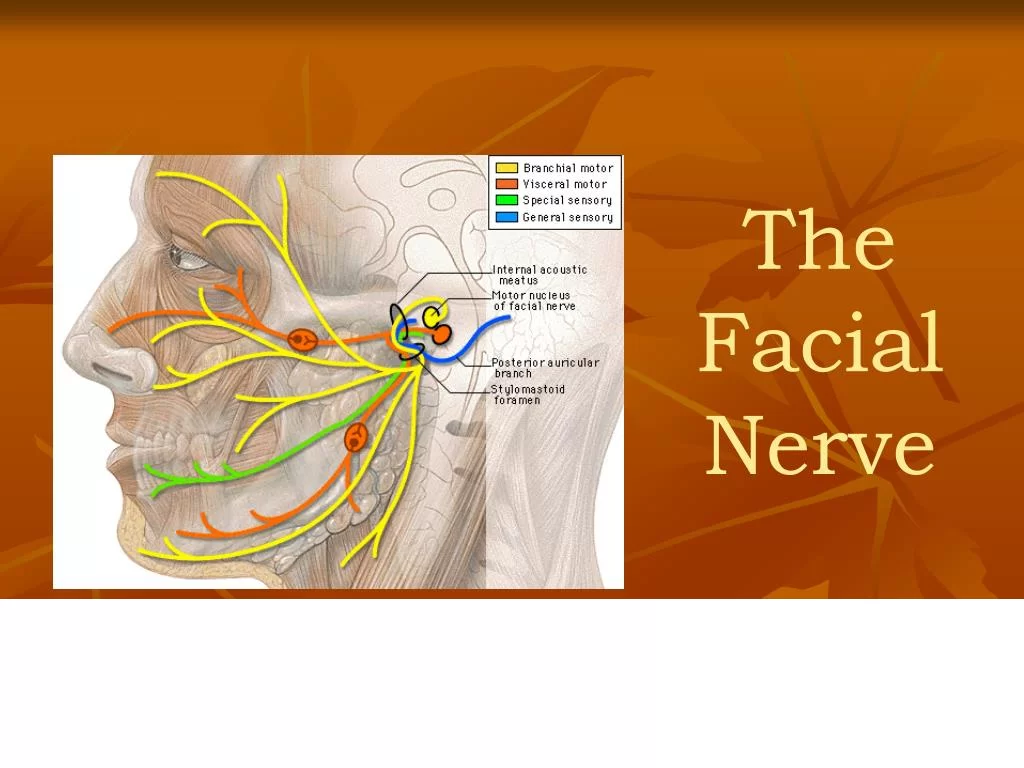
The facial nerve is the seventh cranial nerve, or simply CN VII. It emerges from the pons of the brainstem, controls the muscles of facial expression, and functions in the conveyance of taste sensations from the anterior two-thirds of the tongue.
The nerves typically travel from the pons through the facial canal in the temporal bone and exit the skull at the stylomastoid foramen. It arises from the brainstem from an area posterior to the cranial nerve VI (abducens nerve) and anterior to the cranial nerve VIII (vestibulocochlear nerve).
The facial nerve also supplies preganglionic parasympathetic fibers to several head and neck ganglia.
The facial and intermediate nerves can be collectively referred to as the nervus intermediofacialis.
Anatomical Course
The course of the facial nerve is very complex. There are many branches, which transmit a combination of sensory, motor, and parasympathetic fibres.
Anatomically, the course of the facial nerve can be divided into two parts:
Intracranial – the course of the nerve through the cranial cavity, and the cranium itself.
Extracranial – the course of the nerve outside the cranium, through the face and neck.
Intracranial:
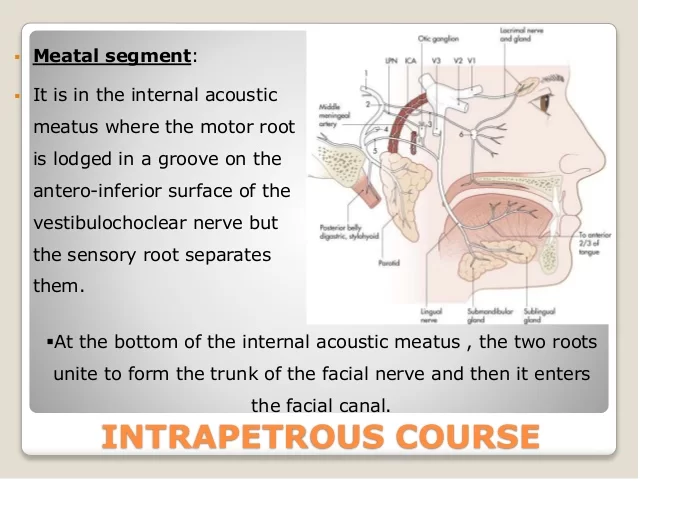
- The nerve arises in the pons, an area of the brainstem. It begins as two roots; a large motor root, and a small sensory root (the part of the facial nerve that arises from the sensory root is sometimes known as the intermediate nerve).
- The two roots travel through the internal acoustic meatus, a 1cm long opening in the petrous part of the temporal bone. Here, they are in very close proximity to the inner ear.
- Still, within the temporal bone, the roots leave the internal acoustic meatus, and enter into the facial canal.
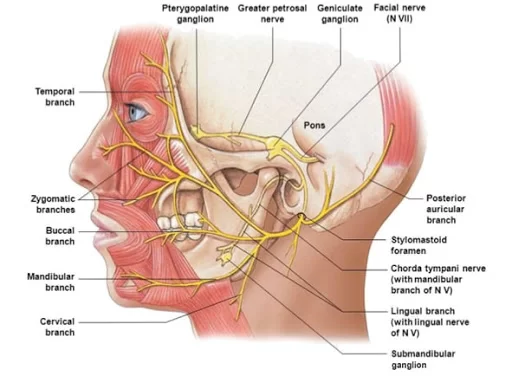
- The canal is a ‘Z’ shaped structure. Within the facial canal, three important events occur:
Firstly the two roots fuse to form the facial nerve.
Next, the nerve forms the geniculate ganglion (a ganglion is a collection of nerve cell bodies).
Lastly, the nerve gives rise to:
- Greater petrosal nerve – parasympathetic fibres to mucous glands and lacrimal glands.
- Nerve to stapedius – motor fibres to stapedius muscle of the middle ear.
- Chorda tympani – special sensory fibres to the anterior 2/3 tongue and parasympathetic fibres to the submandibular and sublingual glands.
- The facial nerve then exits the facial canal (and the cranium) via the stylomastoid foramen. This is an exit located just posterior to the styloid process of the temporal bone.
Extracranial:
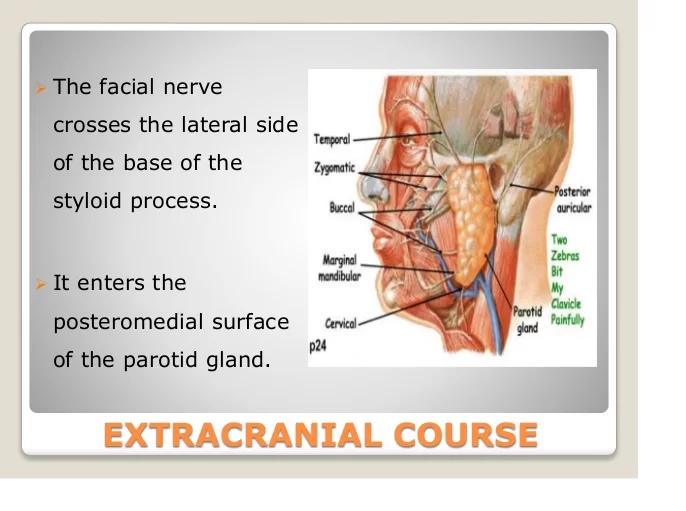
- After exiting the skull, the facial nerve turns superiorly to run just anterior to the outer ear.
- The first extracranial branch to arise is the posterior auricular nerve. It provides motor innervation to some of the muscles around the ear.
- Immediately distal to this, motor branches are sent to the posterior belly of the digastric muscle and to the stylohyoid muscle.
- The main trunk of the nerve, now termed the motor root of the facial nerve, continues anteriorly and inferiorly into the parotid gland (note – the facial nerve does not contribute towards the innervation of the parotid gland, which is innervated by the glossopharyngeal nerve).
Within the parotid gland, the nerve terminates by splitting into five branches:
- Temporal branch
- Zygomatic branch
- Buccal branch
- Marginal mandibular branch
- Cervical branch
These branches are responsible for innervating the muscles of facial expression.
Structure of Facial Nerve:
The path of the facial nerve can be divided into six segments.
- Intracranial (cisternal) segment
- Meatal (canalicular) segment (within the internal auditory canal)
- Labyrinthine segment (internal auditory canal to geniculate ganglion)
- Tympanic segment (from geniculate ganglion to pyramidal eminence)
- Mastoid segment (from pyramidal eminence to stylomastoid foramen)
- Extratemporal segment (from stylomastoid foramen to post parotid branches)
The motor part of the facial nerve arises from the facial nerve nucleus in the pons while the sensory and parasympathetic parts of the facial nerve arise from the intermediate nerve.
From the brain stem, the motor and sensory parts of the facial nerve join together and traverse the posterior cranial fossa before entering the petrous temporal bone via the internal auditory meatus.
Upon exiting the internal auditory meatus, the nerve then runs a tortuous course through the facial canal, which is divided into the labyrinthine, tympanic, and mastoid segments.
The labyrinthine segment is very short and ends where the facial nerve forms a bend known as the geniculum of the facial nerve (“genu” meaning knee), which contains the geniculate ganglion for sensory nerve bodies.
The first branch of the facial nerve, the greater superficial petrosal nerve, arises here from the geniculate ganglion.
The greater petrosal nerve runs through the pterygoid canal and synapses at the pterygopalatine ganglion.
Post synaptic fibers of the greater petrosal nerve innervate the lacrimal gland.
In the tympanic segment, the facial nerve runs through the tympanic cavity, medial to the incus.
The pyramidal eminence is the second bend in the facial nerve, where the nerve runs downward as the mastoid segment.
In the temporal part of the facial canal, the nerve gives rise to the nerve to the stapedius and chorda tympani.
The chorda tympani supplies taste fibers to the anterior two-thirds of the tongue and also synapses with the submandibular ganglion.
Postsynaptic fibers from the submandibular ganglion supply the sublingual and submandibular glands.
Upon emerging from the stylomastoid foramen, the facial nerve gives rise to the posterior auricular branch.
The facial nerve then passes through the parotid gland, which it does not innervate, to form the parotid plexus, which splits into five branches innervating the muscles of facial expression (temporal, zygomatic, buccal, marginal mandibular, cervical).
Nucleus:
- The cell bodies for the facial nerve are grouped in anatomical areas called nuclei or ganglia.
- The cell bodies for the afferent nerves are found in the geniculate ganglion for taste sensation.
- The cell bodies for muscular efferent nerves are found in the facial motor nucleus whereas the cell bodies for the parasympathetic efferent nerves are found in the superior salivatory nucleus.
Development:
- This nerve is developmentally derived from the second pharyngeal arch, or branchial arch.
- The second arch is called the hyoid arch because it contributes to the formation of the lesser horn and upper body of the hyoid bone (the rest of the hyoid is formed by the third arch).
- The facial nerve supplies motor and sensory innervation to the muscles formed by the second pharyngeal arch, including the muscles of facial expression, the posterior belly of the digastric, stylohyoid, and stapedius.
- The motor division of the facial nerve is derived from the basal plate of the embryonic pons, while the sensory division originates from the cranial neural crest.
- Although the anterior two-thirds of the tongue are derived from the first pharyngeal arch, which gives rise to cranial nerve V, not all innervation of the tongue is supplied by CN V.
- The lingual branch of the mandibular division (V3) of CN V supplies non-taste sensation (pressure, heat, texture) from the anterior part of the tongue via general visceral afferent fibers.
- Nerve fibers for taste are supplied by the chorda tympani branch of cranial nerve VII via special visceral afferent fibers.
Function of the Facial Nerve:
Facial expression:
- The main function of the facial nerve is motor control of all of the muscles of facial expression.
- It also innervates the posterior belly of the digastric muscle, the stylohyoid muscle, and the stapedius muscle of the middle ear.
- All of these muscles are striated muscles of branchiomeric origin developing from the 2nd pharyngeal arch.
Facial sensation:
- In addition, the facial nerve receives taste sensations from the anterior two-thirds of the tongue via the chorda tympani.
- The taste sensation is sent to the gustatory portion (superior part) of the solitary nucleus.
- General sensations from the anterior two-thirds of the tongue are supplied by afferent fibers of the third division of the fifth cranial nerve (V-3).
- These sensory (V-3) and taste (VII) fibers travel together as the lingual nerve briefly before the chorda tympani leaves the lingual nerve to enter the tympanic cavity (middle ear) via the petrotympanic fissure.
- It joins the rest of the facial nerve via the canaliculus for chorda tympani.
- This nerve then forms the geniculate ganglion, which contains the cell bodies of the taste fibers of chorda tympani and other taste and sensory pathways.
- From the geniculate ganglion, the taste fibers continue as the intermediate nerve which goes to the upper anterior quadrant of the fundus of the internal acoustic meatus along with the motor root of the facial nerve.
- The intermediate nerve reaches the posterior cranial fossa via the internal acoustic meatus before synapsing into the solitary nucleus.
- This nerve also supplies a small amount of afferent innervation to the oropharynx below the palatine tonsil.
- There is also a small amount of cutaneous sensation carried by the nervus intermedius from the skin in and around the auricle (outer ear).
Motor Functions:
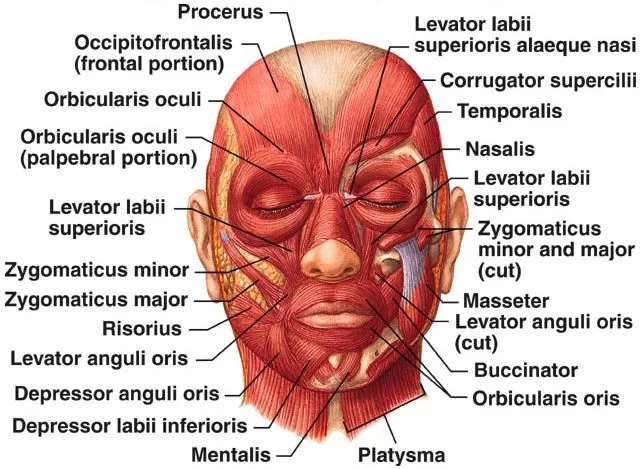
- Branches of the facial nerve are responsible for innervating many of the muscles of the head and neck.
- All these muscles are derivatives of the second pharyngeal arch.
- The first motor branch arises within the facial canal the nerve to stapedius.
- The nerve passes through the pyramidal eminence to supply the stapedius muscle in the middle ear.
- Between the stylomastoid foramen, and the parotid gland, three more motor branches are given off:
- Posterior auricular nerve – Ascends in front of the mastoid process, and innervates the intrinsic and extrinsic muscles of the outer ear. It also supplies the occipital part of the occipitofrontalis muscle.
- Nerve to the posterior belly of the digastric muscle – Innervates the posterior belly of the digastric muscle (a suprahyoid muscle of the neck). It is responsible for raising the hyoid bone.
- Nerve to the stylohyoid muscle – Innervates the stylohyoid muscle (a suprahyoid muscle of the neck). It is responsible for raising the hyoid bone.
- Within the parotid gland, the facial nerve terminates by bifurcating into five motor branches. These innervate the muscles of facial expression:
- Temporal branch – Innervates the frontalis, orbicularis oculi and corrugator supercilii
- Zygomatic branch – Innervates the orbicularis oculi.
- Buccal branch – Innervates the orbicularis oris, buccinator, and zygomaticus muscles.
- Marginal Mandibular branch – Innervates the mentalis muscle.
- Cervical branch – Innervates the platysma.
Special Sensory Functions:
- The chorda tympani branch of the facial nerve is responsible for innervating the anterior 2/3 of the tongue with a special sense of taste.
- The nerve arises in the facial canal, and travels across the bones of the middle ear, exiting via the petrotympanic fissure, and entering the infratemporal fossa. Here, the chorda tympani ‘hitchhikes’ with the lingual nerve.
- The parasympathetic fibres of the chorda tympani stay with the lingual nerve, but the main body of the nerve leaves to innervate the anterior 2/3 of the tongue.
Parasympathetic Functions:
The parasympathetic fibres of the facial nerve are carried by the greater petrosal and chorda tympani branches.
Greater Petrosal Nerve :
- The greater petrosal nerve arises immediately distal to the geniculate ganglion within the facial canal. It then moves in anteromedial direction, exiting the temporal bone into the middle cranial fossa.
- Its travels across (but not through) the foramen lacerum, combining with the deep petrosal nerve to form the nerve of the pterygoid canal.
- The nerve of pterygoid canal then passes through the pterygoid canal (Vidian canal) to enter the pterygopalatine fossa, and synapses with the pterygopalatine ganglion.
- Branches from this ganglion then go on to provide parasympathetic innervation to the mucous glands of the oral cavity, nose and pharynx, and the lacrimal gland.
Chorda Tympani:
- The chorda tympani also carries some parasympathetic fibres. These combine with the lingual nerve (a branch of the trigeminal nerve) in the infratemporal fossa and form the submandibular ganglion.
- Branches from this ganglion travel to the submandibular and sublingual salivary glands.
Clinical Relevance:
Damage to the Facial Nerve:
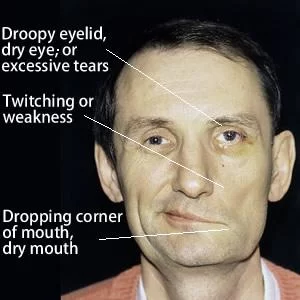
The facial nerve has a wide range of functions. Thus, damage to the nerve can produce a varied set of symptoms, depending on the site of the lesion.
Intracranial Lesions:
- Intracranial lesions occur during the intracranial course of the facial nerve (proximal to the stylomastoid foramen).
- The muscles of facial expressions will be paralyzed or severely weakened.
The other symptoms produced depend on the location of the lesion, and the branches that are affected:
Chorda tympani – reduced salivation and loss of taste on the ipsilateral 2/3 of the tongue.
Nerve to stapedius – ipsilateral hyperacusis (hypersensitive to sound).
Greater petrosal nerve – ipsilateral reduced lacrimal fluid production.
The most common cause of an intracranial lesion of the facial nerve is:
Middle ear pathologies – such as a tumour or infection. If no definitive cause can be found then the disease is termed Bell’s palsy.
Extracranial Lesions:
- Extracranial lesions occur during the extracranial course of the facial nerve (distal to the stylomastoid foramen).
- Only the motor function of the facial nerve is affected, therefore resulting in paralysis or severe weakness of the muscles of facial expression.
There are various causes of extracranial lesions of the facial nerve:
Parotid gland pathology – e.g. a tumour, parotitis, surgery.
Infection of the nerve – particularly by the herpes virus.
Compression during forceps delivery – the neonatal mastoid process is not fully developed and does not provide complete protection of the nerve.
Idiopathic – If no definitive cause can be found then the disease is termed Bell’s palsy.
Facial palsy:
Bell’s palsy:
- It is the idiopathic variety of facial nerve palsy where the patient has signs and symptoms of paralysis of facial muscles without known etiology.
- The etiologies that should be excluded in diagnosing Bell’s palsy include intracranial and extracranial malignancies, infections, trauma, cerebrovascular accident, etc.
- The clinical features that may help to distinguish it from other causes of facial palsy include the sudden onset of usually unilateral facial palsy with the absence of signs and symptoms of CNS, ear, and cerebellopontine angle disease.
- Bell’s palsy is thought to account for approximately 60–75% of cases of acute unilateral facial paralysis with the right side being affected 63% of the time.
- Bell’s palsy typically occurs suddenly, and the symptoms peak in less than 48 hours.
- The paralysis must include the upper and lower aspects of the face, otherwise, if it involves the lower portion of the face, a central cause (supranuclear), such as stroke, should be suspected.
- If the onset of the facial paralysis is insidious, associated with weakness of the contralateral side, or there is a preceding history of trauma or infection, other causes of facial paralysis must be strongly considered.
FAQ
Does facial nerve have sensation?
The muscles of mastication and facial feeling are innervated by the trigeminal nerves (V), whereas the facial nerve (VII) innervates the muscles of facial expression and taste.
What is the buccal branch of the facial nerve?
The buccinator, levator labii, anguli oris, and orbicularis oris are innervated by the buccal branch of the facial nerve. Salivary leaks, fistulae, and sialoceles may result from resection margins that impact the parotid gland, accessory ducts, and Stensen’s duct drainage of saliva.
How do you identify facial nerves?
The location of this muscle—slightly deep to the sternomastoid—as well as the orientation of the muscle fibers that extend toward the mastoid tip make it incredibly simple to recognize. Near its insertion at the mastoid tip, the facial nerve trunk is situated about 1 cm above and parallel to the upper border of the digastric muscle.
What canal is in the facial nerve?
The face nerve travels through the fallopian canal, also known as the facial nerve canal, which is a bony passageway that runs through the petrous temporal bone from the internal auditory meatus to the stylomastoid foramen.

20 Comments