Finger Replacement and Physiotherapy
Introduction
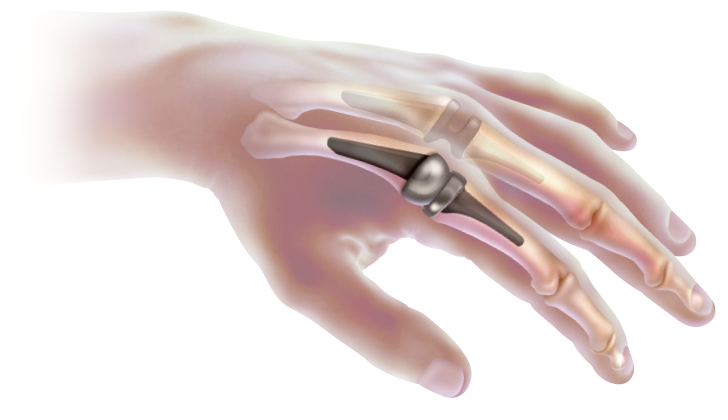
Finger joints are essential for many activities, and arthritis in this area can cause significant joint damage and deformity. Artificial finger joint replacement is a surgical procedure that involves the removal of an arthritic or damaged finger joint and replacement with an artificial prosthesis.
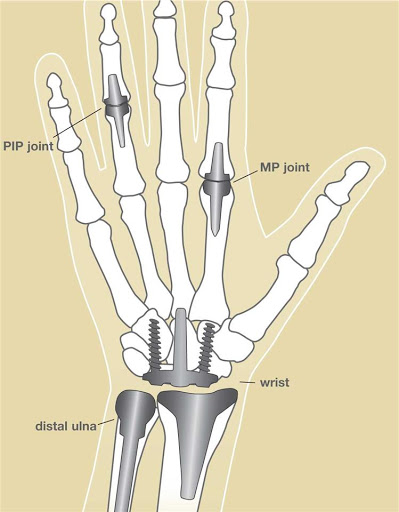
In artificial joint replacement of the finger, a surgeon removes one or more of the joints in your finger and replaces them with an artificial joint. There are two finger joints that can be replaced:
- The PIP joint is the second joint from the end of your finger.
- The MP joint is your knuckle, the joint at the base of your finger.
Joint replacement is used when the joints in your fingers and hands are injured, damaged, or in a lot of pain due to an illness like arthritis. Joint replacement of the finger is most commonly done when your symptoms are severe or don’t get better with medicine or physical therapy.
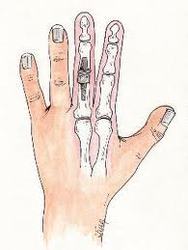
Anatomy
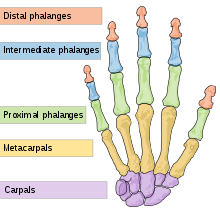
The hands are made up of 27 bones, which are grouped into carpals, metacarpals and phalanges. Each bone is separated by the articular cartilage, which helps in a smooth gliding movement of the fingers. Arthritis develops when the cartilage wears-out, resulting in pain, stiffness and inflammation in the joints. Arthritis can affect any joint in the body, but the most commonly affected joints are the small joints of the fingers.
Causes
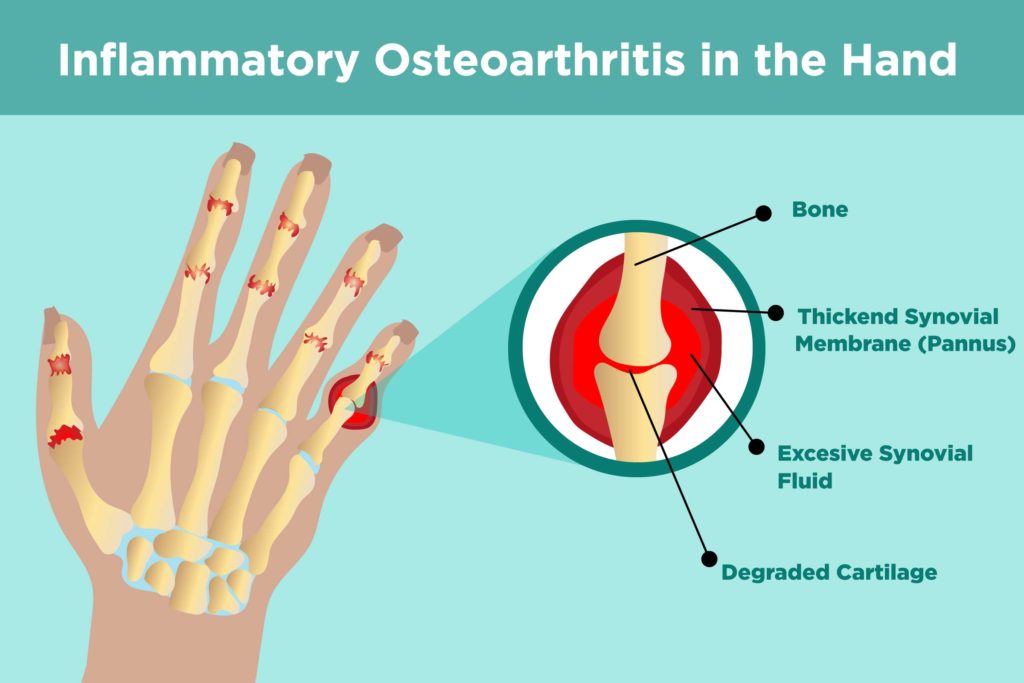
In a normal joint, bones have a smooth surface made of a substance called articular cartilage on their ends that allows one bone to glide easily against another. Joints are lubricated by a thin layer of fluid (synovial fluid) that acts like oil in an engine to keep parts gliding smoothly. When the articular cartilage wears out, is damaged, or the joint fluid is abnormal, problems develop, and joints often become stiff and painful. This is arthritis, which may be possible to treat with a knukcle, wrist or finger joint replacement.
Diagnosis
Your doctor diagnoses arthritis of the finger joint after reviewing your medical history, performing a physical examination, and obtaining X-rays. Additionally, blood tests may also be ordered to confirm the presence of rheumatoid arthritis.
Indications
Artificial finger joint replacement is indicated for patients with arthritis of the fingers. Finger joint replacement is considered if other treatment options fail to relieve the pain and disability.
The surgery is usually reserved for older patients who do not perform heavy labor activities. Finger replacement implants are not appropriate for younger, more active patients as the implants may loosen or wear out over time.
Artificial joints in the hand may help:
- Reduce joint pain
- Restore or maintain joint motion
- Improve the look and alignment of the joint(s)
- Improve overall hand function
Contraindications
Artificial finger joint replacement is not recommended in patients with:
- Poor skin or bone quality
- An active infection in the affected joint
- Damage of muscle or tendons
- Presence of other implants from prior surgeries that would block the insertion or movement of the new prosthetic.
The different surgical options
Surgical options include:
- cleaning of the abnormal cartilage and bone, including removal of bone spurs,
- fusion of the joint and
- joint replacement surgery.
The optimal surgical treatment of arthritis of the hand and wrist varies from patient to patient and is based on many factors. These factors include the patient’s age, hand dominance, employment, level of pain, functional goals, and underlying disease.
Alternatives
Some alternate procedures for treating arthritis include:
- Joint injections
- Oral medications such as aspirin or anti-inflammatory medicine
- Hand therapy exercises and protective splints
- Arthrodesis surgery to fuse bones together, which relieves pain by eliminating motion be-tween damaged joint surfaces
- Resection arthroplasty, which is a surgery to remove arthritic surfaces and/or bone
- Surgery on tendons or ligaments to repair related joint injuries
Procedure
The surgery is performed under local or general anesthesia and usually takes about two hours to complete. A cut on the back of the finger joint is made and the soft tissues are spread out to expose the joint. The bone ends that form the finger joint are cut to form a flat surface. Next, a small cutting tool called a burr is used to create an opening in the bones of the finger joint. Your surgeon will then shape and insert the prosthesis so that it fits snugly in both ends of the finger bone. Nearby ligaments are repositioned to wrap the joint for additional support and the soft tissues are stitched back. The finger is secured in a splint and bandaged.
Finger Joint Replacement Surgery
Finger joint replacement surgery is performed by first removing the damaged and deformed joint surface. Once the damaged portion of the joint is removed, the bone ends are shaped to accommodate the artificial implant. Finger implants may be made of metal, ceramic, or plastic. The implants are positioned and held tightly in the hollow center of the bone. Care is taken to protect the tendons and ligaments that surround the joint.
After surgery, you will work with a hand therapist to regain mobility and strength of the joint. Total recovery after finger joint replacement can take several months. Risks of finger joint replacement include infection, nerve injury, joint instability, and implant problems including wearing out and loosening.As stated before, generally finger joint replacements are best suited for individuals who do not stress the fingers with heavy lifting or repetitive tasks. There are other surgical procedures that are better suited to holding up to these types of activities.
Alternatives to Finger Joint Replacement
There are other surgical options to consider if finger joint replacement is not the right option for you. Probably the most common alternative is called joint fusion. Joint fusion is a surgical procedure to permanently remove the joint, and stimulate the bone to grow where the joint once was. Often the joint is held in proper position with plates, screws, pins, or wires until the bone is fully healed. The advantage of a fusion procedure is that once healed, this is a permanent solution — there are no implants to wear out or loosen over time. The disadvantage is that finger mobility is limited, although with many finger joints this only minimally impacts the function of the finger.
The surgical options vary with the different joints of the hands and wrists
Hand joint replacement surgery options differ according to the specific joint(s) involved.
- DIP joint (joint closest to the fingertip): This joint is not a good candidate for joint replacement. The bones are very small and do not hold the implant very well. The best treatment option for advanced arthritis at this joint is fusion. Hand function is only minimally compromised by lack of motion at this joint after a fusion procedure, while pain is relieved.
- PIP joint (second joint from the fingertip): Joint replacement is commonly performed in the PIP joint. Hand function, especially power grasp, can be hindered by fusion of this joint. The small and ring fingers are the best candidates for joint replacement as they are the most important for power grasp. The index finger is not a good candidate for a PIP joint replacement, as it must withstand sideways forces which accompany movements such as key turning and fine manipulation of objects. These forces cause excess stress on the joint implant and can lead to early implant breakage.
There have been numerous false (prosthetic) joints designed for PIP joint replacement, but only one has stood the test of time. The only non experimental PIP joint replacement is the silicone inter positional arthroplasty. These joints are made of silicone rubber and have a flexible hinge in the middle and stems at the ends which insert into the shaft of the bone, providing stability. The most frequently used silicone joint implants are termed the Swanson implant and the Sutter implant.
The best results with PIP joint replacement are in patients with rheumatoid arthritis and in older, lower-activity patients.
- MCP joint (third joint from the fingertip): Osteoarthritis rarely affects the MCP joints. The most common need for joint replacement in this joint is destruction from rheumatoid arthritis. Silicone joint replacement of the MCP joint has been used since the 1960s and has produced excellent long-term results.
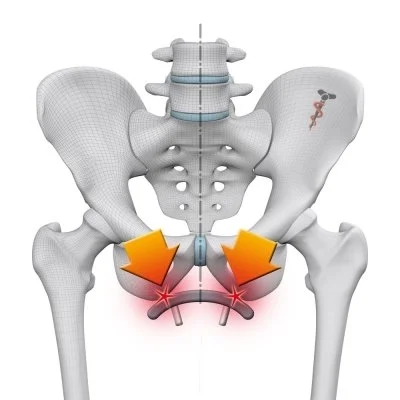
- Thumb basal joint (where the thumb meets the wrist): This joint is exposed to very high stresses with normal activities. Forces felt at the tip of the thumb are multiplied 12 times in their effect to the thumb base, thus predisposing this joint to wear. Arthritis of this joint is very common, especially in women, and frequently requires joint replacement. Attempts at silicone replacement of this joint have not been as successful as hoped due to implant failure and bone destruction. Thus, the most common joint replacement procedure for the thumb base is done with natural material. The procedure is termed the ligament reconstruction-tendon interposition procedure (LRTI). This procedure uses the patient’s own tendon to stabilize the thumb and resurface the joint. LRTI provides stability and pain relief. Long-term results have been excellent. This has also been called the tendon roll or “anchovy” procedure because the tendon used is curled to form the new joint cushion.
- Wrist joint: Most patients with wrist arthritis are best treated with surgical joint cleaning or fusion and not joint replacement. Most wrist-joint prostheses on the market are currently investigational and for use in extremely low activity patients with osteoarthritis or rheumatoid arthritis.
Postoperative care
Following the surgery, the finger is splinted and bandaged. The splint will help keep the finger straight during the healing process. In some cases, your hand may be placed in an arm-length cast for about three weeks. Avoid excessive use of your operated hand as it can damage the new joint(s). You will have to visit your surgeon five to seven days after the surgery. You will be prescribed medication to control the pain and discomfort. You will have to keep your arm propped up to avoid throbbing and swelling. Physical therapy will also be advised to regain mobility and strength of the finger joint.
What are follow-up requirements and options?
After surgery, your doctor may recommend other treatments, including:
- Physical therapy. Physical therapy is a set of exercises, stretches, and other techniques to help you build strength and restore motion to your fingers, knuckles, and hand.
- Splinting. A splint is a tough, or stiff brace that holds your hand in the right position and protects it while it heals.
Risks and Complications
As with any major surgery there are potential risks involved. Some of the risks and complications following artificial finger joint replacement include:
- infection,
- damage to the blood vessels or nerves,
- loosening of the implants,
- wear of the implant, and
- failure of the procedure to relieve pain.
- Dislocation of the artificial joint
You should call the doctor if your finger becomes red, hot, painful or crooked, or you have sudden severe pain or swelling.
Rehabilitation
Physiotherapy will begin once your surgeon allows it. The time frame regarding when you can move your finger after surgery will depend on several factors including your surgeon’s opinion, the type of replacement used, and potentially other factors that are specific to your injury or recovery. Many patients will be able to start doing general finger range of motion exercises a few days after surgery whereas others will be asked to wait 2-3 weeks before beginning any motion to allow further healing time. Generally, once therapy begins, you will be fitted with a removable supportive finger splint that can be taken off to do your exercises but should be worn at all other times including at night.
As your rehabilitation progresses your surgeon or physiotherapist will determine when it is no longer necessary to wear this splint. Generally it is removed during daytime activities before it is removed completely at night. It may even be needed for up to 3 months post surgically.
Your first physiotherapy sessions will focus on relieving the pain associated with the surgical process as well as the immobilization. Modalities are used such as heat, ice, or electrical current to assist with decreasing any pain or swelling you have around the surgical site or anywhere along the arm, or into the shoulder or hand. Massage to these areas may also be done in order to improve circulation and assist with the pain. Depending on how extensive the splint was some of the muscles of the neck may also initially be painful and therefore may also benefit from some massage treatment to make movement of your entire surgical side easier.
The next part of our treatment will focus on regaining the range of motion, strength, and dexterity in your finger, wrist, hand, elbow, and even shoulder. Your physiotherapist will prescribe a series of range of motion and strengthening exercises that you will practice in the clinic and also learn to do as part of your home exercise program. These exercises may include the use of rehabilitation equipment such as mini pulleys, putty, elastics or balls for strengthening and gripping resistance. In addition to strengthening your grip we will educate you on ways to grip and support items in order to do your tasks without putting too much stress on your new finger joint.
If necessary, your physiotherapist will mobilize your finger joint or any other joint in the area that is stiff and impeding normal movement of your hand and limb. This hands-on technique encourages the stiff joints to move gradually into their normal range of motion.
Being able to move your hand and finger so that you can complete your work tasks and daily activities is the goal. Maximizing dexterity can greatly improve the functional use of your hand. For this reason, we will also incorporate activities like picking up items from a table or twisting items into place using your surgical hand. These functional activities encourage the joints and the muscles of the hand and arm to work in unison, which is critical to maximizing the use of your entire upper limb. Exercises where weight is put through your new joint, such as pressing the pad of your finger into something, will also be added, when appropriate, to encourage the joint to tolerate weight in a controlled fashion.
Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program. Generally, the majority of your gains from physiotherapy will occur within the first 2-3 months after the joint is replaced, but ongoing tissue remodeling will occur even up to 12 months post-surgery.
Physiotherapy after Hand Joint Replacement Surgery
Rehab will focus not only on restoration of movement and strength but on activities needed to return to active work, hobbies and sports. Treatment will begin following your surgery and recovery can be seen within 12 weeks.
Weeks 1-3
Initial treatment is focussed on minimising pain and swelling following surgery and to encourage the use of your finger in normal movement patterns. Through early encouragement, end stage rehabilitation becomes easier and the restoration of a fully functioning hand is more complete. Treatment will include:
- Cryotherapy (Ice)
- Analgesia (Pain killers)
- Passive controlled range of movement exercises
- Gentle active finger range of movement exercises
- Wrist range of movement exercises
- Wound monitoring
- Splint use – these can be fixed at varying lengths as to give a constant stretch on the tendon in order to improve range of movement and reduce stiffness.
- Electrotherapy modalities
- Advice
Weeks 4-6
After 3 weeks of rehabilitation your splint can be removed and your rehabilitation can be advanced. During this stage focus will be on the restoration of movement and building up of strength in order to help restore hand function. Treatment will comprise of:
- Splint removal
- Continued passive range of movement to reach end range.
- Active range of movement exercises
- Scar management
- Heat therapy
- Soft tissue massage to break down scar tissue
- Begin gentle strengthening exercises
Weeks 7-12
During the later stages of rehab you will begin to see marked improvements of movement, strength and function of your hand. Physiotherapy will help to maximise your hands mobility and restore functional use. Treatment will consist of:
- Continued active and passive range of movement exercises to end of range
- Progressive strengthening exercises
- Isolated strengthening of replaced joint.
- Hand dexterity
- Functional activity exercises
- Advice for long term care
Following 12 weeks of rehabilitation, you will have achieved significant improvements in range of movement and strength. Physiotherapist will provide you with the knowledge and exercises needed to maximising the success of your surgery, enabling you to achieve maximal function and use of your hand.
5 Hand Exercises for Dexterity and Flexibility
Grab a squeeze ball
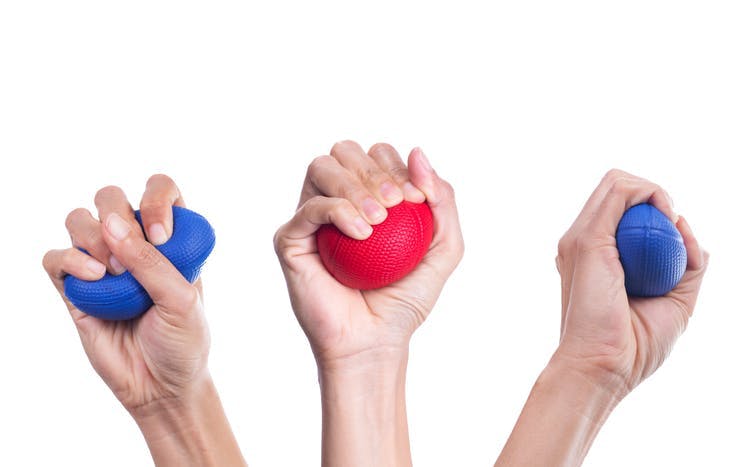
Grab a soft ball and hold it in your palm, squeezing it as hard as you can without causing your hands pain. Hold this position for three to five seconds, and then release. Work up to repeating this exercise 10 to 12 times for each of your hands. Continue this exercise two to three times weekly, but rest approximately two days before your next session. This exercise will provide the ability to hold things without dropping them, as well as help you open door knobs throughout your day.
Put up your dukes and make a fist
With each hand, independently make a gentle fist, then wrap your thumb across your fingers. Hold this position for up to one minute, then release and spread open all of your fingers as wide as you can. Repeat this exercise three to fives times with each hand. This can help you increase your range of motion.
Get relief when you exercise
Warming up your hands before you exercise can help alleviate discomfort, which will subsequently have the potential to make your stretching and movement become easier. Suggested treatments include, soaking them in warm water, wrapping them in a heated towel or using a heating pad for approximately five to 10 minutes. To gain an even deeper warming effect for your hands, you can rub some oil into your hands, put on a pair of rubber gloves and soak them in warm water, or use a heated towel or heating pad. This method may help your hands feel better, especially if you regularly experience pain or stiffness in your hands and fingers.
Lift your fingers
Starting with your left hand, place it flat, palm down, on a table. Starting with your thumb, gently lift each finger at a time slowly off the table. Hold each of your fingers one to two seconds, and then lower them. Repeat with your right hand and then repeat eight to 10 times for each hand. This exercise can help increase the range of motion of your hands, as well as finger flexibility.
Stretch your wrists
Many people, particularly women, have wrist pain during exercise, especially yoga and lifting heavy objects. Sometimes, they even feel this when lifting their children. A stretching exercise for the wrist may help increase flexibility and decrease discomfort. To complete this exercise, extend your right arm in front of you with your palm facing toward the floor. Bend your wrist, pointing the tips of your fingers toward the floor. With your left hand, gently bend your wrist toward you until you feel a mild to moderate stretch in your forearm (that means behind your wrist). Hold this position for at least 15 to 30 seconds, switch to your left arm and then repeat two to four times.




cool!