Geriatrics Disease
What are Geriatric Diseases?
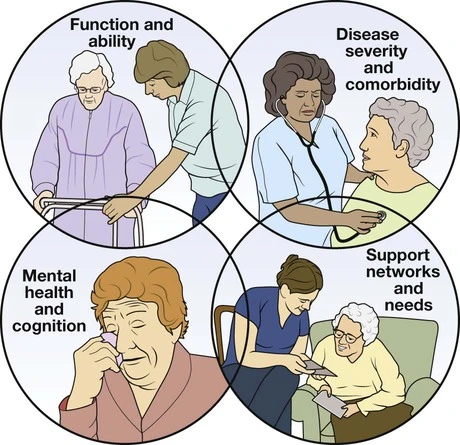
Geriatric diseases are complex diseases, with shared risk factors that include age, cognitive impairment, functional impairment, and reduced mobility. These risk elements have been identified across various common geriatric conditions such as pressure ulcers, incontinence, falls, functional decline, and fever. The management of older adults often differs from that of younger individuals due to factors such as polypharmacy, incomplete symptom representation, and challenges in assigning diagnoses when multiple health conditions coexist.
Elderly adults are more prone to developing age-related illnesses that are less common in younger individuals. While hypertension can be a generational issue, conditions such as cardiovascular disease, ischemic heart disease, urinary incontinence, vascular dementia, multiple sclerosis (MS), and other illnesses are more frequently observed among older adults.
What is Geriatrics?
Geriatrics is focused on understanding the various processes that bring an individual closer to the end of life.
Aging involves a series of changes that make an individual more vulnerable to death. The term ‘old age’ generally refers to individuals who have reached or exceeded the average lifespan. In many societies, retirement, typically occurring around the age of 60-65 years, marks the transition into old age.
There was a time when a silver strand of hair was considered the first sign of aging. However, in the current era of stress and illnesses, premature graying has become commonplace. Nevertheless, classic signs such as graying hair, loss of hair, decreased eyesight and hearing, diminished dexterity, and memory decline are some of the indicators along the path of aging.
Why do people grow old?
Aging has been a fascinating and awe-inspiring aspect of life for ages. Throughout human history, much time has been dedicated to considering the possible causes of old age.
The role of genetic factors in aging has been much studied and recognized through the discovery of longevity genes and the investigation of the early onset of age-related diseases.
Aging occurs at various levels, including DNA, cells, and body tissues. When cells are unable to repair DNA damage, they undergo self-destruction through a process called apoptosis. Apoptosis plays a crucial role in preventing diseases like cancer, but it also contributes to organ degeneration and decline. Aging is also associated with the progressive impairment of genes involved in the regulation and repair of cells and body tissues.
Replicative senescence is another phenomenon often associated with the process of aging. After approximately 50 divisions, cells reach a point where they can no longer divide.
Environmental factors also play a significant role in accelerating the aging process. When oxygen levels exceed 50%, which is necessary for life, cells can become cytotoxic.
Our modern lifestyle choices contribute to the existing factors and can exacerbate the process of aging.
What is The Development of Formal Criteria for Geriatric Disease?
Geriatric diseases refer to multifactorial health conditions that arise when a combination of impairments in various systems leaves an older individual vulnerable to situational challenges. Therefore, the term “syndrome” in geriatrics emphasizes the significant factors contributing to a particular presentation. By using this term, the understanding of geriatric disease aligns well with the concept of phenotype, which refers to the observable characteristics of an individual at the physical, morphological, or biochemical level, influenced by both genetic factors (genotype) and the environment. This concept highlights the significant contributors to visual characteristics, such as phenotype.
Geriatric diseases present certain clinical considerations. Firstly, for a given geriatric disease, multiple risk factors and organ systems are typically involved. Secondly, diagnostic methods to identify the underlying causes can sometimes be impractical, demanding, intimidating, and costly. Lastly, therapeutic management of the clinical manifestations can be beneficial even in the absence of a definitive diagnosis or clarification of the underlying causes.
Instead of the term “geriatric disease,” alternative terms that may be used are “final typical outcome” or “end result.” In this context, geriatric disease refers to the culmination of a series of processes or changes involving multiple contributing factors. This concept is similar to other medical conditions such as renal failure and hypertension, where multiple factors can contribute, making it challenging to always identify the underlying cause, and where management does not solely depend on the underlying reason.
In the field of medical research and practice, the establishment of standardized criteria for disease identification has a long-standing tradition. Examples include criteria used in rheumatology to define rheumatoid arthritis and systemic lupus erythematosus, the National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) clinical criteria for Alzheimer’s disease, and psychiatric diagnoses in the Diagnostic and Statistical Manual of Mental Disorders (DSM). The advantages of such criteria include improved communication in both clinical and research settings, enhanced ability to compare syndromes across studies and pool research findings, and the ability to develop regulations and diagnoses for the International Classification of Diseases.
Implementing standardized criteria would also aid in developing appropriate concepts, promoting pathophysiological research, and enhancing investigations into common mediators. For conditions such as agitation and chronic fatigue syndrome, functional explanations have been formulated, stimulating research in these areas. However, the early establishment of formal criteria without sufficient evidence base can lead to rigid perceptions, hinder progress and advancement in the field, and result in improper application of concepts by physicians and researchers, potentially leading to incorrect diagnoses and mismanagement of treatment. Examples of this phenomenon include the early classification of diabetes as Type 1 and Type 2, or the categorization of hyperlipidemias as Types I to V, which hampered exploration and advancement for many years.
A balanced approach would involve the development of initial criteria for desired geriatric diseases based on an evidence base, using panels comprised of experts from reputable organizations such as the American Geriatrics Society (AGS). These preliminary criteria can then be subjected to analysis by other organizations and the AGS membership. Once released, these criteria can be regularly updated and allowed to evolve. For research studies, these criteria would be valuable in aligning study designs and outcomes, pooling research findings, modifying, expanding, or focusing research models, and appropriately targeting interventions.
What are the Risk Factors for Geriatric Diseases?
An important characteristic of geriatric disease is that it is influenced by significant risk factors. Previous research has indicated that certain geriatric diseases may share common risk factors. To address this, we propose a comprehensive conceptual model for the geriatric disease, which suggests that these shared risk factors can contribute to the development of both specific diseases and the overarching geriatric condition of frailty. Defining frailty as a deficiency in flexibility, balance, muscle strength, cognition, nutrition, endurance, and physical activity, this model highlights how frailty and other geriatric diseases can create a feedback loop, leading to the accumulation of additional risk factors and the development of more geriatric diseases. These pathways ultimately result in disability, dependence, and even death. This conceptual framework provides a unified perspective and is of significant importance in advancing our understanding of both the underlying pathophysiological mechanisms and the management approaches for geriatric diseases.
Diseases and Old Age

Old age, simply put, is a natural process that limits our regular functions and makes us more vulnerable to illness and death.
As we age, there are various changes that occur in our body’s structure and functions. These include a decrease in muscle mass and bone density, a decline in mental and memory processes, a reduction in sensory perceptions, a decrease in sexual activity, and an increased likelihood of developing chronic illnesses like cancer.
Certain diseases that are commonly associated with old age can be influenced by specific genes. Interestingly, individuals who remain free of these diseases despite their advanced age can attribute their resilience to genes that provide protection against these conditions. It is ironic that the same gene, in different forms, can have both positive and negative effects on a person’s well-being.
This article will briefly discuss some of the common age-related illnesses.
Heart Disease in Old Age
Heart disease, particularly Coronary Artery Disease (CAD), is the leading cause of death in individuals over the age of 70. High blood pressure is a common factor associated with aging and increases the risk of developing diseases such as stroke and heart failure.
Aging is accompanied by a decline in cardiovascular function. While this decline may not have a significant impact on individuals who are otherwise healthy and fit, it can exacerbate the situation or limit the effectiveness of therapy in individuals with pre-existing heart conditions.
Two genes associated with longevity, apoE and Angiotensin Converting Enzyme (ACE), are also related to heart disease. The apoE gene produces the protein apolipoprotein E, and the E2 variant of this gene is more commonly found in individuals who live longer, while the E4 variant predisposes individuals to heart disease and Alzheimer’s disease. The ACE gene plays a role in regulating blood pressure, and certain variants of this gene can impact the development of heart conditions.
It is intriguing how the same gene can have both positive and negative effects on the health of individuals. Additional analysis is required to fully understand the underlying mechanisms.
Age-Related Macular Degeneration
Age-related Macular Degeneration (AMD) is commonly recognized as the leading cause of visual impairment in individuals over the age of 60, particularly in developed nations. However, there is limited information available on macular degeneration in developing nations such as China and India.
Macular degeneration impacts the macula which is responsible for central vision. This type of vision is essential for activities like reading, driving, and recognizing faces.
Various factors have been implicated in the development of macular degeneration, including age, genetics, smoking, and nutrition. The genetic component of the disease is not well understood, although the apoE gene and its E4 variant have been associated with it.
In some individuals, the progression of the disease is slow, and they may not notice a significant change in their vision, while in others, it can progress more rapidly. Regular eye check-ups can help in the early detection of the disease, which in turn can facilitate the provision of appropriate therapies. These therapies can help slow down the progression of the disease but cannot fully restore vision.
Age-Related Hearing Loss/Presbycusis in Old Age
Presbycusis or age-related hearing loss refers to the slow loss of hearing that occurs as you age.
This type of hearing loss occurs when the tiny hair cells inside the ear get damaged.
Age-related hearing loss usually occurs due to:
- Repeated frontages of blasting noise to the ears
- Hereditary
- Medical conditions like diabetes
- Chemotherapy drugs
Osteoporosis in the Elderly
Osteoporosis is an illness that reduces bone viscosity, compelling the bones to be weak and breakable. The bones evolve abnormally spongy and compare to a sponge.
Osteoporosis is additionally ordinary among elder individuals, particularly in post-menopausal females. Hormone Replacement Therapy (HRT) is frequently the method of management. In many, the condition encroaches without signs. The sufferer may be clueless about the disease until an aching fracture happens. That is why aging is usually illustrated by slips and fractures, affecting different regions of the body.
Investigation indicates that osteoporosis is extremely related to aging. Even though a single gene hasn’t been involved, a mixture
of alleles of different genes has been comprehended to play a part in the condition.
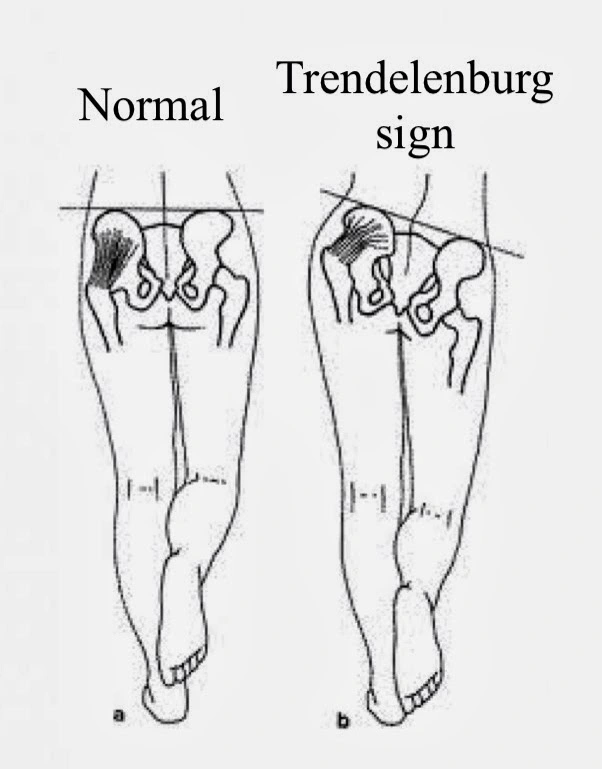
Falls in the Elderly
Falls in aged individuals usually guide to serious damage. One out of three individuals beyond the age of 65 years or more aged incident falls every year.
Some of the reasons conduct to decline in elders contain:
- Dizziness
- Vision problems
- Arthritis
- Weakness
- Malnutrition
- Falls may result in ruptures of the hip, spine, arms, pelvis, hands, or ankle.
Management for Falls:
Appropriate exercise, physical therapy, and walking benefit to strengthen the muscles and enhance balance to control falls.
It is even advisable that geriatric patients wear appropriate glasses to evade vision issues to stop falls.
Consult the doctor before accepting any prescriptions that can make you sense dizzy.
Examples of Chronic Geriatrics Diseases
During this is by no means a wide list of conditions undergone in elder adults, these and other chronic diseases are among the more typical:
- Arthritis
- Cancer
- Chronic Kidney Disease
- Chronic Obstructive Pulmonary Disease
- Dementia, Alzheimer’s, and Parkinson’s
- Diabetes
- Osteoporosis
- Stroke
Arthritis
This chronic illness is the most ordinary age-associated illness which elder adults experience. Arthritis induces joint pain and chronic swelling. Arthritis is classified into two types: osteoarthritis & rheumatoid arthritis. Osteoarthritis the more ordinary of the two, is an outcome of regular wear and tear in joints. Rheumatoid arthritis is an autoimmune condition in which the immune system attacks the joint lines.
There is no treatment for arthritis, but it can be controlled with analgesics and corticosteroids. Symptoms contain:
- Pain, stiffness, and tenderness in the joints
- Swelling near joints
- Limited/restricted activity
Cancer
With around 200 various forms of cancer breast cancer, prostate cancer, and lung cancer only to name a few, this is one of the most ordinary problems that elder individuals. Cancer happens via the quick and irregular double of cells in the body, including tumors that can lay via the bloodstream.
Treatments have been found for many kinds of cancer, cancer treatment can be incredibly invasive and carries a significant charge on the body. Regardless, the earlier it is caught, the more useful the possibility of defeating it. It is a suitable concept to consider executing a routine cancer screening. Here is the common manifestation:
- Discovery of a surprising lump/mass
- Unexplainable weight loss
- Blood in a person’s stool, urine, or vomit, while coughing
Why is Cancer a Disease of the Old Age?
Aging is associated with an increased risk of developing cancer. While cancer can affect individuals of all ages, it is predominantly considered a disease of aging.
There are several reasons for this, but one plausible explanation is the accumulation of chromosomal changes, which are a hallmark of cancer, as we age. Chromosomal abnormalities increase with each generation, and as individuals grow older, they are exposed to a greater variety of mutagens and carcinogens that can induce these abnormalities.
The human body possesses a surveillance system that identifies and repairs DNA abnormalities. However, the efficiency of this surveillance system weakens with age, making older individuals more susceptible to developing cancer.
Furthermore, the apoE genes, which are associated with aging and heart disease, are also linked to tobacco-related cancers.
Some of the common cancers that tend to develop with aging include colorectal cancer, breast cancer, and tobacco-related cancers.
In older individuals, the treatment approach for cancer aims to cure the disease if it is diagnosed early. However, if curative treatment is not feasible, the focus shifts to managing the disease by alleviating symptoms and improving quality of life.
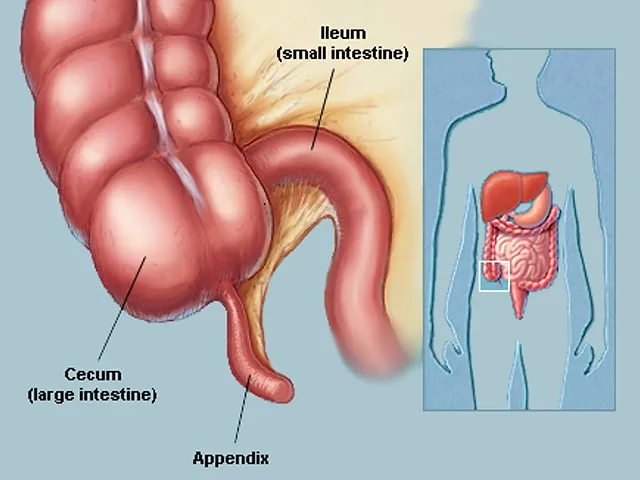
Chronic Kidney Disease
Kidney illnesses, kidney swelling, high blood pressure, and diabetes can all guide to chronic kidney disease. This illness impacts the kidneys and can guide to kidney defeat, and there is currently no treatment. Another painful fact is that early signs don’t generally occur rather, the situation is usually determined via urine tests ordered for other medical requirements.
Elder adults need to thus be engaged in documenting the ensuing later-stage signs to their doctor as soon as they find them:
- Bloody urine
- Shortness of breath
- Swollen ankles, hands, or feet
- Tiredness or a feeling of sickness
Chronic Obstructive Pulmonary Disease
The best-known circumstance beneath this variety of illnesses is chronic bronchitis. Bronchitis is induced by a disease involving the lungs and airways, contributing to a buildup of extreme slime. The body attempts to replace this buildup via coughing.
Smoking is one of the largest contributing aspects to the outcome of chronic bronchitis, which indicates that quitting is the best manner to overpower it. A healthy diet is even necessary as are rest, hydration, and the therapy of headaches.
Symptoms of bronchitis contain:
- Chest pain
- Fatigue
- Hacking, productive cough
- Headaches
- Runny nose or congestion
- Sore throat
- Neurological MRI Diagnosis
Dementia, Alzheimer’s Disease, and Parkinson’s Disease
Dementia is an umbrella word utilized to define a syndrome or a group of chronic illnesses in elder adults that guide issues with remembering and awareness. This happens when there is an injury of brain cells or a defeat of association between cells that leads to them breaking. Signs of dementia contain:
- Memory defeat
- Problem with vocal expression
- Efforts with visual/spatial capabilities
- The problem with problem-solving/reasoning
- Problem control complicated tasks, planning, crucial thinking skills, and organization
- The reduction in coordination with motor functions
- Confusion and disorientation
- Personality differences
- Unsuitable manners
- Depression, stress, paranoia, and agitation
- Hallucinations
Alzheimer’s disease is a specific kind of dementia, accounting for up to 70% of patients. Induced by disruptive buildups of proteins in the brain, the signs of Alzheimer’s contain:
- Problem recalling particulars about individuals, places, or events
- Problem focusing
- Modifications to one’s personality such as disinterest, nervousness, or aggression
- Apathy and depression
- Mood changes
- Confusion
- Poor judgment/judgment-making capabilities
- Problems with speaking, swallowing, or walking
Parkinson’s disease is another kind of dementia. This developed disease is induced by a defeat of nerve cells in the brain, which decreases the quantity of dopamine essential for normal mental functioning. During there is no treatment, the signs can be regaled. Here is what to examine out for:
- Spontaneous trembling of separate parts of the body
- Muscles that are rigid and inflexible
- Slow action
What are the Neurological Ailments in the Elderly?
Alzheimer’s disease is relatively general among elder people. But the earlier beginning domestic type of the disease is understood to happen before the age of 60 years. Earlier beginning disease impacts from mutations in the genes that code for the proteins called ‘presenilins.’ The late-onset illness, regardless, affects the E4 variant of the apo E gene which is also involved in heart diseases.
There is a decrease in mental function in elder people. And this is particularly seen in smokers & drinkers. The variants of the apoE gene are also accepted to recreate a part.
The elder an individual, the more prominent the risk of sorrowing a stroke. A stroke can transform the lives of the sufferer and even those implicated in patient maintenance.
Diabetes
Diabetes can produce while middle age and occasionally also in younger. But it most naturally evolves among elder adults, and it has to be handled as a lifelong illness. This disease happens when the body isn’t capable to assemble adequate insulin to provide regular functioning.
The most ordinary type of diabetes is Type II diabetes. This is when the pancreas isn’t elongated and qualified of constructing the proper quantity of insulin. An individual possibility of acquiring diabetes can be decreased via lifestyle modifications, contains:
- A healthy diet
- A healthy weight
- Regular exercise
Type I diabetes accounts for approximately 10% of general patients. It is an autoimmune disease, in which the body attacks the cells that construct insulin.
Diabetes in Elderly
Diabetes mellitus is characterized by high blood sugar levels, and the incidence of diabetes tends to increase with age. Elder adults are at a more increased chance of developing diabetes.
There are several factors that contribute to the elevated risk of diabetes in older adults:
- Increased insulin resistance: As individuals age, their cells may become less responsive to insulin, which leads to higher blood sugar levels.
- Impaired pancreatic islet function: The cells in the pancreas that produce insulin may experience age-related dysfunction, resulting in inadequate insulin production.
Diabetes in older patients is often associated with declining levels of mental function or increased cognitive impairment.
It is crucial for elderly patients to follow the necessary medical treatment to effectively manage diabetes.
Furthermore, appropriate geriatric assessment should be conducted to ensure that there is no risk of severe hypoglycemia associated with the use of insulin.
The American Diabetes Association (ADA) also recommends that geriatric patients with diabetes adhere to an appropriate diet and exercise regimen to effectively manage their condition.
Osteoporosis
Osteoporosis is one of the most common illnesses among older adults. This condition involves a decrease in bone density, and it often goes unnoticed until a fall leads to a bone fracture. Similar to the decline in muscle mass, decreased bone strength is a part of the natural aging process, but individuals with osteoporosis experience a more rapid decline than those without the condition.
Osteoporosis can be treated with medications and supplements such as calcium and vitamin D. Weight-bearing activities and exercises designed to improve muscle strength can also help older adults manage the condition.
Stroke
A stroke happens when the essential blood flow in the brain is cut off. This leads to brain cells starving, it can guide to an enduring disability, and it can be life-frightening. Strokes are very ordinary among elder adults, so it is essential to know the signs & symptoms so you can pursue medical awareness as soon as practicable. A useful acronym (FAST) makes it more comfortable to recognize.
- the face drooping on one side.
- Arms are the person unable to lift both arms.
- Speech is speech slurred.
- If so, don’t waste time seeking medical attention instantly.
How to Manage Geriatrics Disease?
Geriatric diseases are constant occasionally also permanent and so they need periodic concentration. Elder adults should believe in controlling a chronic care management team in a position to assist them to gain their health aims and hold their quality of life (QOL). This is specifically true of senior patients who are handling multiple chronic illnesses at a time.
As more elder adults undergo more age-related modifications, geriatric medication will evolve into an increasingly essential component of their medical regimen. More senior patients who are handling a chronic illness can help with the aid of a home nursing team. In addition to nutritional eating and a restorative lifestyle, frequent connection with dedicated therapists can assist control inadequate health.
Keystone Health delivers aid for elder patients in Idaho by delivering house calls and different conditions of care. Learn more about how we can support you preserve your quality of life throughout the aging procedure.
Here are some processes for geriatrics disease management:
- Regular health examinations: Regular health examinations can assist detect possible health issues earlier and control difficulties. Complete geriatric examinations can assist determine any medical, functional, and social problems that may impact the elder’s quality of life (QOL).
- Medication: Elder adults usually take considerable drugs, which can raise the chance of damaging drug exchanges and side effects. A geriatric expert can assist handle medications, observe for possible interactions, and modify dosages as required.
- Nutritional counseling: Correct nutrition is important for sustaining general health and controlling chronic illnesses. A registered dietitian can deliver an individualized dietary plan to assure that elders are obtaining the nutrients they require.
- Exercise programs: Everyday exercise is necessary for supporting mobility, strength, and general health. A physiotherapist can design an exercise schedule that is tailored to the elder’s precise requirements and capabilities.
- Fall prevention: Falls are a reason for damage in elder adults. A physiotherapist can assist in determining possible fall risks in the home and form methods to decrease the chance of falls.
- Social support: Social loneliness are typical among elder adults and can negatively affect physical and mental fitness. A geriatric professional can deliver social reinforcement and attach elders with assembly help and sponsorship organization.
- Chronic illness management: Chronic illnesses for example diabetes, hypertension, and heart disease are ordinary among elder adults. A geriatric expert can deliver instruction and assets for handling these situations and controlling difficulties.
Geriatrics disease administration demands a cooperative method that implicates doctors, guardians, and relatives. With appropriate care and administration, many geriatric diseases can be virtually controlled, and elders can hold their independence and quality of life (QOL).
FAQ
What are the 5 geriatric giants?
Geriatric giants contain a batch of circumstances that guide to considerable mortality and morbidity and contribute to the complexity of regaling old patients. They are typical and infrequently appear in isolation. The 5 is of aging giants are iatrogenesis, stiffness, instability, incontinence, and poor awareness.
What are geriatric age-related problems?
Regular diseases in the geriatric individual contain refractive mistakes, cataracts, hearing defeat, neck & back pain and osteoarthritis (OA), chronic obstructive pulmonary disease (COPD), diabetes, depression, and dementia. As individuals age, they are additionally conceivable to encounter several situations at the same period.
What is geriatric failure?
Indications of these circumstances contain weight loss, reduced appetite, inadequate nutrition, and laziness. Four syndromes are general and predictive of damaging results in patients with defeat to succeed: insufficient physical function, malnutrition, depression, and mental impairment.
What are geriatric factors?
We explained geriatric risk factors as health quality features ordinary in elder adults who have the possibility to be moderated upon and facilitated if recognized in a punctual way. These risk factors may not be universal/even generally considered despite their connection with low-grade results in elder adults.
What are the aims of geriatric care?
Geriatric care benefits aged individuals who control their general health and well-being and preserve their independence for function as long as doable.




5 Comments