Knee Pain at the Back of the Knee
What is Knee Pain at the Back of the Knee?
The back of the knee, also known as the popliteal fossa, is a complex anatomical region with a network of structures, including muscles, tendons, ligaments, and nerves. Knee Pain at the Back of the Knee may be due to several reasons, such as injuries, overuse, degenerative conditions, or underlying medical issues.
Baker’s cysts, a type of cyst, or arthritis can both produce pain at the back of the knee. A buildup of joint fluid behind the knee is called a Baker’s cyst. In general, knee discomfort may be caused by bursitis, osteoarthritis, rupture in the ligaments, or infection.
Reasons behind the back of the knee pain:
There are various causes of knee discomfort. Your risk of developing knee issues increases if you are overweight. Overuse of the knee can lead to painful knee problems. It could also result in knee pain if you have a history of arthritis.
- Leg cramps
- Jumper’s knee
- Biceps femoris tendonitis
- Baker’s cyst
- Gastrocnemius tendonitis
- Meniscus tear
- Anterior cruciate ligament injury
- Posterior cruciate ligament injury
- Arthritis
- Deep vein thrombosis
Leg cramps:
- A cramp is a spasm of taut muscle. Although the muscles in the calves are more prone to cramping, other leg muscles, such as those in the back of the thigh close to the knee, can also experience this condition.
- Leg cramps are more likely to occur during pregnancy or after physical activity. Additional potential reasons include of:
- nerve problems in your legs
dehydration
infections, such as tetanus
poisons in the blood, such as lead or mercury
liver disease - Your muscle will suddenly contract, or spasm, when you have a cramp. Ten minutes to a few seconds is how long the agony lasts on average. The muscle may ache for a few hours following the spasm. Here’s how to relieve the discomfort and avoid getting leg cramps again.
Jumper’s knee:
- An injury to the tendon, which is the cord that joins your shinbone to your kneecap (patella), is known as a jumper’s knee. It can happen when you leap or change direction, such as when playing volleyball or basketball.
Biceps femoris tendonitis:
- Three muscles travel down the back of your thigh and make up the hamstring:
- semitendinosus muscle
semimembranosus muscle
biceps femoris muscle
Your knee can be bent due to these muscles - A pulled hamstring or hamstring strain is the term used to describe an injury to one of these muscles—excessive stretching of the muscle results in a hamstring strain. A full muscle tear may occur, and healing may take months.
- You will experience acute pain when your hamstring muscle is injured. Back of the knee discomfort is a result of biceps femoris tendinopathy, an injury to the muscle.
- Other symptoms include:
- swelling
bruising
weakness in the back of your leg
Athletes who run quickly in sports like track, basketball, tennis, or soccer frequently sustain this kind of injury. Preventing this injury can be achieved by stretching the muscles before playing.
Baker’s cyst:
- A fluid-filled sac that develops behind the knee is called a Baker’s cyst. Synovial fluid is the fluid found inside the cyst. Normally, your knee joint is lubricated by this fluid. However, excessive production of synovial fluid in the knee may occur if you have arthritis or a knee injury. The excess fluid may accumulate and develop into a cyst.
- Symptoms include:
- pain in and behind your knee
swelling behind your knee
stiffness and trouble flexing your knee
These symptoms can get worse when you’re active. If the tumor breaks, your knee will hurt sharply. - Sometimes, Baker’s cysts disappear by themselves. You could require physical therapy, steroid injections, or cyst extraction to treat a large or painful cyst. It’s critical to ascertain whether the cyst is being caused by an underlying issue, such as arthritis. If so, treating this issue first might cause the Baker’s cyst to disappear.
Gastrocnemius tendonitis:
- Your calf, or rear of the lower leg, is made up of the gastrocnemius and soleus muscles. These muscles assist you in pointing your toes and bending your knee.
- Tennis and squash are two sports that can cause strain or tears in the gastrocnemius muscle because they involve rapid transitions from a standing to a running position. The abrupt soreness in the back of your leg will indicate that this muscle is stretched.
- Other symptoms include:
- pain and swelling in the calf
bruising in the calf
trouble standing on tiptoe
Depending on the size of the rip, however, the pain should go away. The wounded area will recover more quickly if you rest, elevate the leg, and apply ice to it.
Meniscus tear:
- A meniscus is a wedge-shaped cartilage that stabilizes and cushions your knee joint. Each knee includes two menisci, one on each side.
- When an athlete squats and twists their knee, they may tear the meniscus. Your meniscus weakens and degenerates with age, increasing the likelihood that it will rip from any twisting motion.
- There may be a “popping” sound when a meniscus is torn. The injury might not hurt at first. But the knee may hurt more after a few days of walking on it.
Other symptoms of a meniscus tear are:
- stiffness in the knee
- swelling
- weakness
- locking or giving way of the knee
- The affected knee may heal more quickly and relieve symptoms with rest, ice, and elevation. If the rip does not heal itself, surgery may be required to fix it.
Anterior cruciate ligament injury:
- A band of tissue called the anterior cruciate ligament (ACL) passes through the front of your knee joint. It helps support and provide movement for your knee by joining your thighbone to the shinbone.
- The majority of ACL injuries occur when a runner unexpectedly shifts direction, slows down, or stops. Also, if you land a jump incorrectly or are struck in a contact sport like football, you run the risk of spraining or tearing this ligament.
- The injury might “pop” as it happens. Your knee will ache and swell after that. You may have pain when walking and find it difficult to fully extend your knee.
- An ACL strain can mend with physical treatment and rest. It is frequently necessary to have surgery to repair a damaged ligament. This is what to anticipate when reconstructing your ACL.
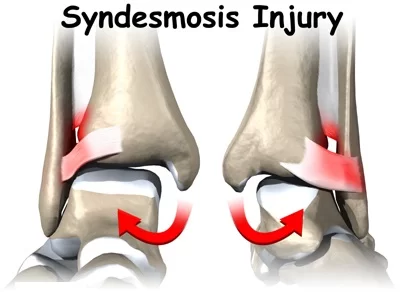
Posterior cruciate ligament injury:
- The ACL’s spouse is the posterior cruciate ligament (PCL). It is an additional ring of tissue that supports your knee and joins your shinbone to your thighbone. It should be noted that the PCL is less prone to injury than the ACL.
- If you get a forceful impact on the front of your knee, like in an automobile accident, you may injure the PCL. Injuries can occasionally result from walking and twisting the knee or forgetting a step.
- A strain is the result of overstretching the ligament. A sufficient amount of pressure might cause the ligament to split in two.
Arthritis:
- The degenerative condition known as arthritis causes the cartilage that supports and cushions the knee joint to gradually deteriorate. A few different kinds of arthritis can impact the knees:
- Osteoarthritis is the most common type. As you get older, your cartilage gradually breaks down.
An autoimmune condition called rheumatoid arthritis occurs when the body’s systems incorrectly target the joints.
Another autoimmune condition that inflames the knees and other joints is arthritis.
Skin rough patches and joint discomfort are symptoms of psoriatic arthritis.
Injections, painkillers, and physical activity can all help control the symptoms of arthritis.
Disease-modifying medications, which reduce inflammation in the body and decrease the immune system’s reaction, are used to treat rheumatoid arthritis and other inflammatory types of the illness.
Seek alternative methods of treating your arthritis pain.
- A blood clot that develops in a deep vein inside the leg is known as deep vein thrombosis (DVT). Leg soreness is likely to occur, especially when standing. This is how a blood clot can be detected.
- Other symptoms include:
- swelling of the leg
warmth in the area
red skin
Treatment for DVT must start as soon as possible. A loose clot may end up in the lungs. A pulmonary embolism occurs when a clot lodges in a lung artery (PE). PE carries the risk of being lethal. - Thinners are used to treat DVT. These medications inhibit the clot from growing larger and from generating additional clots. Your body will disintegrate the clot in due course.
- Your doctor may prescribe thrombolytics to break up large, potentially dangerous blockages more quickly.
Injuries and overuse:
- Bursitis: inflammation caused by prolonged strain on the knee, such as by prolonged kneeling, misuse, or trauma
- Tendinitis: Changes in activities that cause tendon inflammation may be linked to overuse or deconditioned tissue.
- kneecap dislocation
- fractured bones in the kneecap or somewhere
- Iliotibial band syndrome: damage to the thick band that extends from your hip to your knee’s outside
- Patellofemoral syndrome: pain near the kneecap on the front of your leg
- Torn ligament: An injury to the medial collateral ligament (MCL) or anterior cruciate ligament (ACL) may result in knee instability, edema, or bleeding into the knee.
- Torn cartilage (a meniscus tear): discomfort experienced either inside or outside the knee joint
- Strain or sprain: Ligament irritation from sudden or abnormal twisting
Home care of knee pain at the back side of the knee:
- Simple knee pain reasons frequently go away on their own while you manage your symptoms. You should get in communication with your healthcare practitioner if an accident or injury is the source of your knee pain.
- If your knee pain is mild at this point and has just started, you can:
- Rest and stay away from painful activities. Avoid bearing weight on your knee.
- Apply ice: Initially, apply it for up to 15 minutes every hour. Apply it four times a day at least after the first day. Before applying ice, wrap a cloth around your knee. When using ice, do not freeze off. The condition could result from leaving it on for too long.
- Try to keep your knee as elevated as you can to reduce any swelling.
- Use an elastic sleeve or bandage, which are available at most pharmacies. This could offer support and lessen edema.
- If you have discomfort or swelling, take naproxen or ibuprofen. Acetaminophen is useful for pain relief, but not for edema. If you have any health concerns or have been taking these medications for longer than a day or two, consult your doctor before using them.
- Use a pillow between your knees or behind you while you sleep.
- For general advice on preventing and treating knee discomfort, use these resources:
- It is important to always warm up before working out and cool down afterward. Stretch your hamstrings and quadriceps, the muscles located at the front and back of your thigh, respectively.
- Walk down hills rather than running along.
- Rather than running, take a bicycle or, better yet, a swim.
- Reduce your exercise program.
- Run on a soft, smooth surface, like a track, rather than a sidewalk or stone.
- If you are overweight, please lose weight. When you go up and down stairs, each ounce of excess weight adds around five kilograms of strain to your kneecap. When you jump, the additional pressure increases even more. Ask your doctor for advice on weight loss.
- Try using arch supports and specialty shoe inserts if you have flat feet.
- Make sure the support, fit, and construction of your running shoes are all excellent.
When to Contact a Medical Professional:
- Your knee cannot support your weight.
- Even without carrying any weight, you are in severe pain.
- It clicks, buckles, and locks your knee.
- Your knee has a malformation or deformity.
- You struggle to fully extend your knee and are unable to flex it.
- You experience a high degree of swelling, redness, or warmth around the knee.
- Below the aching knee, you get calf discomfort, swelling, numbness, tingling, or bluish discoloration.
- Even after three days of at-home therapy, your pain remains.
When to see your doctor:
- Pain from arthritis or small injuries could be manageable at home. But if you experience any of the following, contact your physician:
- The affected leg is red.
It is a swollen leg.
You’re aching.
You have a fever.
You’ve suffered blood clots in the past.
They can identify the underlying reason for your knee discomfort and assist you in getting better. - Additionally, you should get help right away if you’re feeling any of the following:
- severe pain
sudden swelling or warmth in the leg
trouble breathing
a leg that can’t hold your weight
changes in the appearance of your knee joint
What to Expect at Your Office Visit:
- Your doctor will examine your knees, hips, legs, and other joints during a physical examination.
- Your provider may do the following tests:
- X-ray of the knee
MRI of the knee to see whether there is a possible meniscus or ligament rupture
CT scan of the knee
Fluid collected from the knee and analyzed under a microscope is known as joint fluid culture.
To relieve pain and inflammation in your knee, your doctor could administer a steroid injection. - Stretching and strengthening activities might be necessary for you. To get fitted for orthotics, you might also need to visit a podiatrist.
- In some cases, you may need surgery.
- Treatment of knee pain at the back side of the knee:
- Making sure that the muscles surrounding the knee, particularly the hamstrings, calf, and quads, are correctly stretched is a good idea at all times. While it might not offer protection against all traumatic sources of knee discomfort, this could improve the way the muscles react to exercise.
- When an injury first happens, doctors frequently advise the RICE method to help reduce pain and swelling. RICE is a shorthand for:
- Resting (the leg)
Icing (the knee)
Compressing (the area with an elastic bandage)
Elevating (the injured leg)
Summary
Baker’s cysts, a type of cyst, or arthritis can both produce pain at the back of the knee. A buildup of joint fluid behind the knee is called a Baker’s cyst. In general, knee discomfort may be caused by bursitis, osteoarthritis, rupture in the ligaments, or infection.
FAQ
What does it mean to have pain behind the knee from the back of your leg?
There are several reasons. As you age, your knee joint can weaken or you may sustain an injury that tears cartilage or a ligament in your knee. A popliteal cyst and an injury to the posterior cruciate ligament are two common disorders that produce pain behind the knee.
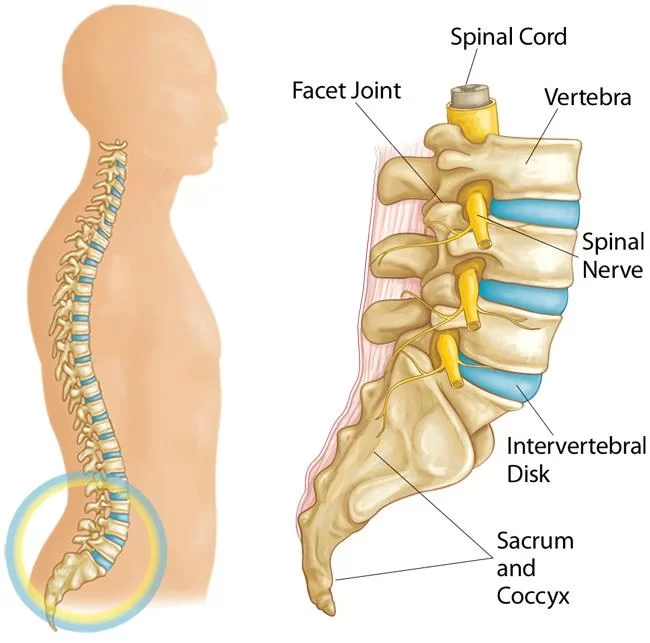
What is the reason for back discomfort in the knees?
One of the spinal nerves, the sciatic nerve, runs from your lower back through your leg and into your knee. Sciatica can cause knee pain and feels like a shooting pain that travels down your leg from your lower back. Usually, it has another underlying cause, such as damage or degeneration of the nerves.
When knee discomfort occurs, is it better to rest or walk?
Once more, RICE (rest, ice, compress, elevate) should be applied to the affected area for a minimum of 48 hours if you have sprained, dislocated, or, in the worst case scenario, shattered your kneecap. Walking, however, can eventually be beneficial for people with long-term (chronic) arthritis.
How long does it take for knee or back pain to go away?
The time it takes for a knee injury to heal can vary based on many factors. It may take two weeks to nine months for common knee injuries to fully heal. Small cuts don’t require extensive medical attention. Other injuries can require surgery, physical therapy, and a protracted recuperation period.
How can I tell whether the pain in my knee is severe?
It clicks, buckles, and locks your knee. Your knee has a malformation or deformity. You struggle to fully extend your knee and are unable to flex it. You experience a high degree of swelling, redness, or warmth around the knee.
References
- Why Knees Hurt. (n.d.). WebMD. https://www.webmd.com/pain-management/knee-pain/ss/slideshow-why-knees-hurt
- Watson, S. (2023, January 18). What’s Causing This Pain in the Back of My Knee? Healthline. https://www.healthline.com/health/pain-in-back-of-knee
- Image, Wilson, C. (2021, September 28). Pain Behind The Knee: Causes & Treatment. Knee-Pain-Explained.com. https://www.knee-pain-explained.com/pain-behind-the-knee.html






3 Comments