Muscle of ankle and intex
Superficial Posterior Compartment :
Gastrocnemius Muscle :
Gastrocnemius forms the major bulk at the back of lower leg and is a very powerful muscle .
The gastrocnemius muscle (plural gastrocnemii) is a superficial two-headed muscle that is in the back part of the lower leg of humans. It runs from its two heads just above the knee to the heel, a three joint muscle (knee, ankle and subtalar joints).
The muscle is named via Latin, from Greek ?ast?? (gaster) ‘belly’ or ‘stomach’ and (kn?me) ‘leg’, meaning ‘stomach of leg’ (referring to the bulging shape of the calf).
Anatomy :-
Origin :-
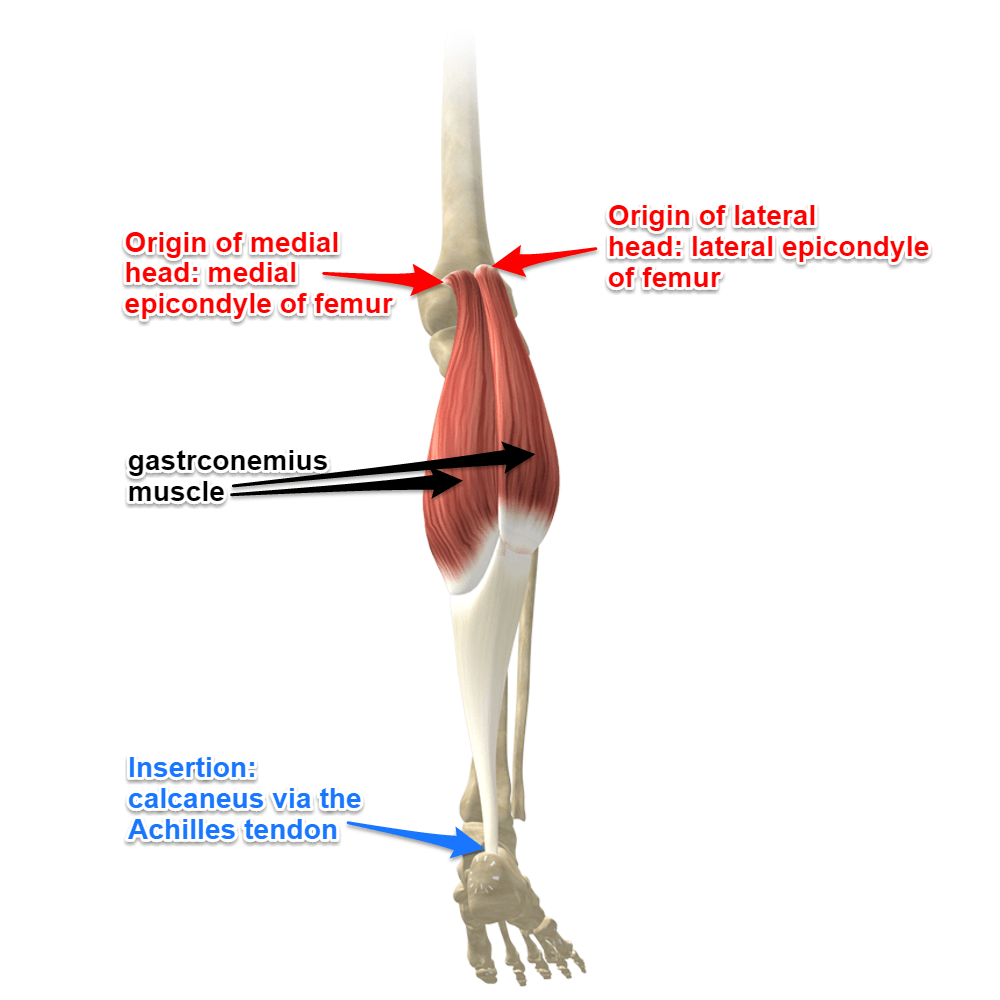
The two heads are located from the medial and lateral condyles of the femur.
The medial head from behind the medial supercondylar ridge and the adductor tubercle on the popliteal surface of the femur.
The lateral head from the outer aspect of the lateral condyle of the femur, just superior and posterior the lateral epicondyle.
Both heads have attachments from the knee joint capsule and from the oblique popliteal ligament .
Insertion :-
The bulk of the gastrocnemius muscle from each of the heads come together and insert into the posterior surface of a broad membranous tendon.
It then fuses with the soleus tendon to form the upper part of tendocalcaneus.
This broad tendon then narrows until it reaches the the calcaneous where it expands again for its insertion on the middle part of the posterior surface of the calcaneus .
Nerve supply :-
Both heads of the gastrocnemius is supplied by the tibial nerve (S1 and 2). Cutaneous supply is mainly provided by L4, 5 and S2 .
Structure :-
The gastrocnemius is located with the soleus in the posterior (back) compartment of the leg.
The lateral head originates from the lateral condyle of the femur, while the medial head originates from the medial condyle of the femur.
Its other end forms a common tendon with the soleus muscle; this tendon is known as the calcaneal tendon or Achilles tendon and inserts onto the posterior surface of the calcaneus, or heel bone.
It is considered a superficial muscle as it is located directly under skin, and its shape may often be visualized through the skin.
Deep to the gastrocnemius (farther from the skin) is the soleus muscle.
Some anatomists consider both to be a single muscle—the triceps surae or “three-headed [muscle] of the calf”—since they share a common insertion via the Achilles tendon.
The plantaris muscle and a portion of its tendon run between the two muscles, which is involved in “locking” the knee from the standing position.
Since the anterior compartment of the leg is lateral to the tibia, the bulge of muscle medial to the tibia on the anterior side is actually the posterior compartment. The soleus is superficial to the mid-shaft of the tibia.
Innervation and blood supply :-
The gastrocnemius is innervated by the ventral rami of S1 and S2 spinal nerves, carried by the tibial nerve into the posterior compartment of the leg.
Both medial and lateral heads of gastrocnemius are supplied by the lateral and medial sural arteries, which are direct branches of the popliteal artery.
The arteries arise in the popliteal fossa, although the level at which these arteries arise is variable, with the medial sural artery usually arising more proximally and the lateral more distally.
Minor accessory sural arteries may also branch off the popliteal and superior genicular arteries.
Venous drainage is through corresponding medial and lateral sural veins into the popliteal vein .
Arterial Supply :-
Each head supplied by a sural branch of the popliteal artery
Function :-
Along with the soleus muscle, the gastrocnemius forms half of the calf muscle.

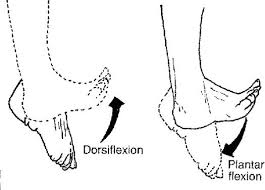
Its function is plantar flexing the foot at the ankle joint and flexing the leg at the knee joint.

The gastrocnemius is primarily involved in running, jumping and other “fast” movements of leg, and to a lesser degree in walking and standing.
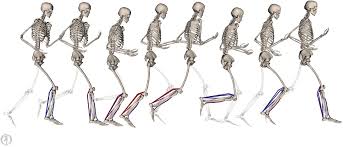
This specialization is connected to the predominance of white muscle fibers (type II fast twitch) present in the gastrocnemius, as opposed to the soleus, which has more red muscle fibers (type I slow twitch) and is the primary active muscle when standing still, as determined by EMG studies.
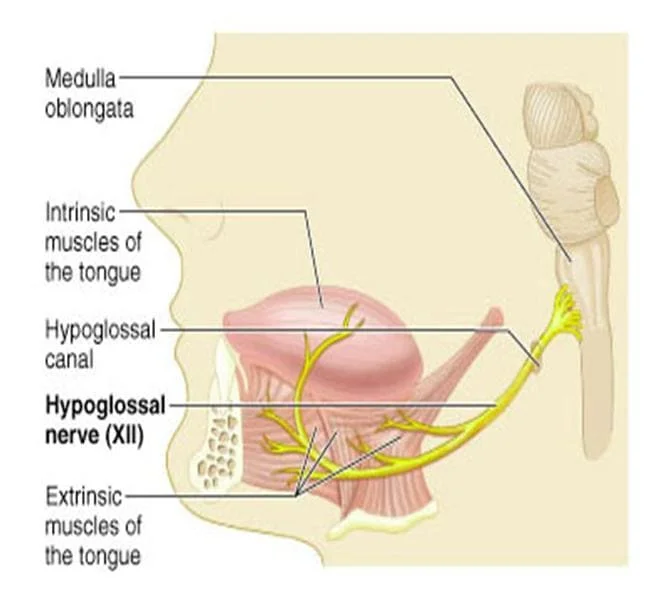
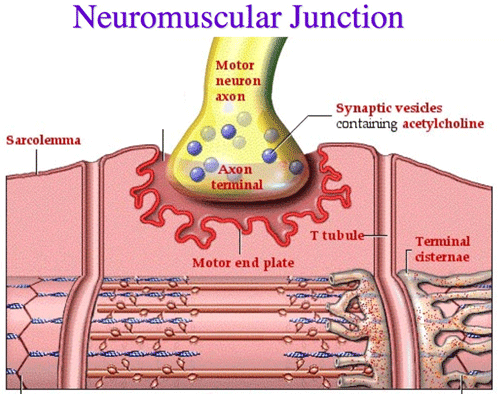
Motor pathway :-
The plan to use the gastrocnemius in running, jumping, knee and plantar flexing is created in the precentral gyrus in the cerebrum of the brain.
Once a plan is produced, the signal is sent to and down an upper motor neuron.
The signal is passed through the internal capsule and decussates, or crosses, in the medulla oblongata, specifically in the lateral corticospinal tract.
The signal continues down through the anterior horn of the spinal cord where the upper motor neuron synapses with the lower motor neuron.
Signal propagation continues down the anterior rami (Lumbar 4-5 and Sacral 1-5) of the sacral plexus.
The sciatic nerve branches off of the sacral plexus in which the tibial and common fibular nerves are wrapped in one sheath.
The tibial nerve eventually separates from the sciatic nerve and innervates the gastrocnemius muscle.
Thus, completing the plan the brain had originally started with, so that the actions of running, standing, and jumping could be executed.
innervation :-
The gastrocnemius is innervated by the tibial nerve, a terminal branch of the sciatic nerve.
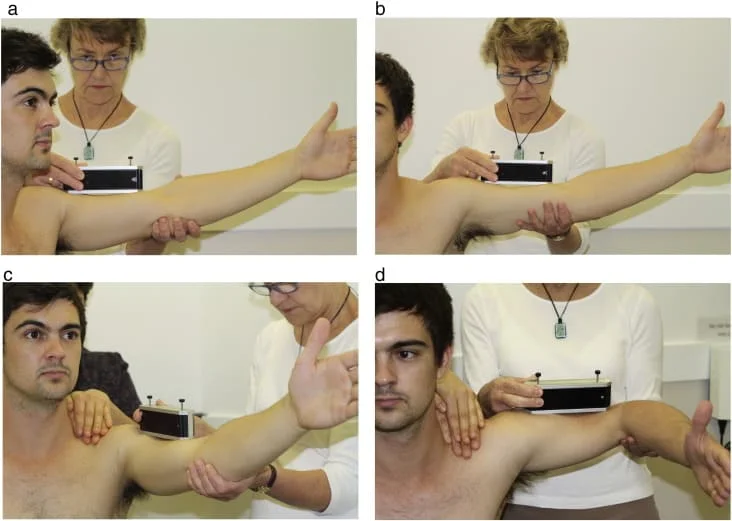
Assessment :-
Palpation :-
At the posterior aspect of the knee joint, the two large muscle bellies of gastrocnemius can be felt on either side of the upper portion of the calf.
The medial head is projects higher and is lower than the lateral.
Both can be felt joining the tendinous junction.
Further down the calf is the flattened tendocalcaneus which can be palpated to its insertional attachment at the posterior surface of the calcaneus .
Power :-
Ankle plantarflexion in long-sitting (consider that gastrocnemius works against full body on a daily basis).
Double/single leg calf raise
Straight leg jump
Functional tasks (steps, etc.)
Length :-
Passive dorsiflexion
Body-weight lunge, measure the straight back leg.
Treatment :-
Weakness :-
Nonweightbearing and basic weightbearing exercises such as theraband exercises, double and single leg calf raises.
Weight-bearing exercises and gradually progresses stability exercises by :-
(i) increasing load
(ii) increasing the repetitions
(iii) varying surface, for example introducing a wobble board
Sport-specific movement patterns such as running, jumping, and bounding.
Trigger Points :-
Gastrocnemius trigger points referred pain .
The gastrocnemius may contain up to four trigger points.
The two medial trigger points lie in the medial head of the gastrocnemius, with the upper trigger point found just below the crease of the knee, and the lower trigger point an inch or two below it.
The two lateral trigger points in the lateral head mirror the positioning of the medial trigger points, except that they lie slightly more distal (towards the foot) by about a half-inch .
Superficial Posterior Compartment :
Soleus muscle :
Introduction :-
Located in superficial posterior compartment of the leg Soleus is a powerfull lower limb muscle which along with gastronemius and plantaris forms the calf muscle or triceps surae. It runs from back of knee to the ankle and is multipennate.
Anatomy :-
Origin :-
posterior surface of the head and upper 1/3 of the shaft of the fibula
middle 1/3 of the medial border of the tibia, tendinous arch between tibia and fibula.
Insertion :-
Into calcaneus with gastrocnemius by way of achilles tendon
Nerve supply :-
Tibial nerve, L4, L5, S1 , S2
Blood supply :-
Blood supply of the soleus muscle is from peroneal artery proximally and the posterior tibial artery distally
Muscle has a mixed blood supply
Vascular supply of the soleus is from popliteal, posterior tibial, & peroneal vascular pedicles to the proximal muscle, peroneal pedicles to distal lateral belly, and segmental posterior tibial pedicles to distal medial belly
With distal pedicles from the posterior tibial artery ligated & based on proximal pedicles from the posterior tibial and peroneal arteries, muscle can be transposed medially or laterally to cover defects in middle third of the leg
Proximal vasculature arises directly from the popliteal vessels and can reliably carry all but the distal 4 to 5 cm of the muscle
Intramuscularly, vasculature of the soleus divides into a bipenniform segmental pattern
this vascular pattern, either half of the soleus muscle can be used, leaving a functional hemisoleus muscle intact
Function :-
Soleus has two major functions :-
To act as skeletal muscle: Along with other calf muscle it is powerfull plantarflexor and have major contribution in running,walking and dancing.In the seated calf raise (knees flexed approximately 90º), the gastrocnemius are virtually inactive while the load is borne almost entirely by the soleus.
In moderate force, the soleus is preferentially activated in the concentric phase, whereas the gastrocnemius is preferentially activated in the eccentric phase .
Human soleus muscle have majority of slow twitch fibers.Human soleus fiber composition is quite variable, containing between 60 and 100% slow fibers .
To act as muscle pump: along with other calf muscles it is known as peripheral heart as in uprite posture it enhance pumping the venous blood back into heart from periphery
Accessory soleus muscle (ASM) :-
It is present in 0.7 to 5.5% of humans.It is usually observed during the second or third decade of life and is more commonly seen in females than males at a ratio of 2:1.
It is mostly unilateral.This supernumerary muscle is located under the gastrocnemius muscle, in the posterior upper third of the fibula, in the oblique soleus line, between the fibular head and the posterior part of the tibia.
From its origin, the ASM runs anteriorly and medially until it reaches the Achilles tendon .
Depending upon its insertion it is of 5 types, or in other words it can origninate from 5 sites
Achilles tendon
Upper calcaneus region
Insertion in the upper calcaneus,
Medial calcaneus region,
Medial part of the calcaneus
Sometimes it is impossible to precisely identify the ASM origin and insertion, since the MRI fails to show details, depending on the slices.
Itmay cause pain on exercise. One may suspect a soft-tissue tumor, such as lipoma, hemangioma, and even sarcoma, but the anomalous muscle has a typical appearance on plain radiographs, and the appearance on computed tomography is diagnostic.
If the patient is asymptomatic, no therapy is required, but if pain or other discomfort is provoked by exercise, exploration with fasciotomy or excision of the accessory muscle is recommended, as was done in six of our eleven patients who were seen between 1968 and 1985
Structure :-
The soleus is located in the superficial posterior compartment of the leg.
The soleus exhibits significant morphological differences across species. It is unipennate in many species.
In some animals, such as the rabbit, it is fused for much of its length with the gastrocnemius muscle.
In the human, soleus is a complex multi-pennate muscle, usually having a separate (posterior) aponeurosis from the gastrocnemius muscle.
A majority of soleus muscle fibers originate from each side of the anterior aponeurosis, attached to the tibia and fibula .
Other fibers originate from the posterior (back) surfaces of the head of the fibula and its upper quarter, as well as the middle third of the medial border of the tibia.
The fibers originating from the anterior surface of the anterior aponeurosis insert onto the median septum and the fibers originating from the posterior surface of the anterior aponeurosis insert onto the posterior aponeurosis .
The posterior aponeurosis and median septum join in the lower quarter of the muscle and then join with the anterior aponeuroses of the gastrocnemius muscles to form the calcaneal tendon or Achilles tendon and inserts onto the posterior surface of the calcaneus, or heel bone.
In contrast to some animals, the human soleus and gastrocnemius muscles are relatively separate, such that shear can be detected between the soleus and gastrocnemius aponeuroses .
The Soleus is vestigial in the horse.
Relations :-
The gastrocnemius muscle is superficial to (closer to the skin than) the soleus, which lies below the gastrocnemius.
The plantaris muscle and a portion of its tendon run between the two muscles. Deep to it (farther from the skin) is the transverse intermuscular septum, which separates the superficial posterior compartment of the leg from the deep posterior compartment.
On the other side of the fascia are the tibialis posterior muscle, the flexor digitorum longus muscle, and the flexor hallucis longus muscle, along with the posterior tibial artery and posterior tibial vein and the tibial nerve.
Since the anterior compartment of the leg is lateral to the tibia, the bulge of muscle medial to the tibia on the anterior side is actually the posterior compartment.
The soleus is superficial middle of the tibia.
Clinical significance :-
Disease :-
Due to the thick fascia covering the muscles of the leg, they are prone to compartment syndrome. This pathology relates to the inflammation of tissue affecting blood flow and compressing nerves. If left untreated compartment syndrome can lead to atrophy of muscles, blood clots, and neuropathy.
Pathology :-
Strain/Rupture :-
Full or partial rupture of the soleus muscle usually occurs when the calf muscle becomes stretched while it is contracting (eccentric contraction).
Partial ruptures represent the majority of the ruptures.
The rupture occurs in many instances at the point of attachment of the soleus muscle to the Achilles tendon, which will often trigger an inflammation of the Achilles tendon as a result of the soleus rupture.
Symptoms:-
Pain when activating the calf muscle (running and jumping), when applying pressure on the Achilles tendon approx. 4 cm. above the anchor point on the heel bone or higher up in the calf muscle, and when stretching the tendon.
Walking on tip-toe will aggravate the pain.
In all cases when there is a sense of a “crack”, or sudden shooting pains in the Achilles tendon, medical attention should be sought as soon as possible.
Ultrasound scanning or MRI examination is used to advantage when making the diagnosis, as even full ruptures can easily be overlooked by normal clinical examination .
Further, about the soleus and calf strain can be read here
Whenever there occurs calf strain and the soleus is the muscle affected then there occur usually the medial or lateral pain i.e along the soleus fibres.
And when the pain is in the bulk of the calf muscle then the gastrocnemius is the muscle affected,but, mostly both the muscles are affected together.
Soleus Syndrome :-
Another cause of medial pain (posteriomedial aspect of ankle) just above the medial malleous is the soleus syndrome.
It occurs because of abnormal sliping of soleus muscle from its normal origin site and is similar to exertional campartment syndrome and commaly seen in dancers and athlets.
Respond well to conservative treatment and if not then rarely fasciotomy of the soleus insertion may be required .
Mechanism of injury :-
The potential underlying causes of soleus strain include (but are not limited to) :-
Training error – overtraining, rate of increase of training loads too high, introduction of too much hill work over too short a time, poorly designed training program – eg a hard running session after a long run
Kinetic chain dysfunctions – poor hip extension flexibility and associated poor gluteus maximus recruitment.
This is a common problem in triathletes or runners that sit for long periods for work.
Past injury – to the ankle plantar flexors, the ankle joint or the Achilles or plantar fascia.
Poor strength-endurance of ankle plantar flexors.
Footwear – a change leading up to the injury (eg change in heel counter, pronation control).
Running technique – conscious change in running technique to mid-forefoot running or running technique modified by footwear type.
Rehabilitation :-
There are two considerations during rehabilitation :-
Rehabilitating the injured muscle so it is physiologically and neurologically capable of returning to the desired capacity for running.
Ensuring the identified underlying causes play less of a role in overloading the soleus muscle during future running.
In the acute stage of injury, the goal is to manage the muscle, as with any other type of low-grade strain.
Ensure the athlete rests and manages the pain and swelling. After a bit of rest, the athlete may think they have recovered. However, soleus strains are notorious for returning when the athlete ‘feels better’.
Often an athlete will resume running and after a few kilometers intense tightening begins.
Little specific information with regard to rehabilitation of the soleus muscle exists in the literature.
The following guidelines have therefore been developed from a combination of adhering to general guidelines for muscle strain rehabilitation, and the training/rehabilitation principles of overload and specificity.
Successfully rehabilitating a soleus muscle involves doing three things well:
Developing strength/endurance of ankle plantar flexors :-
Strengthening exercises for the ankle plantar flexors involve calf raises with both straight knees for gastrocnemius activation and knees bent for the soleus.
Begin with both legs on the ground then progress to double legs on the stairs, single leg on the ground and finally single leg on the stairs.
Complete two sets each of knee straight and knee bent. Very high repetitions using the athlete’s body weight will focus on strength/endurance, which relates to distance running (as opposed to a sprinter’s requirement of high load for maximal strength).
The initial goal is to perform four sets of 20 repetitions on a single leg stair raise in one session with 2-minute rest intervals.
The end goal will be dependent on the level of the runner and the training loads intended.
Developing power/endurance of the ankle plantar flexors :-
Athletes should begin hopping exercises after achieving adequate endurance with single leg raises.
These should not be maximal jump/hop height exercises, which would preferentially recruit the fast-twitch dominant gastrocnemius muscle.
Instead, they should be rather moderate level hopping exercises that mimic the stretch-shortening cycle of soleus, which occurs in running.
Hopping should begin on two legs (mini continuous jumps) and progress to single leg.
A high level of power endurance can be considered four sets of 100 hops, but you take individual considerations into account.
If completing a rehabilitation session, the power exercises should be done before the strength/endurance exercises to ensure dynamic exercises are not performed in a fatigued state, which reduces the chance of re-injury.
Graded return to running :-
Commonly, athletes will ‘feel good’ when beginning running and just keep going until they experience the familiar tightness.
This puts their rehabilitation back a couple of weeks.
Educate athletes with regard to the importance of following the designated distances and intensity, and to resist doing a little more upon feeling good! As a guide, begin two runs per week: one kilometer on the first run maximum, and add no more than one kilometer at a time to running sessions.
As the rehabilitation progresses, induce overload to produce muscle remodeling.
This can result in mild soreness over the strain site and generalized delayed onset muscle soreness (DOMS).
Allow enough time for recovery and avoid performing a running session too soon after a rehabilitation session.
During rehabilitation, the soleus muscle will suffer from trigger points and range of movement restrictions.
As needed, perform regular dry needling to trigger points, deep tissue massage and stretching.
Also, encourage athletes to perform daily self-massage techniques like foam rolling and a home-stretching program .
Although soleus muscle rehabilitation deserves more attention in research, it is hoped that this article has provided both background information on soleus muscle strain in distance runners, and a framework for approaching rehabilitation.
Action :-
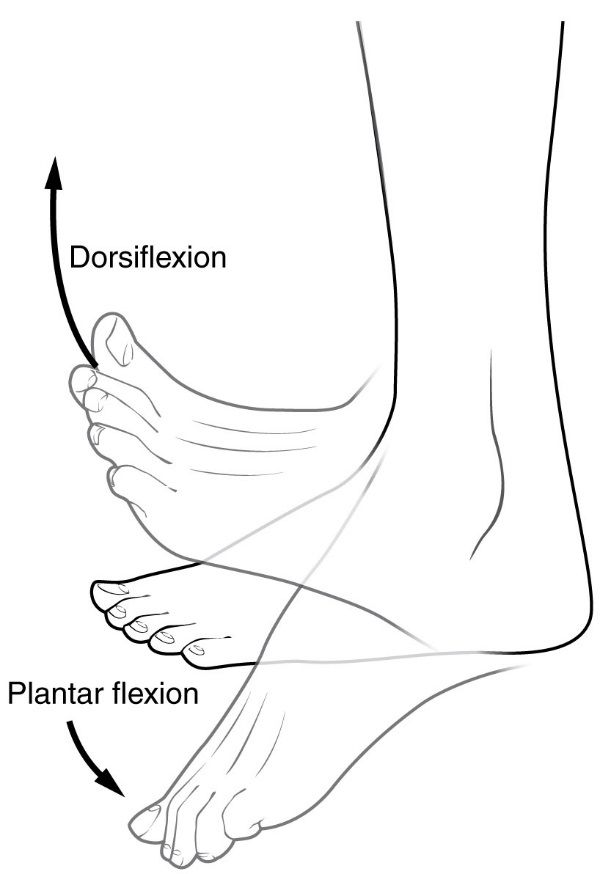
Plantar flexion of the foot at the ankle
Reversed origin insertion action: when standing, the calcanius becomes the fixed origin of the muscle
Soleus muslce stabilizes the tibia on the calcaneus limiting forward sway .
Superficial Posterior Compartment :-
Plantaris Muscle :

Plantaris muscle
Introduction :-
The plantaris is one of the superficial muscles of the superficial posterior compartment of the leg, one of the fascial compartments of the leg.
It is composed of a thin muscle belly and a long thin tendon. While not as thick as the achilles tendon, the plantaris tendon (which tends to be between 30–45 centimetres (12–18 in) in length) is the longest tendon in the human body.
Not including the tendon, the plantaris muscle is approximately 5–10 centimetres (2.0–3.9 in) long and is absent in 8-12% of the population.
It is one of the plantar flexors in the posterior compartment of the leg, along with the gastrocnemius and soleus muscles.
The plantaris is considered an unimportant muscle and mainly acts with the gastrocnemius.
Anatomy :-
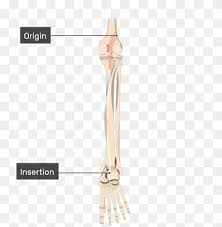
Plantaris origin and insertion
Origin :-
Lateral supracondylar line of femur, oblique popliteal ligament of knee
Insertion :-
Posterior surface of calcaneus (via calcaneal tendon)
Nerve supply :-
tibial nerve from anterior rami of S1-S2
Artery :-
Blood supply to the plantaris muscle is from the popliteal artery.
Innervation :-
Tibial nerve (S1, S2)
Blood supply :-
Superficially :-
lateral sural and popliteal arteries
Deeply :-
superior lateral genicular artery
Actions :-
Talocrural joint :- foot plantar flexion
Knee joint: knee flexion
Primary Actions of the Plantaris :-
- The plantaris muscle is not a prime mover and does not have a primary action but assists with the actions of other muscles at the knee and ankle joints.
Secondary Actions of the Plantaris :-
- Assists with flexion of the knee :-
Agonists :-
Biceps Femoris
Semitendinosus
Semimembranosus
Antagonists :-
Vastus Lateralis
Vastus Medialis
Vastus Intermedius
Rectus Femoris
- Assists with plantarflexion of the foot at the ankle :-
Agonists :-
Gastrocnemius
Soleus
Antagonists :-
Tibialis Anterior
Structure :-
The plantaris muscle arises from the inferior part of the lateral supracondylar ridge of the femur at a position slightly superior to the origin of the lateral head of gastrocnemius.
It passes posterior to the knee joint in an inferomedial direction and becomes tendinous distally to insert into the Achilles tendon.
It occasionally separately inserts into the medial side of the calcaneus.
Innervation :-
The plantaris muscle is innervated by the tibial nerve, a branch of the sciatic nerve in the sacral plexus.
Signaling for contraction begins in the frontal lobe of the brain with the pre-central gyrus (primary motor cortex).
Upper motor neurons are stimulated and send a signal through the internal capsule and down the corticospinal tract.
Decussation of the lateral corticospinal tract occurs in the medullary pyramids, then the fibers continue down the contralateral side of the spinal cord.
Upper motor neurons synapse with lower motor neurons at the anterior horn of the spinal cord in the sacral plexus (formed from the anterior rami of spinal nerves L4, L5, S1–4).
The lower motor neuron fibers continue down the sciatic nerve and then diverge into the tibial and common fibular nerves.
The tibial nerve runs medially at the knee joint.
When the tibial nerve receives an action potential, the plantaris muscle contracts, providing weak plantar flexion of the foot and weak flexion of the knee .
Variation :-
The muscle may arise from the oblique popliteal ligament. Interdigitations with the lateral head of the gastrocnemius and a fibrous extension of the muscle to the patella are not unusual .
Function :-
The plantaris acts to weakly plantar flex the ankle joint and flex the knee joint.
The plantaris muscle may also provide proprioceptive feedback information to the central nervous system regarding the position of the foot.
The unusually high density of proprioceptive receptor end organs supports this notion .
Its motor function is so minimal that its long tendon can readily be harvested for reconstruction elsewhere with little functional deficit.
Often mistaken for a nerve by new medical students (and thus called the “freshman nerve”), the muscle was useful to other primates for grasping with their feet .
Clinical significance :-
A common injury that is normally attributed to the plantaris muscle is a condition called tennis leg.
Although pain in the calf can be attributed to a rupture of the plantaris muscle, recent ultrasound research has shown that tennis leg more commonly arises from tears in the musculotendinous junction of the medial gastrocnemius.
In one clinical study, 94 out of 141 patients (66.7%) diagnosed with tennis leg were found with a partial rupture of the gastrocnemius muscle, while rupture of the plantaris tendon was only seen in 2 patients (1.4%) .
Injury may occur from running, jumping, or pushing off one leg in sports such as tennis, basketball and soccer, which require quick foot movement in a certain direction.
Isolated plantaris muscle strains are rare, and ruptures normally occur in conjunction with injury to other muscles in the posterior compartment of the lower leg.
Symptoms of a plantaris muscle rupture may include an audible popping sound in the area during physical activity, swelling, pain in the back of the lower leg, and persistent soreness.
Ankle flexion may also be painful .
Deep Posterior Compartment :
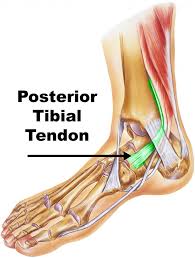
Tibialis posterior :
Introduction :-
The Tibialis Posterior is located in the deep compartment of the lower leg, and is a key stabilising muscle, supporting the medial arch of the foot.
The tibialis posterior is the most central of all the leg muscles, and is located in the deep posterior compartment of the leg.
It is the key stabilizing muscle of the lower leg.
Blood is supplied to the muscle by the posterior tibial artery, and innervation is via the tibial nerve.
Anatomy :-
Origin :-
Proximal postero-lateral aspect of the tibia.
Proximal postero-medial aspect of the fibula and the interosseous membrane
Mid portion: Situated in the deep posterior compartment of the lower leg and runs proximal to the medial malleoli where it is secured by the flexor retinaculum.
Insertion :-
The major insertion is onto the navicula and the plantar slip attatches to the medial cuniform
Nerve supply :-
Tibial Nerve (L4-S3)
Blood supply :-
Branches of the posterior tibial artery .
Artery :-
Tibial Artery
Structure :-
The tibialis posterior muscle originates on the inner posterior borders of the tibia and fibula.
It is also attached to the interosseous membrane, which attaches to the tibia and fibula.
The tendon of the tibialis posterior muscle (sometimes called the posterior tibial tendon) descends posterior to the medial malleolus and terminates by dividing into plantar, main, and recurrent components.
The main portion inserts into the tuberosity of the navicular and the plantar surface of the medial cuneiform.
The plantar portion inserts into the bases of the second, third and fourth metatarsals, the intermediate and lateral cuneiforms and the cuboid.
The recurrent portion inserts into the sustentaculum tali of the calcaneus.
Function :-
As well as being a key muscle and tendon for stabilization, the tibialis posterior also contracts to produce inversion and assists in the plantar flexion of the foot at the ankle.
The tibialis posterior has a major role in supporting the medial arch of the foot.
Dysfunction of the tibialis posterior, including rupture of the tibialis posterior tendon, can lead to flat feet in adults, as well as a valgus deformity due to unopposed eversion when inversion is lost.
Clinical relevance :-
Tibialis Posterior Rupture
Shin Splints
Posterior Tibial Tendon Dysfunction
Assessment :-
Resisted Muscle Test .
Palpation Assessment .
Treatment :-

Strengthening exercises for Tibialis Posterior .
Anterior Compartment (Dorsal flexors) :-
Tibialis anterior :
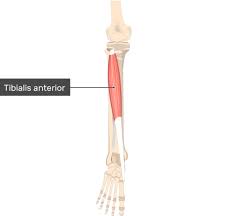
Introduction :
The Tibialis anterior (Tibialis anticus) is situated on the lateral side of the tibia; it is thick and fleshy above, tendinous below.
The fibers run vertically downward, and end in a tendon, which is apparent on the anterior surface of the muscle at the lower third of the leg.
This muscle overlaps the anterior tibial vessels and deep peroneal nerve in the upper part of the leg.
Variations.—A deep portion of the muscle is rarely inserted into the talus, or a tendinous slip may pass to the head of the first metatarsal bone or the base of the first phalanx of the great toe.
The Tibiofascialis anterior, a small muscle from the lower part of the tibia to the transverse or cruciate crural ligaments or deep fascia .
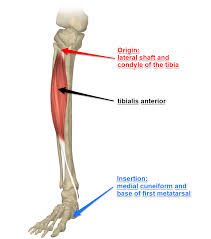
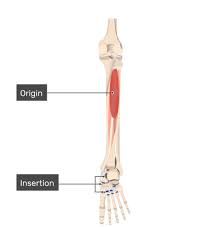
Origin :-
It arises from :-
Lateral condyle and upper half or two-thirds of the lateral surface of the body of the tibia
Adjoining part of the interosseous membrane
Deep surface of the fascia
Intermuscular septum between it and the Extensor digitorum longus.
Insertion :-
Medial and under surface of the first cuneiform bone, and the base of the first metatarsal bone .
Nerve supply :-
Deep Pereonal Nerve (L4, L5, S1)
Blood supply :-
Arterial supply of the tibialis anterior is rather complex .
The body of the muscle is entirely supplied by the branches of anterior tibial artery; anterior muscular, medial muscular branches and anterior tibial recurrent artery
The tendon is mainly supplied by the branches of anterior tibial artery but also by the branches of posterior tibial artery.
The former are the anterior medial malleolar artery and network, dorsalis pedis artery and medial tarsal arteries.
The latter are the medial malleolar and calcaneal arteries.
Artery :-
Anterior Tibial Artery
Structure :-
It arises from the lateral condyle and upper half or two-thirds of the lateral surface of the body of the tibia; from the adjoining part of the interosseous membrane; from the deep surface of the fascia; and from the intermuscular septum between it and the extensor digitorum longus.
The fibers of this circumpennate muscle are relatively parallel to the plane of insertion, ending in a tendon, apparent on the anteriomedial dorsal aspect of the foot close to the ankle.
After passing through the most medial compartments of the transverse and cruciate crural ligaments, it is inserted into the medial and under surface of the medial cuneiform bone and the base of the first metatarsal bone.
Nerve supply :-
Deep peroneal (fibular) nerve, branch of common peroneal (fibular) nerve (L4, L5, S1).
Variation :-
A deep portion of the muscle is rarely inserted into the talus, or a tendinous slip may pass to the head of the first metatarsal bone or the base of the first phalanx of the great toe.
The tibiofascialis anterior, a small muscle from the lower part of the tibia to the transverse or cruciate crural ligaments or deep fascia
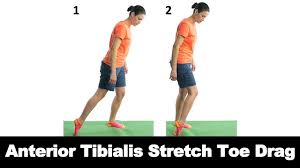
Function :-
Tibialis anterior is the primary dorsiflexor of the ankle with synergistic action of extensor hallicus longus, extensor digitorium longus and peroneous tertius.
Inversion of the foot.
Adduction of the foot.
Contributor of maintaining the medial arch of the foot .
At anticipatory postural adjustment (APA) phase during gait initiation tibialis anterior favour knee flexion at the stance limb by causing forward displacement of tibia .
Eccentric deceleration of foot plantarflexion, eversion and foot pronation.
Integrated Anatomy :-
Tibialis anterior is one of the muscles that tend to be inhibited and underactive this leads to overactive of synergistic muscles; extensor hallicus longus, extensor digitorium longus and peroneous tertius.
People with an inhibited or weak Tibialis anterior, for example those with hemiplegia or parkinson’s, will have an abnormality in their anticipatory postural adjustment (APA) phase during gait initiation of the affected limb.
They will try to compensate for the weakness of Tibialis anterior by overactivity of the contralateral tensor fascia latae (TFL)
Clinical Significance :-
Foot Drop :
Because the primary function of the tibialis anterior is dorsiflexion, paralysis of this muscle results in “foot drop,” or an inability to dorsiflex.
Paralysis can be caused by nerve injury, like direct damage to the deep peroneal nerve, or by a muscle disorder, like ALS.
“Foot drop” is often most obvious during gait when the patient cannot clear their foot during swing phase.
Tendinitis :-
The tibialis anterior tendon (TAT), like any tendon, can become irritated and inflamed—a condition known as tibialis anterior tendinitis.
Excessive tension on the tendon causes tendinitis, often due to repetitive, high-force activities, for example, hill running, or direct contact with equipment, like a shoe that is too tight around the ankle and the tendon.
Because the tendon traverses the anterior ankle and inserts on the medial foot, most patients will complain of pain at the front of the ankle or the medial midfoot.
Pain will be aggravated by the stressful activity and alleviated by rest.
Symptoms usually present gradually and get progressively worse.
On exam, the patient will have tenderness over the tendon and maybe even swelling.
Loading the tendon, as in dorsiflexion, will exacerbate the pain.
Treatment is conservative. Because the injury is due to exertion, the primary treatment is limiting activity.
NSAIDs can be used for analgesia.
It is also important to stretch the calf, decreasing the resistance to dorsiflexion.
A stabilizing or restricting ankle brace may also decrease the load through the tendon.
Tibial Stress Syndrome (Shin Splints) :-
The tibialis anterior muscle is often overused, resulting in a tibial stress syndrome that is more commonly known as shin splints.
Anterior tibial stress syndrome (ATSS) is acute and experienced by new runners or walkers; medial tibial stress syndrome (MTSS) is more chronic and occurs with athletes.
The tibialis anterior muscle is more commonly involved in the former while the tibialis posterior muscle is more commonly involved in the latter, though the tibialis anterior can also cause MTSS.
Both syndromes are caused by repetitive stress and strain on the tibia, often due to training errors or various biomechanical abnormalities.
Training errors include the recent onset of increased activity, intensity, or duration (doing “too much, too fast”) or running/walking on hard or uneven surfaces.
Biomechanical abnormalities include hyperpronation of the subtalar joint (eversion) and tibial torsion.
Tibial stress syndrome, particularly MTSS, can progress to a stress fracture of the tibia.
This is more common in females than in males due to a higher incidence of diminished bone density and osteoporosis.
In ATSS, the patient will present with tightness or tenderness in the anterior muscles of the leg that is aggravated by running or walking and alleviated with rest.
The pain may begin as a dull ache but often progresses to sharper pain. As the injury progresses, pain may be present even at rest.
Since tibial stress syndrome is a result of overuse and repetitive stress, the most important treatment in the acute phase is rest.
Ice and NSAIDs can provide analgesia. Long-term, it is critical to modify the training routine and add in stretching as well as strengthening exercises.
Stretching helps prevent muscle fatigue and subsequent strain on the tibia where muscles attach; strengthening muscles, like the tibialis anterior, helps control movement to reduce stress on the tibia.
It is also important to correct underlying biomechanical abnormalities.
Anterior Compartment Syndrome :-
Compartment syndrome occurs when tissue pressure within a closed, non-extensible muscle compartment exceeds the perfusion pressure.
Pressure greater than 30 mm Hg (in relaxed muscles, normal tissue pressure is 10 to 12 mm Hg) compromises circulation and can lead to necrosis and/or ischemia.
In acute compartment syndrome, the increased pressure is caused by bleeding or edema, usually due to fracture or trauma.
In chronic compartment syndrome (CCS), the increased pressure in skeletal muscle is due to overexertion.
Unlike other exertional injuries, like ATSS or MTSS, chronic compartment syndrome won’t respond to NSAIDs or physical therapy.
In the leg, the anterior compartment is most frequently affected by compartment syndrome.
Patients with compartment syndrome often present with ischemic pain, described as pain that is greater than one might expect given the clinical situation.
The pain can be reproduced by passively stretching the muscles in the affected compartment.
For example, in anterior compartment syndrome, plantar flexion will increase pain.
In CCS, like other exertional injuries, the pain is aggravated by activity and alleviated by rest.
Patients may also develop paresthesia due to nerve ischemia or paralysis of the affected muscles; however, neurological symptoms may also be due to a concurrent nerve injury.
Ischemia may also lead to pallor and pulselessness, though the latter may be a sign of arterial injury instead.
Finally, swelling is common and can make the leg feel firm and “wooden” upon palpation.
Early diagnosis of compartment syndrome is critical to avoiding poor outcomes, such as infection, contracture, and amputation.
Diagnosis requires awareness of the syndrome and appropriate examination.
Intra-compartmental pressure can also be measured to diagnose compartment syndrome.
Fasciotomy is the standard treatment; the recommendation is to decompress all four compartments.
Chronic compartment syndrome can be treated nonoperatively with complete cessation of all causative activities and massage therapy.
In general, nonoperative treatment is unsuccessful.
Assessment :-
Palpation :-
The client is supine. Place your resistance hand on the medial side of the distal foot.
Resist the client from dorsiflexing and inverting the foot. Look the distal tendon of the tibialis anterior on the medial side of the ankle joint and foot; it is usually visible.
Palpate the distal tendon by strumming perpendicular across it. Continue palpating the tibialis anterior proximally to lateral tibial condyle by strumming perpendicular to the fibers.
Once the tibialis anterior has been located, have the client relax it and palpate to asses its baseline tone .
Power :-
The action of the tibialis anterior muscle is considerably stronger than that of the other three dorsiflexor muscles of the foot .
Treatment :
Strengthening

Stretching

Dry Needling
Lateral Compartment (Evertors) :
Peroneus longus Muscle :
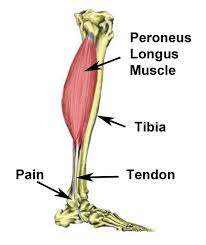
peroneus longus muscle
Introduction :
In human anatomy, the peroneus longus (also known as fibularis longus) is a superficial muscle in the lateral compartment of the leg, and acts to evert and plantarflex the ankle.
The muscle, the longest and most superficial of the three peroneus muscles, is attached proximally to the head of the fibula and its ‘belly’ runs down most of this bone.
It becomes a tendon that goes posteriorly around the lateral malleolus of the ankle, then continues under the foot to attach to the medial cuneiform and first metatarsal.
It is innervated by the Superficial peroneal nerve (L5,S1) .
Origin :-
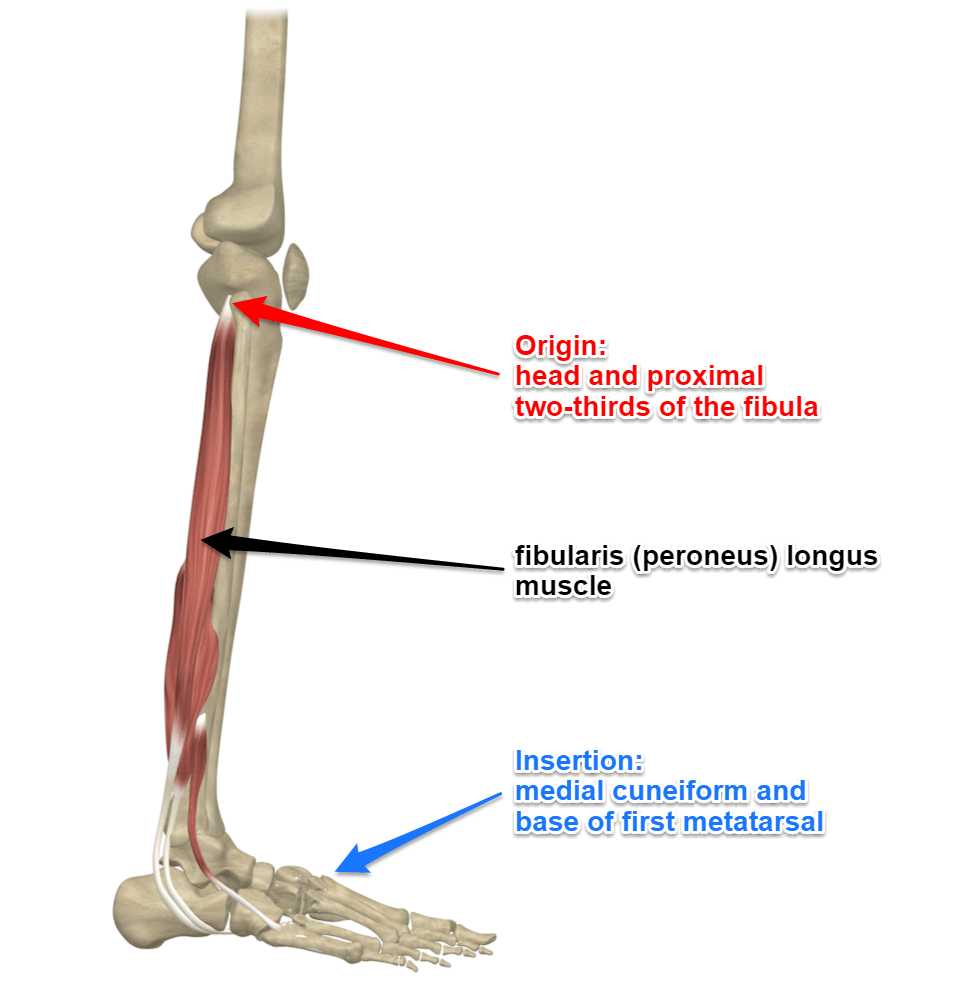
peroneus longus origin and insertion
Lateral condyle of tibia,
Head and proximal two-thirds of the lateral surface of fibula,
Intermuscular septa, and
Adjacent deep fascia .
Insertion :-
Lateral side of base of first metatarsal and of medial cuneiform bone.
Nerve :-
Superficial fibular (peroneal) nerve, L4,5,S1.
Blood Supply and Lymphatics :-
The anterior tibial artery and peroneal artery supply the peroneus longus muscle.
The anterior tibial artery arises from the popliteal artery, which originates from the superficial femoral artery, a branch of the common femoral artery off of the external iliac artery.
As the superficial femoral artery passes through the adductor hiatus into the popliteal fossa, it becomes the popliteal artery.
The popliteal artery then divides toward the distal end of the popliteal fossa to give rise to the anterior tibial artery and tibioperoneal trunk.
The tibioperoneal trunk then bifurcates into the posterior tibial and peroneal arteries.
The posterior tibial artery continues inferiorly to supply the posterior leg muscles, while the peroneal artery descends posteriorly to the fibula within the posterior compartment of the leg.
It then divides into perforating branches, which penetrate the intermuscular septum to supply the muscles of the lateral compartment of the leg .
The lymphatic vessels of the lower limb can subdivide into two major groups: superficial and deep vessels.
The superficial lymph vessels of the lower limb can further split into two groups: a medial group, which follows the greater saphenous vein, and a lateral group, which follows the small saphenous vein.
There are also deep lymph vessels including the anterior tibial, posterior tibial, and peroneal vessels that follow the course of the corresponding blood vessels.
The lymph vessels of the lower limb drain into the popliteal, superficial inguinal, deep inguinal, external iliac and lumbar or aortic lymph nodes .
Artery :-
Fibular (peroneal) artery.
Action :-
Talocrural joint: Foot plantar flexion;

Subtalar joint: Foot eversion;
Supports longitudinal and transverse arches o

Structure :-
It arises from the head and upper two-thirds of the lateral surface of the body of the fibula, from the deep surface of the fascia, and from the intermuscular septa between it and the muscles on the front and back of the leg; occasionally also by a few fibers from the lateral condyle of the tibia.
Between its attachments to the head and to the body of the fibula there is a gap through which the common peroneal nerve passes to the front of the leg .
It ends in a long tendon, which runs behind the lateral malleolus, in a groove common to it and the tendon of the peroneus brevis; the groove is converted into a canal by the superior peroneal retinaculum, and the tendons in it are contained in a common mucous sheath .
The tendon then extends obliquely forward across the lateral side of the foot, below the peroneal tubercle, and the tendon of the peroneus brevis, and under cover of the inferior peroneal retinaculum .
It crosses the lateral side of the cuboid, and then runs on the under surface of that bone in a groove which is converted into the peroneal canal by the long plantar ligament; the tendon then crosses the sole of the foot obliquely, and is inserted into the lateral side of the base of the first metatarsal bone and the lateral side of the medial cuneiform .
Occasionally it sends a slip to the base of the second metatarsal bone .
The tendon changes its direction at two points: first, behind the lateral malleolus; secondly, on the cuboid bone; in both of these situations the tendon is thickened, and, in the latter, a sesamoid fibrocartilage (sometimes a bone), is usually developed in its substance .
Function :-
Everts the foot, assists in plantar flexion and
In weight-bearing position depresses head of first metatarsal due to the strong pull on its insertion.
Maintains the transverse arch of the foot, due to how it crosses the sole of the foot.
Steadies the leg on the foot by drawing on the lateral leg, and stops it from collapsing medially.
Clinical relevance :-
Peroneal Tendinopathy
Peroneal tendon subluxation
Assessment :-
Peroneus longus and brevis tests
Weakness :-
The weakness of Peroneus lessens the ability to rise on the toes, decreases the lateral stability of the ankle and allows a varus position of the foot.
Length :-
Contracture results into an everted or valgus foot.
Associated Conditions :-
Injury to the peroneus longus muscle may cause pain in your lower leg, ankle, or foot.
Various conditions may affect the muscle and cause difficulty with walking or running.
Conditions that may affect the peroneus longus may include:3?
Peroneal tendonitis :-
This occurs when the long tendon of the peroneus muscle becomes inflamed and irritated.
This may occur due to overuse, or the peroneal tendon may be pinched beneath the bone that is courses under.
Pain on the outer portion of your foot and ankle may result making it difficult to walk or run normally.
Peroneus longus muscle strain :-
If a forceful movement of your foot or ankle occurs, your peroneal muscles may be overstretched, leading to a strain.
Strains may range in severity from a mild overstretch to a full-thickness tear of the peroneus muscle.
Peroneus longus strain may result in lateral leg pain, swelling near your ankle, and difficulty walking and running.
Peroneal tendon subluxation :-
If your foot is forcefully moved into dorsiflexion or inversion, the peroneal tendons may become overstretched and the retinaculum that holds them in place may become damaged.
This may result in tendon subluxation; the peroneus longus tendon moves out of place behind the lateral malleolus of your ankle and then snaps back into place.
This may or may not be accompanied by pain or discomfort.
Ankle sprain :-
The most typical motion of an ankle sprain is when your foot moves suddenly into inversion and your ankle rolls over laterally.
This may damage the lateral ligaments of your ankle and may overstretch your peroneal tendons.
The peroneus longus may become irritated as a result.
Weakness due to a pinched spinal nerve :-
The nerve that innervates your peroneus longus emerges from your low back, and a problem there from arthritis or a herniated disc may cause the nerve to become pinched.
This may result in pain in your lower leg and weakness in the muscles that move your ankle.
Sometimes, the tibialis anterior may be weakened as a result, leading to foot drop and difficulty moving your ankle normally.
Treatment :-
strengthening
dry needling
Rehabilitation :-
If you have a peroneus longus injury, you may benefit from working with a healthcare professional, such as a physical therapist (PT), to help you fully recover.
Various treatments for peroneus longus injuries may include:
Rest :-
Rest can be beneficial by allowing your peroneus longus tendon to heal properly.
Depending on the severity of your injury, rest may last from three days to several weeks. If the muscle or tendon are torn, you may be required to immobilize your ankle in a cast or removable walking boot.
Heat or Ice :-
If you have suffered an acute peroneal tendon injury, you may benefit from applying ice to the affected area to control inflammation.
Ice should be applied for 10 to 15 minutes several times each day. A few days after the injury, heat may be used to promote circulation.
Heat can be applied for 10 minutes. Care should be taken when using ice or heat to avoid skin irritation and burns.
Your PT can show you the best way to apply heat or ice.
Neuromuscular Electrical Stimulation (NMES) P :-
If you have peroneus longus weakness due to injury or from a pinched nerve, your PT may use neuromuscular electrical stimulation (NMES) to promote proper muscular function and contraction.
The NMES artificially contracts your muscle, helping it to function properly.
Low Back Exercises :-
If a pinched nerve is causing peroneus longus weakness or pain, performing lumbar stretching exercises may help get pressure off the nerve.
Prone press-ups, side glides, or lumbar flexion may benefit a pinched nerve. Which one is right for you? Your local PT can help you decide.
Stretching Exercises :-
After a peroneus longus injury, your healthcare provider may prescribe stretching exercises for your ankle and lower leg.
The runner’s stretch may be used to stretch your calf and soleus muscles, and ankle alphabet exercises where you draw letters with your ankle can help improve ankle range of motion.
The peroneus longus muscles are stretched by inverting (turning inwards) your ankle.
Using your hands, turn your foot inwards so the sole of your foot is facing inwards.
Hold the stretched position for 15 seconds and then rest. This can be repeated three to five times.
Strengthening Exercises :-
If your peroneus longus is weak, strengthening exercises may be performed.
To do this, simply move your foot outwards into eversion. Hold the position for 5 seconds, and then rest. Repeat 10 to 15 times.
You can also use a resistance band to strengthen your peroneus longus.
First, tie your resistance band to a sturdy object, such as a sofa leg. Next, place your foot in the loop, rotate your ankle outwards, stretching the band using only your foot.
Hold for two to three seconds and then rest. Repeat 10 to 15 times.
Since the peroneus longus also functions to point your toes, performing calf raises can also help strengthen the muscle.
Simply stand with the balls of your feet on the edge of a step and rise up onto your toes.
Hold the position for a few seconds, and then slowly lower yourself down. Perform 10 to 15 repetitions.
Balance and Proprioception Exercises :-
Since the peroneus longus helps to stabilize your ankle and foot when walking, it may be helpful to work on improving balance and proprioception as part of your peroneus rehab program.
A simple progression of single-leg standing may be prescribed. To start, hold onto something stable and stand on one foot.
If you can hold this for 30 seconds, perform the exercise without holding on. When this becomes easy, perform the exercise while holding something stable, but keep your eyes closed while balancing.
Finally, stand on one foot with no upper extremity support and keeping your eyes closed.
To make the single-leg standing exercise more challenging, stand upon something unstable such as a couch cushion or a pillow.
Massage :-
After a peroneus longus injury or with tendonitis, massages can promote circulation and decrease muscle pain.
Massage can also help to improve tissue mobility of the muscle and may be used prior to stretching.
Massaging the peroneal muscles should not be painful; gentle strokes of progressive intensity is enough to promote movement and circulation in your peroneus longus.
Shoe Orthotics or Inserts :-
Sometimes, poor foot position can place excessive stress on your peroneus longus muscle, leading to pain and difficulty walking.
Your physician may recommend using inserts in your shoes to help support the arch of your foot.
This may give your peroneus longus some help keeping your foot in the right position and may decrease pain.
Injections :-
If you have persistent peroneus longus pain due to inflammation, you may benefit from a steroid injection.
The steroid is a powerful anti-inflammatory medication that can reduce tendon pain and swelling.
A newer procedure called platelet-rich plasma (PRP) injection may also be helpful in relieving peroneus longus pain.
During PRP, blood is drawn from your body and is spun in a centrifuge to obtain the platelets and plasma.
Then, the platelets are mixed with a small amount of plasma and are injected into your tendon.
This signals your body’s immune system to release white blood cells and growth factors to begin healing the injured tendon.
PRP injections are touted as helping your body heal itself.
Research continues to be done on PRP therapy and its efficacy in the treatment of tendon injuries.
Lateral Compartment (Evertors) :
Peroneus brevis Muscle :
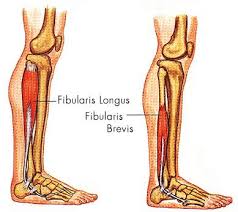
peroneus brevis muscle
Introduction :-
peroneus brevis muscle
The Peroneus Brevis (also known as Fibularis Brevis) is a short muscle that lies at the lateral part of the lower leg deep to the Peroneus Longus . It is one of the three peroneus muscles .
Origin :-
Distal two-thirds of lateral fibula , its tendon pass downwards and loops posterior to the lateral malleolus .
Insertion :-
Base of the fifth metatarsal .
Nerve :-
Superficial peroneal nerve .
Innervation :-
Superficial peroneal nerve (L5, S1, S2)
Blood Supply and Lymphatics :-
The peroneal artery arises from the tibial-peroneal truck distal to the popliteal artery.
The peroneal artery is also called the fibular artery. The peroneal artery is the blood supply to the lateral compartment of the leg.
Muscular branches of the peroneal artery supply the peroneus brevis muscle .
Venous drainage is by superficial veins that drain into the small saphenous vein and by deep veins that drain into the posterior tibial vein.
The bilateral peroneal brevis muscles and lateral compartments lymphatics first drain to the popliteal and inguinal nodes and subsequently to the external iliac nodes.
The external iliac nodes then drain into lumbar (aortic) nodes .
Artery :-
Muscular branches of the peroneal artery .
Action :-
everts foot and weakly plantarflexes it
provides support for the lateral longitudinal arch
Structure and Function :-
The peroneus brevis muscle, also referred to as the fibularis brevis muscle, is located in the lateral compartment of the lower extremity below the knee, underneath the peroneus longus muscle.
It is a small, relatively short muscle of the leg that originates from the lower two-thirds of the lateral surface of the fibula bone.
Its muscle fibers traverse downwards and form into a tendon which runs just posterior to the lateral malleolus, crossing the ankle, and inserting on the styloid process of the proximal the fifth metatarsal bone .
The ankle joint is a relatively mobile joint that relies on its surrounding ligaments for stability.
The structural ligaments of the ankle connect bones to bones and are deep to the muscles and tendons of the ankle and lower extremity.
Muscles that cross the ankle joint have a mechanical action on the foot and ankle.
The primary movements of the foot and ankle are plantar flexion, dorsiflexion, eversion, and inversion.
The peroneal brevis muscle and tendon cross the ankle joint posterior to the fibula.
The peroneus brevis muscle assists with eversion of the foot, and to a weaker extent, plantarflexes the ankle .
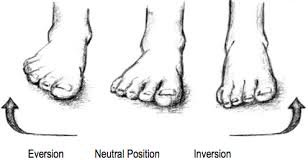
Foot eversion is tilting of the sole of the foot away from the midline, and foot inversion is the tilting of the sole towards the midline.
Foot eversion requires a muscle to have an insertion on the lateral aspect of the foot, such as with peroneus brevis which inserts on the lateral foot at the proximal fifth metatarsal.
Plantar flexion describes the movement of the foot down towards the sole of the foot and dorsiflexion is the action of foot upward towards the shin.
Plantar flexion requires the muscle to have an insertion relatively close to the ankle, such as with peroneus brevis which inserts on the proximal fifth metatarsal.
The ankle joint serves as the fulcrum for both eversion and plantar-flexion .
Foot eversion and assists in plantar flexion .
Clinical relevance :-
Peroneal tendinopathy
Avulsion fracture of the ankle
Peroneal tendon sublaxation
Jones Fracture
Clinical Significance :-
Ankle and foot injuries are common in the occupational setting.
Being aware of a few of the common pathologies associated with the peroneal brevis muscle and tendon is helpful in making a diagnosis in cases of ankle and foot injury.
The most common injuries to the peroneal brevis muscle are to its tendon in the form of tendon sprain, dislocation, or splitting.
The tendinous insertion of peroneus brevis can be injured following an inversion or supination injury resulting in a tendon sprain.
During an ankle sprain the peroneus brevis can be torn presenting as persistent swelling along the lateral aspect of the ankle at the peroneal tendon sheath.
Supination-adduction (SAD) injuries to the ankle often involve damage to the lateral ligaments of the ankle, fracture of the distal fibula, and possibly an injury to the peroneal tendons and peroneal retinacula.
Occasionally, the base of the fifth metatarsal is also fractured in a lateral ankle sprain and the peroneal brevis tendon may pull on and detach the bone at the metaphyseal-diaphyseal junction, which is called a Jones fracture.
This can occur as either an avulsion or oblique/spiral type fracture.
Additionally, a strike to the lateral aspect of the foot can result in laceration of the peroneal brevis tendon.
There is a groove in the posterior aspect of the distal fibula is where the tendon of the peroneal brevis muscle sits with the tendon of peroneal longus behind it.
The groove is variable depth and may be shallow, which is the reason that the peroneal tendons are the most commonly dislocated tendons in the ankle.
Another cause for tendon dislocation is the peroneus brevis tendon rubbing on fibula and causing an inflammatory periosteal reaction and bony proliferation which can cause chronic subluxation or displacement of the peroneal tendons.
A longitudinal (vertically oriented) split of the peroneus tendon can also occur with subluxation.
A low-lying or inferiorly positioned peroneus brevis muscle belly can cause tendon problems and lead to instability, dislocation, tendonitis, or tendon tears as well .
Assessment :-
Peroneus longus and brevis tests
cause :-
Weak or loose ligament that covers the tendons can allow the tendons to dislocate.
A shallow groove in the fibula may not allow the tendons to seat properly.
Twisting injury to the ankle that causes the tendons to over contract and tear the ligament that covers it.
Twisting injury to the ankle may cause a severe contraction causing a fracture off of the fibula, allowing the tendons to dislocate.
Anomalous muscle in the outer part of the ankle.
Hypertrophy of a normal muscle causing too much bulk on the outside of the ankle.
Weak or loose ligament that covers the tendons can allow the tendons to dislocate.
A shallow groove in the fibula may not allow the tendons to seat properly.
Twisting injury to the ankle that causes the tendons to over contract and tear the ligament that covers it.
Twisting injury to the ankle may cause a severe contraction causing a fracture off of the fibula, allowing the tendons to dislocate.
Anomalous muscle in the outer part of the ankle.
Hypertrophy of a normal muscle causing too much bulk on the outside of the ankle.
Sign and symptoms :-
Swelling behind the fibula on the outside of the ankle.
Popping sensation with movement of the foot down and in and up and out.
Appearance of the tendons in the front part of the ankle instead of in their normal position behind the fibula where they are not visible.
Weakness with activity.
Frequent ankle sprains.
Often associated with a tear of the peroneus brevis tendon.
May be associated with ankle ligament injury and chronic instability of the ligaments in the ankle.
Treatment :-
Everts foot
plantar flexes ankle
Deep Posterior Compartment :
Flexor hallucis longus :

flexorhallucislongus
Introdution :-
Flexor hallucis longus is a powerful muscle located on the posterior aspect of the fibular below the deep fascia of the calf.
In its own synovial sheath, the tendon passes downwards, deep to the flexor retinaculum, crossing the posterior ankle joint, lateral to flexor digitorum longus.
The tendon wraps around the lower end of the of the tibia, the back of the talus, and the inferior surface of the sustentaculum tali, where its passes through a fibrous, synovial-lined tunnel.
As the tendon enters into the sole of the foot it lies superficial to the spring ligament passing forward deep to the tendon of flexor digitorum longus.
It then enters the fibrous sheath of the great toe passing between the two sesamoid bones to insert at the base of the distal phalanx .
Origin :-
Lower two-thirds of posterior fibula.
Insertion :-
Plantar surface at the base of the first distal phalanx.
Nerve :-
Branch of the tibial nerve (root S1 and S2).
Cutaneous supply from root S2.
Artery :-
Peroneal artery
Blood supply :-
Flexor digitorum longus receives arterial supply from the branches of the posterior tibial and fibular arteries . Venous drainage is of this muscle is provided by the peroneal vein, a tributary of the popliteal vein.
Innervation :-
Tibial nerve (S2, S3)
Structure :-
The flexor hallucis longus is situated on the fibular side of the leg.
It arises from the inferior two-thirds of the posterior surface of the body of the fibula, with the exception of 2.5 cm. at its lowest part; from the lower part of the interosseous membrane; from an intermuscular septum between it and the peronius muscles, laterally, and from the fascia covering the tibialis posterior, medially.
The fibers pass obliquely downward and backward, where it passes through the tarsal tunnel on the medial side of the foot and end in a tendon which occupies nearly the whole length of the posterior surface of the muscle.
This tendon lies in a groove which crosses the posterior surface of the lower end of the tibia, between the medial and lateral tubercles of the posterior surface of the talus, and the under surface of the sustentaculum tali of the calcaneus; in the sole of the foot it runs forward between the two heads of the flexor hallucis brevis, and is inserted into the base of the last phalanx of the great toe.
The grooves on the talus and calcaneus, which contain the tendon of the muscle, are converted by tendinous fibers into distinct canals, lined by a mucous sheath.
As the tendon passes forward in the sole of the foot, it is situated above, and crosses from the lateral to the medial side of the tendon of the flexor digitorum longus, to which it is connected by a fibrous slip.
Variation :-
Usually a slip runs to the flexor digitorum and frequently an additional slip runs from the flexor digitorum to the flexor hallucis.
Peroneocalcaneus internus, rare,[clarification needed] arises below or outside the flexor hallucis from the back of the fibula, passes over the sustentaculum tali with the flexor hallucis and inserts into the calcaneum.
Function :-
Flexes all the joints of the great toe as the foot is raised from the ground. Additionally stabilises the first metatarsal head and keeps distal pad of the great toe in contact with ground in toe-off and when on tip-toe.
Aids in plantarflexion at the ankle joint .