Neurological Rehabilitation
What is neurological rehabilitation?
According to the World Health Organization (WHO) definition provided in 2011, rehabilitation refers to a set of measures aimed at assisting individuals who have or are likely to have a disability in achieving and maintaining optimal functioning in their interaction with the environment. Based on this definition, neurological rehabilitation specifically focuses on helping patients with neurological conditions recover or improve their functionality within their environment.
The significance of neurological rehabilitation lies in its ability to enhance independence, elevate the quality of life, and effectively manage symptoms associated with neurological disorders. These rehabilitation programs are tailored to meet the individual needs of patients and may vary depending on the specific areas affected by their condition.
Neurological rehabilitation is a wide program led by physicians and developed especially for people with neurological diseases, trauma, and disorders. By engaging in neurological rehabilitation, patients often experience improvements in their overall functioning, a reduction in symptoms, and an enhanced sense of well-being. It is important to emphasize that neurological rehabilitation is highly individualized, as each patient’s condition and requirements are unique. Therefore, a thorough assessment and personalized approach are crucial in determining the most appropriate and effective course of treatment.
Principles of neurological rehabilitation
Neurological rehabilitation is founded on a range of principles that guide the treatments provided. These principles include:
- Neuroplasticity: Recognizing the brain’s dynamic nature and its capacity to adapt and change following brain or spinal cord injury.
- Individualized approach: Employing a problem-solving and eclectic approach to tailor treatments according to the patient’s specific symptoms and the extent of their injury.
- Maximizing movement: Encouraging and enhancing any existing movement capabilities through techniques such as strengthening exercises, sensory stimulation, positive reinforcement, and verbal feedback.
- Promotion of normal movement and function: Focusing on restoring and improving movement patterns and functional abilities that align with normal daily activities.
- Correcting and varying positions: Addressing and modifying the patient’s positioning and posture while lying, sitting, and standing to optimize functional outcomes.
- Task-oriented activities: Emphasizing functional activities that replicate daily tasks, allowing patients to practice and regain skills relevant to their everyday lives.
- Cognitive engagement: Utilizing verbal and visual prompts to stimulate patients’ cognitive processes, encouraging active thinking and learning during treatment.
- Prevention of muscle shortening: Addressing muscle tightness and contractures to prevent the development of spasticity and abnormal movement.
- Interdisciplinary teamwork: Adopting a team-based approach to rehabilitation, involving professionals from various disciplines to provide comprehensive care and support.
- Goal-oriented treatment: Establishing realistic, measurable goals within specific timeframes to guide the rehabilitation process and track progress.
- Patient engagement and empowerment: Actively involving patients in their treatment sessions, promoting their active participation, and striving to achieve the highest possible degree of independence and quality of life.
By adhering to these principles, neurological rehabilitation aims to optimize recovery, enhance functional abilities, and improve the overall well-being of patients.
Goals of Neurological Rehabilitation
Preventing complications:
Neurological conditions can give rise to various complications if left unaddressed. These complications can worsen the underlying conditions and, in some cases, pose life-threatening risks. Additionally, secondary complications can hinder the recovery process and limit the effectiveness of rehabilitation. By participating in rehabilitation programs, individuals can proactively prevent these complications, and healthcare specialists can identify and address potential issues before they escalate.
Teaching adaptive strategies:
A primary objective of rehabilitation is to educate patients on how to function and carry out daily activities despite their neurological condition. Physical therapists assess the patient’s impairments and devise personalized plans to enhance their ability to function in their usual environment. These strategies can help reduce disability and enable patients to adapt and cope with their condition more effectively.
Facilitating function in a normal environment:
In certain cases, patients may not be able to regain their pre-existing level of functioning, necessitating support from family caregivers and community-based service providers upon discharge from the hospital. Rehabilitation plays a crucial role in teaching patients and their caregivers how to navigate and adapt to these changes. Adjusting to new circumstances can require significant mental and physical energy, and rehabilitation provides guidance and support in this process.
In general, neurological rehabilitation programs aim to help patients:
- Develop the necessary skills to perform daily activities and lead a more independent life.
- Manage stress, anxiety, and depression associated with their condition.
- Receive training in bladder and bowel control.
- Engage in support groups to connect with others facing similar challenges.
- Learn to use assistive devices that promote self-dependency.
- Acquire knowledge of safety measures to prevent accidents or injuries.
- Gain understanding and proficiency in managing their home care requirements.
- Address pain management and receive nutritional and vocational counseling as part of their rehabilitation journey.
What Does a Neurological Rehabilitation Program Consist Of?
Neurorehabilitation programs are comprehensive and encompass a range of activities tailored to each patient’s specific condition. These programs aim to enhance recovery and functional abilities. Here are some common activities included in neurological rehabilitation programs:
- Assistance with Activities of Daily Living (ADLs): This involves helping patients with tasks like eating, housekeeping, bathing, writing, cooking, and dressing, promoting independence and improving functional abilities.
- Stress and Depression Management Techniques: Neurorehabilitation programs often incorporate strategies to manage stress and address depression, as emotional well-being plays a crucial role in the recovery process.
- Pain Management: Patients may receive therapies and techniques to manage and alleviate pain associated with their neurological condition, enhancing their comfort and quality of life.
- Speech Therapy: Speech therapy focuses on improving communication skills, reading, writing, and swallowing abilities for patients experiencing speech and language difficulties due to their neurological condition.
- Assistive Mobility Devices: Rehabilitation professionals assist patients in obtaining and utilizing assistive mobility devices, such as wheelchairs or walkers, to promote independence and mobility.
- Bladder and Bowel Control Retraining: Patients with neurological conditions that affect bladder and bowel function may receive training to regain control and improve the management of these functions.
- Nutritional Management and Counseling: Nutritional management is essential in promoting overall health and recovery. Patients may receive dietary counseling and guidance to ensure proper nutrition.
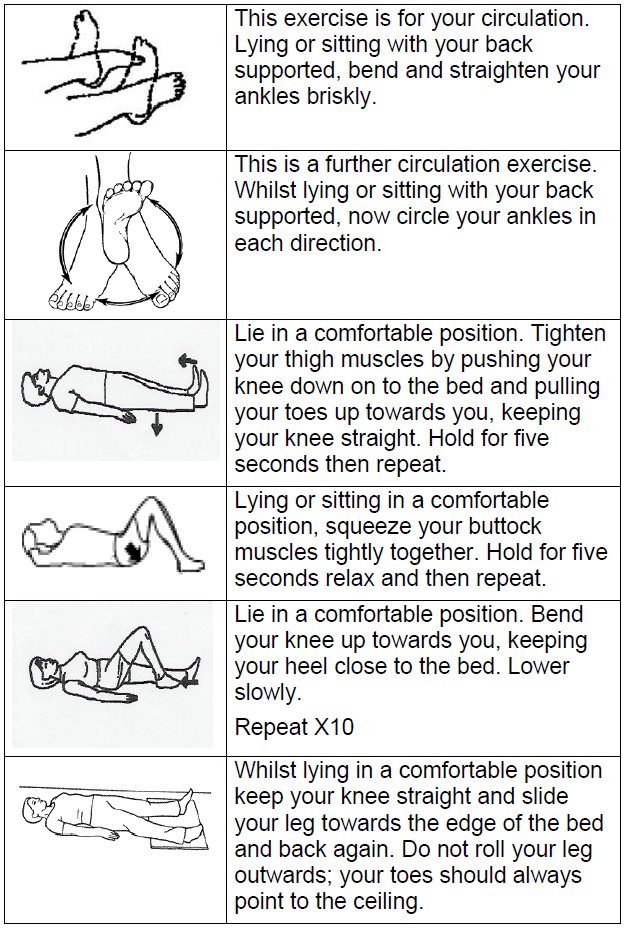
- Mobility Activities: These activities focus on enhancing muscle control, managing spasticity, gait training, range of motion exercises, and improving balance, and coordination, which are crucial for physical functioning.
- Cognitive Improvement Activities: Cognitive exercises and interventions target cognitive difficulties such as concentration, attention, memory, and problem-solving to improve overall cognitive function and enhance daily functioning.
- Social and Behavioral Skills Retraining: Patients may participate in activities that help improve social skills, promote behavior management, and enhance social interactions to reintegrate into their communities.
- Patient and Caregiver Education and Counseling: Education and counseling sessions provide information and support to both patients and their caregivers, equipping them with knowledge and resources to navigate the challenges of their condition effectively.
- Participation in Community Support Activities: Engaging patients in community support activities helps foster social connections, build confidence, and provide opportunities for integration and active participation in society.
- Vocational Counseling: For individuals seeking to return to work or explore vocational options, vocational counseling can provide guidance, skills training, and assistance in identifying suitable employment opportunities.
What does a Neurological Rehabilitation Team consist of?
For prosperous results, neurological rehabilitation teams use a multidisciplinary procedure involving different professionals. It’s important to note that the rehabilitation team provides specialized therapy distinct from the patient’s primary care team. Neurorehabilitation teams may consist of the following specialists:
- Neurologists: Experts in diagnosing and treating neurological conditions, they oversee the overall neurological care of the patient.
- Orthopedist: Specializes in managing musculoskeletal conditions or injuries that may impact the rehabilitation process.
- Physiatrist: A physician specializing in physical medicine and rehabilitation, lead the rehabilitation team and coordinate the overall care plan.
- Internist: Provides general medical care, managing any underlying medical conditions that may affect rehabilitation.
- Rehabilitation Nurse: Plays a crucial role in providing nursing care, managing medications, and monitoring the patient’s health during rehabilitation.
- Dietitian: Offers nutritional guidance tailored to the specific needs of patients with neurological conditions.
- Physical Therapist: Focuses on improving mobility, addressing a range of motion, balance, pain management, gait impairments, and coordination.
- Occupational Therapist: Assists patients in regaining or enhancing their ability to independently perform daily activities, such as dressing, eating, and bathing.
- Speech Therapist: Works with patients experiencing speech or swallowing difficulties due to neurological conditions, helping them recover or improve these functions.
- Social Worker: Provides support, counseling, and assistance with the psychosocial aspects of rehabilitation, including coordinating community resources and addressing emotional well-being.
- Psychiatrist: Evaluates and addresses the psychological and emotional aspects of the patient’s rehabilitation, providing therapy, counseling, and support.
- Recreational Therapist: Designs and implements recreational activities to enhance the patient’s physical, emotional, and social well-being during rehabilitation.
- Case Manager: Coordinates and oversees the patient’s overall care plan, ensuring continuity and effective communication among the different specialists.
- Audiologist: Specializes in evaluating and managing hearing and balance disorders that may impact the patient’s rehabilitation process.
- Chaplain: Provides spiritual support and guidance to patients and their families during the rehabilitation journey.
- Vocational Counselor: Assists patients in exploring vocational options, job placement, and strategies for reintegrating into the workforce post-rehabilitation.
- Neuropsychologists: Specializes in addressing cognitive and behavioral issues resulting from brain injuries, strokes, or other neurological conditions. They provide cognitive therapy and help patients adapt to physical changes.
The collaboration of these diverse specialists within a neurological rehabilitation team ensures comprehensive care that addresses the various facets of the patient’s condition, maximizing the chances of successful rehabilitation outcomes.
Neurological Rehabilitation Supporting Specialisations
Neurological rehabilitation is a collaborative effort, bringing together experts from various fields such as doctors, bioengineers, social workers, computer scientists, and therapists. Each neuro program is carefully designed through thorough planning and evaluation to meet the specific needs of the individual patient.
Neurorehabilitation is supported by several specialized areas, including:
Physiotherapy: The primary goal of physiotherapy is to assist patients in overcoming physical limitations resulting from neurological disorders or trauma. Through consistent physiotherapy, individuals can regain the ability to perform daily activities, pursue hobbies and sports, improve functionality, and restore confidence in leading a near-normal life.
This therapeutic choice deals with comprehensive exercise to correct several problems induced by nerve damage, For example:
- Cardiovascular endurance
- Decreased spasticity
- Prostheses or Orthoses
- Gait training
- Postural realignment
- Balance re-training
- Core Alignment
- Visual-perceptual skill training
- Cardiovascular endurance
- Exercise to operate tools such as wheelchairs, crutches, and walkers.
Occupational therapy: Occupational therapy employs therapeutic strategies to help patients reintegrate into their daily activities, known as Activities of Daily Living (ADL). These may include addressing challenges related to dysphagia or self-feeding, simplifying work tasks, simulating driving scenarios, and managing spasticity.
Speech and language therapy: Speech and language therapy focuses on assisting patients in overcoming speech impairments caused by severe strokes, brain injuries, or other neurological conditions. This therapy also helps individuals regain the ability to eat and swallow, particularly when muscle weakness in the throat is present.
Recreational therapy: Recreational therapy utilizes tailored recreational activities to aid patients in rebuilding skills, enhancing mood, fostering social connections, and improving the overall quality of life during rehabilitation.
By bringing together these different therapeutic approaches and involving a multidisciplinary team of experts, neurological rehabilitation programs can provide comprehensive and personalized care to optimize the recovery and well-being of patients.
Approaches to Neurological Rehabilitation
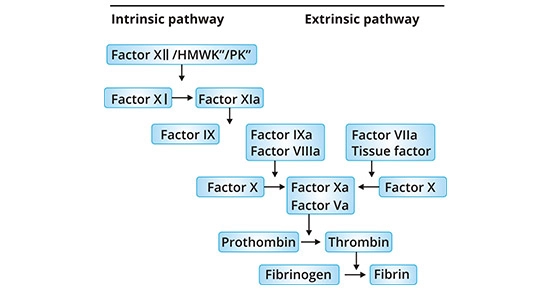
Neurological rehabilitation encompasses a variety of techniques aimed at promoting recovery and improving functionality. Some of these techniques include:
Bobath approach: Also known as neuro-developmental treatment (NDT), this technique focuses on practicing movement patterns under the guidance of a physical therapist. Motor learning principles are applied, and movements are repeated until each component is mastered. Emerging techniques, such as the use of robotic exoskeletons, can provide high repetitions of movement, enhancing balance and stability.
Brunnstrom approach: This popular movement therapy approach utilizes synergistic patterns of muscular movements to promote functional recovery.
Carr and Shepherd’s approach: This method emphasizes functional movements and involves the repeated and correct practice of specific movements until the desired outcome is achieved.
Gait re-education: Many patients experience difficulties with walking after an injury, making gait rehabilitation crucial. Physical therapists identify and correct any abnormalities in walking patterns. Emerging techniques, such as exoskeletons, can automatically train gait, allowing for increased training intensity without additional therapy time.
Transfer rehabilitation: This technique focuses on teaching patients the skills needed to perform transfers, such as moving from the bed to a chair. Patients practice these movements until they can perform them confidently.
Mobility rehabilitation: A significant aspect of rehabilitation programs, mobility rehabilitation aims to help patients regain independent and safe mobility. It includes exercises such as balance exercises, range of motion exercises, and stretches, all intended to improve a patient’s mobility skills.
Contracture management: Patients often experience muscle tightness, and managing contractures is important for proper recovery. Strategies such as splinting, weight-bearing, and casting may be employed to release muscle tension in the lower limbs.
Equipment and adaptations assessment: After an injury, the use of assistive mobility devices like wheelchairs and walkers may be recommended to enhance independence. Physical therapists play a key role in assessing and recommending appropriate equipment and adaptations during the rehabilitation process.
How Does Neurorehabilitation Work?
Rehabilitation, in general, is fundamentally based on the concept of “neuroplasticity,” which refers to the brain’s ability to adapt and reorganize its activity in response to internal and external stimuli. Neuroplasticity encompasses structural and functional changes as well as alterations in neural connections. It enables the brain to learn new information and adjust to different circumstances, particularly following injuries such as stroke or traumatic brain injury (TBI). The brain is not fixed; it undergoes continuous changes with each experience and input, forming new connections as we learn and adapt. This inherent quality of learning and relearning forms the foundation of rehabilitation.
The primary objective of every neurorehabilitation program is to maximize health, independence, and functionality by employing effective rehabilitation strategies. Although the approach may vary for each patient, the general process follows a similar pattern. The initial step of every program involves a comprehensive assessment utilizing specific tests to evaluate the extent of the injury and the patient’s abilities. These assessment results are then used to formulate a personalized treatment plan and establish realistic rehabilitation goals. Once the assessment phase is completed, the rehabilitation process commences and continues until the desired outcomes are achieved.
When does neurological rehabilitation require?
The answer is quite straightforward. The nervous system is responsible for regulating all our bodily functions, from basic activities like breathing and muscle control to sensations of heat, cold, pain, and pleasure.
Any damage to this intricate system can affect the nerves and disrupt these vital functions. Moreover, nerve damage can also occur as a result of chronic conditions such as Parkinson’s, Alzheimer’s, cancer, diabetes, dementia, motor neuron diseases, and autoimmune disorders.
Certain symptoms and signs suggest the necessity for neurological rehabilitation, also after the initial stages of medical therapy:
- Imbalance
- Dizziness
- Difficulty walking without assistance
- Inability to engage in regular activities
Neurological rehabilitation is designed to help patients recover from the consequences of trauma (such as accidents or falls) or diseases. It provides avenues to overcome physiological and psychological barriers and discover new ways to enhance one’s lifestyle.
Nerve damage can lead to varying degrees of after-effects, but the encouraging news is that neurological rehabilitation offers the best solution for many neurological conditions.
What are the Phases of Neurological Rehabilitation?
The method of neurological rehabilitation contains various phases, relying on the severity of the damage and the individual’s symptoms. Each phase is assessed using the Barthel Index, which measures performance in activities of daily living. The treatment a patient receives is determined by the phase they are in within the rehabilitation process.
Long-Term Acute Care Hospital (LTACH):
This initial level of critical care follows inpatient hospital stays. Patients in this phase require intensive clinician supervision and management, including ventilator management, tracheostomy care, and wound infection care.
Acute Rehabilitation:
During this phase, patients engage in three hours of skilled therapy per day, including physical therapy (PT), occupational therapy (OT), and speech and language therapy. This phase distinguishes itself from subacute rehabilitation through its intensive therapy demands. Typically, patients have shorter stays as they transition to home therapy or subacute rehabilitation.
Subacute Rehabilitation in Skilled Nursing Facilities:
Patients in this stage are stable but not yet independent enough to return home. They undergo therapy, although the demands are less rigorous compared to acute rehabilitation. There is less supervision in this phase, with fewer nurses assigned to multiple patients.
Long-Term Care Facility or Nursing Home:
This setting is for patients who require additional care beyond what can be provided at home. They need more supervision and assistance with activities of daily living, such as eating, bathing, and dressing. While not requiring extensive medical care, they may depend on nurses for medication management.
Home with Services:
Patients in this phase have higher functional ability and greater independence compared to the previous stages. They receive support services while residing in their own homes.
Each phase of neurological rehabilitation is tailored to the individual’s needs, ensuring comprehensive care and striving to maximize functional independence and quality of life.
Benefits of Neurological Rehabilitation
Neurological rehabilitation should be initiated promptly following an injury to optimize the chances of a successful recovery.
Neurorehabilitation combines various principles of neurological physiotherapy to provide the most effective treatment for patients. These principles include the Bobath Concept (focusing on normal movement), the Carr and Shepherd Concept (emphasizing motor relearning), the Brunnstrom Approach (targeting synergistic movement), Conductive Education, and functional rehabilitation. The specific treatment approach employed is tailored to the individual’s symptoms, needs, and goals, enabling the maximization of their potential.
After an injury, muscle strength and movement can be adversely affected. Muscles may weaken or become tight, leading to spasms. The sensation may also be altered, and difficulties with speech and swallowing can arise.
Neurological rehabilitation offers several significant benefits:
- Improved Quality of Life: Whether resulting from accidents, falls, or diseases, neurological conditions can profoundly alter a person’s life. The primary objective of rehabilitation is to enhance the quality of life for individuals facing these challenges, whether the effects are permanent or temporary. There is ample evidence indicating that early intervention can slow down the degenerative process. Rehabilitation also increases the likelihood of reversing reversible functions and preserving existing abilities.
- Individualized Approach: As mentioned earlier, there is no standardized protocol for neurological rehabilitation. Ideally, rehabilitation should commence immediately after the injury and continue without interruptions. This personalized approach takes into account the patient’s specific physiological limitations and requirements, promoting optimal outcomes.
- Cost–Effectiveness: Consistent rehabilitation helps patients regain a sense of normalcy and equips them with the skills needed for independence, reducing reliance on hospitals, medications, and costly medical services. This contributes to overall cost savings.
- Comprehensive Multidisciplinary Care: Neuro-rehabilitation often involves a multidisciplinary team working in coordination to achieve the best possible results. This collaborative approach typically takes place in an acute rehabilitation hospital. The treatment plan is continuously reviewed and adjusted based on the patient’s progress. This holistic approach fosters long-term self-dependence and confidence.
Physiotherapy treatment plays a crucial role in neurological rehabilitation, providing the following benefits:
- Facilitating precise and goal-directed movements
- Retraining normal movement patterns
- Enhancing functional abilities for everyday activities
- Increasing muscle strength
- Improving range of motion
- Enhancing gross and fine motor skills
- Improving posture and balance
- Reducing spasticity and preventing contractures by lengthening tight muscles
- Enhancing fitness levels and endurance
- Addressing respiratory issues and reducing the risk of chest infections
- Reducing the risk of falls
- Alleviating stress and anxiety
- Relieving pain
- Promoting independence
- Maximizing the individual’s potential for recovery.
Conditions That Can Benefit From Neurological Rehabilitation
Neurological physiotherapy is recommended by physicians for various conditions that affect the nervous system. While each condition has unique effects on the nervous system, they often share similar impairments. Patients who experience poor balance and coordination, gait issues, vision changes, and difficulties with walking and self-care can benefit from neurological physiotherapy.
Here are some examples of the conditions managed with neurological physiotherapy:
Microcephaly: A rare neurological condition where an infant’s head is smaller than average due to abnormal brain growth. It can be present at birth or develop in infancy, often leading to learning disabilities and neurological issues.
Post-polio syndrome (PPS): Latent symptoms that arise after a polio infection, characterized by declining muscular function, acute weakness, pain, and fatigue. These symptoms can occur 15 to 30 years after an initial acute paralytic attack or after a non-paralytic polio infection.
Guillain Barre syndrome (GBS): A gradually experiencing muscle weakness induced by the immune system impairing the peripheral nervous system. Initial symptoms typically involve changes in sensation or pain, often in the back, along with muscle weakness that starts in the feet and hands and can spread to the arms and upper body.
Stroke: A condition where blood flow to the brain is restricted, leading to the death of brain cells. Symptoms manifest based on the affected area of the brain.
Traumatic Brain Injury (TBI): Dysfunction of the brain resulting from a bump, blow, or sudden jolt to the head.
Parkinson’s disease: A neurodegenerative disorder primarily affecting dopamine neurons in the brain, leading to movement, sleep, and cognitive impairments.
Alzheimer’s disease: A neurodegenerative disease that causes degeneration of brain cells, resulting in dementia characterized by memory decline, impaired thinking, and behavioral changes.
Spinal Cord Injuries: Injuries to the spinal cord, such as from trauma, can disrupt nerve communication between the brain and body. This can cause weakness, loss of strength and sensation, impaired breathing, and loss of bowel or bladder control below the site of injury.
Multiple Sclerosis (MS): An autoimmune disease where the immune system damages the nerves of the central nervous system, leading to the degradation of myelin, the protective covering of nerves. Symptoms and signs vary relying on which nerves are affected.
Cerebral Palsy: A childhood disorder characterized by motor disability and difficulties with movement, balance, and posture due to abnormal brain development.
Charcot-Marie-Tooth Disease (CMT): A hereditary disorder that causes progressive loss of muscle tissue due to damage to peripheral nerves.
Amyotrophic Lateral Sclerosis (ALS): A neurodegenerative disease that affects motor neurons, resulting in the loss of voluntary movement as motor neurons die off.
Chronic Pain: Neurological physiotherapy can also help manage chronic pain conditions, including back pain, that may be primary or secondary to other neurological disorders. Chronic pain significantly impacts the quality of life, making neurological physiotherapy a valuable option.
Neurorehabilitation is not a one-size-fits-all approach. The process is individualized for each patient and depends on the extent of nerve damage and loss of bodily functions. Fortunately, there are various neurorehabilitation options available to help patients overcome challenges and adapt to their physiological changes, leading to improved quality of life and increased independence.
Conclusion
Neurological rehabilitation plays a vital role in the recovery process, emphasizing the importance of a collaborative approach. With the support of family, friends, the community, and the medical team, patients can make significant strides in their healing journey and regain their ability to reintegrate into society.
The primary objective of a neurological rehabilitation program is to enhance physical, emotional, and social well-being, enabling patients to regain their highest level of functioning and independence. Through these programs, individuals often achieve the ability to live autonomously, leading to increased happiness and overall satisfaction in their lives.
FAQ
What are the components of neurological rehabilitation?
Rehabilitation is frequently defined as a procedure that begins when the diagnosis is completed and resumes as extended as the individual requirements interventions. This procedure contains four steps: assessment, goal setting, interventions, and outcome measurement.
What are the different types of neurological therapy?
These include physiotherapy, occupational therapy, rehabilitation psychology, speech & swallowing therapy, vision therapy, language therapy, and therapies concentrated on everyday function & community reintegration.
Can physiotherapy help neurological rehabilitation?
The Part of a Neurological Physiotherapist
Neurological physiotherapists must be experienced and well prepared to regale neurological illnesses with the purpose to deliver interventions that help a person recover and maintain their full motion and functional freedom.
What are the top 3 neurological disorders?
Among the most ordinary are epilepsy, Alzheimer’s, and stroke.
Neurological illnesses are central and peripheral nervous system illnesses, they happen in the brain, spine, and multiple nerves that unite both.
What is brain rehabilitation?
Brain rehabilitation therapy benefits individuals who relearn functions lost as a consequence of brain damage. These may contain everyday actions like eating, dressing, walking, and speech. Brain injuries can impact individuals in many various ways.






7 Comments