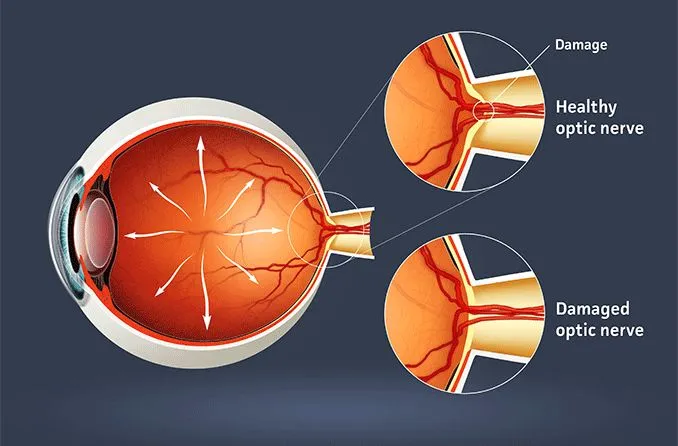
Optic nerve (CN- 2)
The optic nerve is highly important for your vision. It’s the 2nd cranial nerve out of 12 cranial nerves and part of your central nervous system, which includes your brain and spine.
The optic nerve travels electrical impulses from your eyes toward your brain. Your brain processes according to sensory information so that you can see.
Introduction
Perception of the eclectic variation of shapes, colors, and sizes that live across the world is dependent on the proportionally small, spherical eyeballs. There are multiple segments of the eye that permits images to be exposed or detected. However, recognition or identification, and interpretation of these objects are primarily dependent on the optic nerve.
The identity of cranial nerve II (CN II), also known as the optic nerve, anticipates Galenic anatomy. The optic nerve is responsible for communicating special afferent impulses of light to the brain. It is also included in different reflex arcs interconnected to the ocular system. It is a unique structure that role as the bridge between the retinal layer of the eyes and the visual cortex of the brain.
Anatomy
- The optic nerves are paired, cylindrical structures that expand from the posterior segment of the eyeball (roughly 2 mm medial to the posterior pole) to the suprasellar space or expanse in the middle cranial fossa. It comprises roughly or about 1 million myelinated axons of the ganglion cells of the retina. second Cranial nerve II is myelinated by oligodendrocytes and not Schwann cells like the axons of peripheral nerves. While there is significant or remarkable variability in the measurements of the optic nerve (even between optic nerves within the same individual), the average (mean) length of the structure ranges between 35 mm and 55 mm.
- It can be classified into four major parts:
- The optic nerve head (i.e. intraocular portion measures around 1 mm in length.
- The intraorbital portion is about 25 mm in length.
- The optic foramen portion is the most variable or irregular, with measurements between 4 – 10 mm in length.
- The Intracranial portions account for about 10 mm of the total length of the nerve.
Intraocular part of the CN II
- The optic nerve head is the most anterior component or part of the optic nerve and corresponds or communicates to the 1 mm portion that is situated within the eyeball (i.e. the intraocular part). Historically, it was the concept to be an elevated organization extending from the retinal surface and by expansion, was mentioned too as a papilla (hence the term, papilloedema). However, it has since been found that the optic nerve is in reality level with the retina, therefore the term papilla is an old incorrect word that is still used sometimes with reference to the head of the optic nerve.
- The optic nerve head (also known as the optic disc) is about 1.5 mm wide and is also related to a physiological cup that communicates to a central depression in the optic nerve head. The measurements of the cup and disc are dependent on the inclination or orientation shape and size of the corneoscleral canal that lives at Bruch’s membrane. The conical corneoscleral canal leads to widening in the anteroposterior direction.
- The optic nerve head is a unique portion of CN II in that it marks a very important point of vascular, geometric, and tonometric transition or change. At the optic nerve head, the optic nerves are movable to the relatively low-pressure space of the retro-orbital area from the much higher intraocular pressure zone. Furthermore, there is an alteration in the blood supply from the central retinal artery to the ophthalmic and posterior ciliary arteries. The nerve fibers make a sharp 90 degrees turn to penetrate the lamina membrane. Finally, they not only become myelinated but are also enclosed in the meningeal layers or coating in the extraocular areas.
Intraorbital part of CN II
- The 25 mm of optic nerve runs from the posterior portion of the eyeball (a few millimeters medial to its posterior pole) to the intraorbital opening of the optic canal is called the intraorbital portion. The optic nerve fibers distal or end part of the lamina membrane are myelinated, while those precursors to the lamina membrane are unmyelinated. Therefore the diameter of the intraorbital portion of the optic nerve is twice the width of the intraocular portion.
- The intraorbital optic nerve is also adjoining by all three meningeal layers(meninges covering the brain) (i.e. dura, arachnoid, and pia mater). The arachnoid and dura mater is normally loosely attached proximally and are interrelated with a substantial or larger subarachnoid space (giving it a bulbous appearance) at the posterior pole of the eyeball. The subarachnoid space narrows remarkably at the orbital orifice of the optic canal.
- Just before it enters the optic canal, CN II can be obtained adjacent to CN III, CN VI, and the nasociliary nerve, and superomedial to the ophthalmic artery. Within the canal, there are many fibrous dural attachments that expand to the pia mater. Earlier in its course, orbital fat or disparate the optic nerve from the surrounding or nearby extraocular muscles. However, the nerve becomes more closely associated with the annulus of Zinn, where the four recti get originate.
- Within the optic canal situated in the intracanalicular portion of the optic nerve. The optic canal is initiated within the lesser wing of the sphenoid bone. There is a remarkable variance in the thickness of the walls of the optic canal similar in that the thickness increases or enlarges from medial to lateral, and from superior to inferior.
- The optic canal runs posteromedially at a 35 degrees angle compared to the midsagittal plane. Like the preceding intraorbital portion, the intracanalicular portion is also enclosed or surrounded by the meninges described or represented earlier. It has a variable length measurement between 4 – 10 mm. The extra length (in addition to the length of the intraorbital component) permits additional or extra movements of the eyeball within the orbit. It is otherwise structurally identical to the earlier intraorbital segment.
Intracranial part
- The last 10 mm of the optic nerve is the intracranial portion. It expands from the internal orifice of the optic canal and runs above the diaphragm sellae before crossing above the suprasellar portion of the cavernous sinus. Here, the optic nerve combines with its contralateral Cranial nerve II to form the optic chiasm. There are also very important vascular structures that are closely or sharply related to the intracranial optic nerve:
- it is situated medial to the internal carotid artery
- it is superomedial to the ophthalmic artery
- and inferior (below) to the anterior cerebral artery.
- The pia mater is the only meningeal layer (coating) covering the intracranial optic nerve.
Optic chiasm
- The optic chiasm marks a very important portion of Cranial nerve II. Recall that the retina can be subdivided or bifurcated into nasal and temporal halves, which can be further subdivided or bisected into superior and inferior poles. The nasal side of the left eye and the temporal side of the right eye collect input from the temporal and nasal visual fields, individually (i.e. left visual field). Similarly, light from the right visual field is exposed by the temporal side of the left eye and the nasal side of the right eye.
- At the optic chiasm, the optic nerve fibers get originate from the temporal side of the retina of the right eye and continue or resume in the right optic tract (post chiasmatic portion of the optic nerve). At the point of the intersecting, the fibers that get originated from the nasal field of the left eye, traverse and enter the right optic tract. Therefore, visual input from the left visual field runs in the right optic tract. A similar intersection occurs with fibers originating in the nasal side of the contralateral eye.
Optic nerve histology
About one million nerve fibers that make Cranial nerve II can be classified into five groups:
- The nerves responsible for communicating visual impulses are the visual afferent fibers. They run from the retina to the lateral geniculate body of the thalamus.
- Nerve fibers that run to the tectum to control the pupillary light reflex are termed pupillary afferent fibers.
- Efferent fibers to the retina have been recognized but their role is to be interpreted.
- Some fibers run to the superior colliculus and are termed photostatic fibers. They participate or cooperate in the visual body reflexes.
- Finally, there are autonomic fibers that also run alongside or closed by the optic nerve within the optic canal; but they do not pierce the nerve.
- There are indefinite differences in the analysis planning of the optic nerve through its course. It is easier to follow the analysis by subdividing the optic nerve into its comprising portions (i.e. head, intraorbital, intracanalicular, and intracranial segments)
Nervous layer
- additionally, to having neural tissue, the optic nerve head is also occupied by nonneural components or portions similar to astrocytes, fibroblasts, and capillary-interrelated cells. The optic nerve head can be again subdivided into the surface nerve fiber layer or coating, prelaminar area, and lamina cribrosa. The inner limiting membrane of Elschnig (formed by a collection of astrocytes) is responsible for dividing the anterior extremity or boundary of the nerve head – the surface nerve fiber layer – from the vitreous or shiny humor that fills the eyeball. The inner limiting membrane becomes greatly thickened centrally at the physiological cup, and is referred to or mentioned to as the central meniscus of Kuhnt. However, as the cup gets larger or bigger (i.e. the corneoscleral canal gets wider) the membrane gets thinner. The surface nerve fiber layer is highly vascular with many capillary networks, and large retinal arteries and veins run via it. The layer also comprises the tightly encase axons of the ganglion cells.
- Deep to the surface nerve fiber layer is the prelaminar area of the optic nerve. It has also been mentioned as the choroidal or glial layer. The principal component of this layer is glial tissue. There is, however, connective tissue established in the perivascular areas of the layer. Histologically, the distinguishing characteristic between connective tissue and glial tissue is the diameter of the fibers. The connective tissue fibers are thicker or broader than the glial fibers, and glial fibers run in a perpendicular direction corelative to the nerve bundles. In the periphery of the head of the optic nerve, the glial fibers are attached or fixed to the elastic membrane and choroid; while in the center of the optic disc, the optic nerve has attachments or addition to the perivascular connective tissue.
- The glial cells are densely or tightly packed and flattened in the anteroposterior plane, with many capillaries present around the cell layer. The prelaminar glial tissue provides structural support to the axons of the ganglion cells as they form or make the perpendicular bend from the retina to form the optic nerve. All nerve fibers expanding from the surface nerve fiber layer or coating to the prelaminar area are unmyelinated.
- Deep to the prelaminar area is the lamina membrane area of the optic nerve head. This is an extremely fenestrated (about 200 – 300 holes) area that permits passage of the optic nerve axons into the extraocular space. As the nerve fibers convey (myelinated by oligodendrocytes) through the fenestra of the lamina membrane, they make a relatively tight or dense seal in order to protect the retrolaminar tissue from the relatively high intraocular pressures. The lamina membrane has a concave and convex area or surfaces anteriorly and posteriorly, individually.
- There is a very poor or imperfect distinction between the prelaminar and deeper connective tissue area. It, therefore, has a correlative mixture of both glial and connective tissues and is mentioned as a transitional area. The connective tissue forms a full-thickness layer of tissue that covers or coats the optic nerve head. It is organized into thick columns across the periphery that presents the lamina membrane to the adjacent sclera.
- The intraorbital portion of the Cranial nerve II is adjoining by myelin from oligodendrocytes, as well as the three meningeal layers. The pia mater is intimately related to the optic nerve. It is divided from the overlying arachnoid mater by cerebrospinal fluid (CSF). The dura mater provides the final sheath or encasement (similar to the rest of the central nervous system). There are intervening connective tissue septae that comprise a vascular structure that runs longitudinally and transversely. They have inter-connective tissue connections, as well as relationships to the optic nerve. At the periphery, the horizontal septae fix or attach the pia mater to the posterior side of the lamina membrane. Centrally, it fixes or attaches the pia mater to the perivascular fibrous sheaths or coating.
Frontal eye fields
- In addition to the many thalamocortical projections or predictions related or associated with vision, postsynaptic fibers from the primary visual field also run to the cerebrum to synapse and combine with the frontal eye fields (Brodmann areas 6, 8, and 9). This region of the brain has many connections with the thalamus, as well as the parietal lobe and temporal lobes; where it processes afferent signals interrelated to sight and sound. via its efferent tracts to the ipsilateral Edinger-Westphal and primary oculomotor nuclei, the frontal eye fields are capable to regulate or control rapid eye movements between fixation points or positions (saccadic movements).
Blood supply of the optic nerve
- There is some degree of variance in the blood supply of the optic nerve relying on the part of the nerve being discussed. In the center, the optic nerve is indirectly or secondarily supplied by the ophthalmic branch of the internal carotid artery. As the internal carotid artery comes out superiorly from the cavernous sinus, the ophthalmic artery separates and runs along with the ventral or anterior surface of the optic nerve within the optic canal. As the artery appears or comes out at the apex of the orbit, manufacture a triplicate of posterior ciliary arteries, along with the central retinal artery. The vessels run anteriorly in the substance of the optic nerve after they penetrate the structure about 10 – 12 mm from the earth.
- The surface nerve fiber layer or coating of the optic nerve head is perfused or copious by branches from the central retinal artery. Blood supply to the prelaminar area gets arises from the peripapillary and choroid vessels gets arising from the posterior ciliary arteries. The lamina membrane obtains its blood supply from the small posterior ciliary arteries and in some cases the circle of Zinn-Haller. The latter vascular anatomy is a conflict, however, it can be present in the sub-scleral space around the optic nerve at the neuro-ocular junction. influent to the Zinn-Haller network get arise from the choroidal vessels, pial arterial network, perineural arteries, and around 4 – 8 posterior ciliary arteries. The Zinn-Haller arterial network also provides branches to the laminar portion of the optic disc.
- The posterior ciliary arteries supply or innervate the orbital portion of Cranial nerve II through the pia mater vessels, which approach the nerve through fibrous septae. The internalized portion of the central retinal artery may also give arterial supply to the nerve here. Collateral blood supply gets arising from the middle meningeal branch of the external carotid artery may also innervate the intraorbital Cranial nerve II near the orbital apex.
- The intracanalicular portion of Cranial nerve II is situated in a watershed region supplied by the collaterals ophthalmic artery (anteriorly) and pial derivatives (original) of the superior hypophyseal and internal carotid arteries (posteriorly). Within the cranial vault, Cranial nerve II is innervated by the A1 segment of the anterior cerebral, the internal carotid, and the superior hypophyseal arteries. even though the optic nerve is examined as a diencephalic extension, the innervating vessels do not have a blood-brain barrier (BBB).
- Venous tributaries from all parts of the optic nerve in the end drain or exhaust to the central retinal vein. It then drains or exhausts either to the superior ophthalmic vein or directly into the cavernous sinus.
Embryology
- The optic placode, situated at the cranial end of the developing embryo, into the eye and surrounding or nearby structures. Evagination of an area of the forebrain wall gives rise to the retina of the eye. The outer portion of the optic cup is rich in small pigment granules and becomes the pigment layer or coat of the retina.
- The pars optica retinae form the posterior 80% of the neural layer or coating of the optic cup and enlarge into the rods and cones, which are answerable for light perception. The bipolar and parallel cells (of the outer nuclear layer), as well as the ganglion and amacrine cells (of the inner cell layer), gets arise from the mantle layer of the retina; which is also adjacent or near to the pars optica retinae. The bipolar cells allow communication between the photoreceptors and the ganglion cells. The amacrine and parallel cells are supportive cells present in the inner and outer plexiform layers of the retina, individually.
- The distal axons of the ganglion cells combine in the fibrous nerve fiber layer of the retina and unify in the administration of the optic trunk, which becomes prominent around the 4th week of gestation. It has a groove termed as the choroid fissure on the ventral (anterior) aspect of the stalk that residence the hyaloid vessels.
- By the 7th gestational week, closure of the choroid fissure manufactures a lumen that interfaces with the forebrain proximally and the optic vesicle distally. The walls of the optic stalk are made up of a monolayer of primitive epithelial cells. the introversion of the stalk results in shallow ventral depression. As the stalk lumen continues to shrink, the stalk itself is simultaneously enlarged. Glial cells are also added to the proximal portion of the stalk, where the optic disc forms. As more cells are attached to the luminal surface of the stalk, the hyaloid arteries relapse. During gestational week 8, there is subsequent distinct of the glial cell populations (of both the optic stalk and ventral forebrain) into type 1 and type 2 astrocytes, and oligodendrocytes.
- Growth and development of the optic nerve resume into the adolescent years. There is a continuous increase in the diameter of the nerve, with the intraocular part being smaller than the extraocular portion. This variation in diameter can be accounted for by the myelination that takes place in the extraocular portion of the nerve.
Clinical significance
- There are different pathological processes that can affect the optic nerve. The major ones explained here are related to the disease of circulation, intraocular pressure, and inflammation of the nerve. However, the nerve is also prone to a similar array of pathologies that affect the brain, including tumors similar to gliomas and meningiomas.
Anterior ischaemic optic neuropathy (AION)
- Anterior ischaemic optic neuropathy (AION) shares numerous similarities with the cerebrovascular occurrence mentioned as a stroke. The pathology occurs due to a disturbance of the blood supply to the optic nerve. This may result in a different spectrum of disorders ranging from ischemia to infarction with necrosis.
- The intensity of the injury depends on the degree and time of the vascular obstruction. A Milder type of anterior ischemic optic neuropathy (AION) may occur with temporary interference of blood flow to the optic nerve; known as temporary vision loss. Like the brain, the optic nerve does not regenerate or regrowth once severely damaged (infarctions). Therefore, visual impulses reduced by that area of the optic nerve will be permanently lost. While underlying disorders similar to vasculitis, embolic occurrence, or a thrombotic event may cause AION, the likelihood of advanced atherosclerosis as the cause of vascular occlusion should not be ignored.
- doctors should have a high degree of impression with arterial injuries of the eye, as they normally indicate that there is an increased risk that a similar ischaemic incident may occur elsewhere in the body (i.e. in the heart leading to myocardial infarction, in the brain causes the stroke, or in the kidneys causes marked renal impairment). On funduscopic examination, the optic disc in anterior ischemic optic neuropathy (AION) will appear pale, and the margins will seem blurry (swollen).
Papilledema
- Papilledema refers to inflammation(edema) at the optic nerve head of both optic nerves. This may present unilaterally(one side) or bilaterally(both sides). In the case of unilateral or one-sided papilledema, the likely cause is a mass effect from a primary optic nerve tumor. Bilateral(both sides) papilledema is more likely related to increased intracranial pressure.
- An increase in the perineural compulsion may compromise or manage the venous drainage of the nerve. eventually, the transportation of intracellular contents via the neuron will be disrupted or deranged; resulting in inflammation of the disc. Clinically, this occurrence is observed as blurring of the optic disc margins and the disc seems hyperaemic on funduscopic examination.
FAQ
What damages the optic nerve?
The optic nerve can also be damaged or injured by shock, toxins, radiation, and trauma. Eye disorders, similar to glaucoma, can also lead to a form of optic nerve atrophy. The condition can also be caused by any disorder of the brain and central nervous system (CNS).
What controls the optic nerve?
It’s an expansion of the central nervous system (CNS), which involves the brain and spine. The optic nerve transfers the electrical stimulation from the eyes to the brain. the brain proceeding this sensory information so that we can see.
Can optic nerve recover?
Human optic nerve cells decrease the capability to regenerate or regrowth and to re-establish neuronal wiring from the eye to the brain. in addition, there are no FDA-approved drugs or surgeries that prevent or intercept the death of the cells that make the optic nerve, block nerve degeneration, or stimulate nerve regeneration.
How sensitive is the optic nerve?
Optic nerve ultrasonography has 94% reactivity and 87% accuracy for diagnosing increased intracranial pressure | Annals of Internal Medicine.
What can block the optic nerve?
Ischemic optic neuropathy is an injury to the optic nerve caused by a blockage or obstruction of its blood supply.
obstruction can occur with inflammation or swelling of the arteries (called arteritis, typically as a segment of a disorder called giant cell arteritis.
The only continuous symptom is painless vision loss, which is normally sudden.
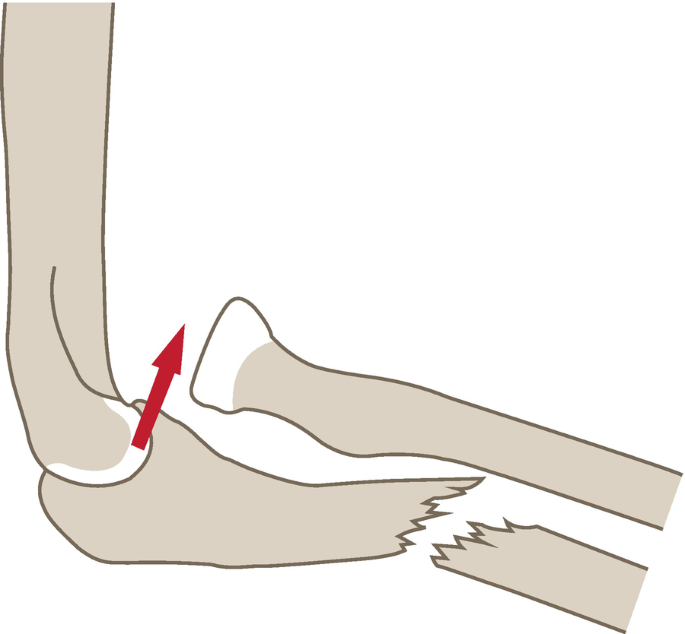
What happens if the optic nerve is injured?
Traumatic Optic Neuropathy (TON) is a disorder in which acute injury to the optic nerve from direct or indirect trauma lead to vision loss. The intensity of optic nerve damage may range from simple swelling to complete avulsion of the optic nerve.
What is optic nerve weakness?
Optic neuritis takes place when swelling (inflammation) damages or injured the optic nerve — a bundle of nerve fibers that transmits visual information from the eye to the brain. Common symptoms of optic neuritis involve pain with eye movement and temporary loss of vision in one eye.
Do you have 2 optic nerves?
Visual Pathways and the Consequences of Damage
Nerve signals run along with the optic nerve from each eye. The two optic nerves converge or meet at the optic chiasm. There, the optic nerve from each eye split, and half of the nerve fibers from each side cross to the other side.
What is the best treatment or management for optic nerve damage?
For most people, the best treatment is the surgery to detach or move whatever is compressing the optic nerve before the compression causes permanent damage.
Is optic nerve damage serious?
The optic nerve is a bundle or group of more than 1 million nerve fibers that conduct visual messages. we have one connecting the back of each eye to the retina) to the brain. Damage or injury to an optic nerve can lead to loss of vision. The type of vision loss and how severe or intense it is depends on where the damage occurs.
How can I protect my optic nerve?
preserving maximal blood flow to the optic nerve. Optimal blood flow is vital to preserving a healthy optic nerve.
preserving healthy eye pressure (intraocular pressure).
assisting mitochondrial health.
Limiting exhibition to oxidation with antioxidants.


One Comment