Sprengel’s Shoulder Deformity
What is a Sprengel’s Shoulder Deformity?
Sprengel’s shoulder deformity, also known as congenital high scapula or undescended scapula, is a rare congenital condition that affects the development and positioning of the shoulder blade (scapula) during early fetal development. This condition is named after the German surgeon Carl Sprengel, who first described it in 1891.
→In Sprengel’s Shoulder scapula fails to descend down from its initial high position in the embryo.
→Here the scapula lies more superiorly. It is hypoplastic and improperly shaped. It is associated with other congenital deformities like cervical ribs.
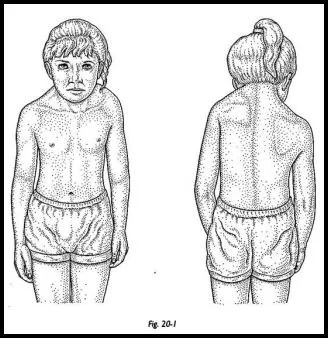
In a typical case of Sprengel’s shoulder deformity, one scapula fails to descend to its normal position in the back, causing it to be located higher on the affected side of the body. As a result, the scapula may appear elevated, rotated, and abnormally small compared to the other side. The condition can affect either one or both shoulders, but it is more commonly found on the right side.
History:
It has the name of German surgeon Otto Gerhard Karl Sprengel (1852–1915), who wrote about four cases in 1891.
Anatomy Related to Sprengel’s Shoulder
Some vital structures are at risk during the extensive dissection that is required as part of the relocation procedure. These structures include the following
- Dorsal scapular nerve
- Spinal accessory nerve
- Suprascapular nerve
→The dorsal scapular nerve courses close to the superomedial border of the scapula in the plane between the rhomboid and the erector spinae. The dorsal scapular nerve remains anterior to the serratus anterior and the subscapular muscles.
There exists a risk of injuring the dorsal scapular nerve during dissection of the periscapular muscles at the superomedial angle of the scapula, and when the trapezius and rhomboid muscles are reflected off as a single unit from the spine in the Woodward procedure (see Treatment). Therefore, staying subperiosteal during the process of freeing the periscapular muscles is essential, especially at the superomedial angle of the scapula.
→The spinal accessory nerve is located between the trapezius and rhomboid muscles and therefore is theoretically at risk; however, because this nerve is sandwiched between the two muscles, it is rarely ever injured when these muscles operate as a unit.
→The suprascapular nerve runs in the suprascapular notch of the scapula and may be injured if the dissection is carried too far laterally when the superior portion of the scapula is resected. By staying at least 1 cm medial to the notch, injury to the nerve during the procedure can be avoided.
Causes of Sprengel’s Shoulder
The exact cause of Sprengel’s shoulder deformity is not always clear, but it is believed to be a result of abnormal development during early embryonic stages. Some cases may be associated with other congenital anomalies or syndromes, such as Klippel-Feil syndrome, which affects the development of the cervical spine.
Sprengel’s Shoulder is a congenital disorder that develops and occurs by:
- Early prenatal development is disturbed.
- This may be due to imperfect descent of the shoulder girdle by the third month or a band of muscle from the skull to the scapula which fails to grow.
- Genetic defect.
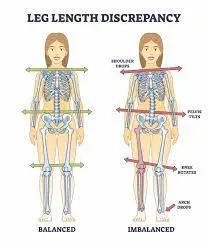
- Klippel-Feil syndrome, clavicular abnormalities, rib abnormalities, limb length disparity, scoliosis, spina bifida, hemivertebrae, and underdevelopment (hypoplasia) of neck or shoulder muscles may all be linked to Sprengel’s deformity.
Pathology
Because a healthy scapula is necessary for the development of neighboring structures, Sprengel’s deformity frequently affects them. The most typical symptom is a raised scapula, but other signs include weak surrounding musculature. an interruption to the growth of muscles, cartilage, and bones. There may be an absence or a deficiency in the trapezius, rhomboids, levator scapulae, pectoralis major, latissimus dorsi, and sternocleidomastoid. The scapula may wing if the serratus anterior muscle is weak.
Epidemiology
The majority of findings in the medical literature claim that females are 3 times more likely than males to experience Sprengel malformation. According to some other studies, stated that the condition can affect both men and women equally.
Associated Conditions
The majority of the time, Sprengel’s Shoulder coexists with other congenital anomalies, notably those affecting the vertebrae and ribs. It is common to have an omovertebral bar, which is a fibrous, cartilaginous, or osseous link between the scapula and cervical spine.
Additionally, it is frequently accompanied with hypoplasia or atrophy of the local muscles, and these characteristics can lead to increased misalignment of the shoulder and restricted shoulder motion.
The following abnormalities and disorders are frequently present in patients with Sprengel deformity:
- Klippel-Feil syndrome
- spina bifida
- kyphoscoliosis
- torticollis
- underdevelopment of the clavicle or humerus
Any patient presenting with Sprengel deformity needs to be evaluated for these potential co-existing abnormalities.
Symptoms of Sprengel’s Shoulder Deformity
Sprengel’s shoulder deformity symptoms can vary based on the severity and any underlying abnormalities that may be present.
- misalignment of the shoulders.
- The scapula is high 2 to 10 cm
- A bump at the base of the neck may result from a raised shoulder blade.
- nearby muscles that are underdeveloped.
- restricted range of motion (ROM) of the affected side’s shoulder and arm.
- restriction on shoulder elevation and abduction.
- cervical spine mobility is limited or restricted.
- Deformities of the neck can range from moderate torticollis to severe spine deformities like kyphoscoliosis.
- Crania bifida and spina bifida may be present
Classification
The Cavendish classification is used for grading Sprengel’s Shoulder Deformity:
| Grade | Level of Sprengel’s Shoulder Deformity |
| grade 1 | Very mild deformity When wearing clothing, the abnormality becomes almost invisible. |
| grade 2 | Although still deformity is small, the abnormality is visible as a bump. The high scapula’s superomedial region is convex and has a bump on it. |
| grade 3 | moderate Sprengel’s Shoulder deformity with 2–5 cm of apparent shoulder elevation |
| grade 4 | significant abnormalities with neck webbing and >5 cm elevation of the affected shoulder |
Diagnosis
Diagnosing Sprengel’s shoulder deformity typically involves a combination of medical history, physical examination, and imaging studies.
Medical history: The doctor will start by gathering information about the patient’s medical history, including any family history of congenital conditions or syndromes that might be related to Sprengel’s shoulder deformity.
Physical examination: A thorough physical examination will be performed to assess the patient’s shoulder and upper back. The doctor will look for signs of asymmetry, abnormal scapula position, shoulder range of motion limitations, and any associated abnormalities or physical features.
Diagnosis of specific symptoms, a comprehensive clinical assessment, and several types of specialized testing, including advanced imaging studies, all contribute to the diagnosis of Sprengel deformity.
X-Ray
Sprengel deformity can be correctly identified via a chest radiograph, often known as an anteroposterior chest x-ray. ‘Front to back’ is what the term ‘anteroposterior’ denotes. This X-ray examination places the subject’s back against the film plate with the X-ray in front of them. Elevation and rotation of the affected scapula are seen, with the inferior angle pointed laterally.
CT Scan
Evaluation of the omovertebral connection, scapula dysplasia, and malpositioning is done using a CT scan with 3D reconstruction. It is helpful for preoperative planning.
Computed tomography (CT) scans and magnetic resonance imaging (MRI) are two advanced imaging modalities that are frequently used to confirm a diagnosis of Sprengel deformity. When doing a CT scan, x-rays and a computer are utilized to produce a film that shows cross-sectional pictures of certain tissue features.
Magnetic resonance imaging (MRI)
Magnetic resonance imaging (MRI) creates cross-sectional pictures of body tissues using magnetic field waves. These examinations can make an omovertebral bone visible. The preparation and supervision of surgical operations can also benefit from the use of advanced imaging methods.
Due to the possibility of overlaid bones, it can often be challenging to identify an omovertebral bone on imaging investigations.
Treatment of Sprengel’s Shoulder Deformity
Treatment for Sprengel’s shoulder deformity typically involves a multidisciplinary approach, including input from orthopedic surgeons, physical therapists, and other specialists. The primary goal of treatment is to improve the range of motion and functional abilities of the affected shoulder. Conservative measures may include physical therapy to strengthen the muscles around the shoulder and improve posture.
In more severe cases or when conservative measures are insufficient, surgical intervention may be considered. Surgical procedures can involve repositioning the scapula, releasing soft tissue attachments that restrict movement, and addressing any associated anomalies.
Physiotherapy Treatment
Physical therapy plays a crucial role in the management of Sprengel’s shoulder deformity. The primary goals of physical therapy for this condition are to improve shoulder function, increase range of motion, strengthen muscles, and improve posture. The specific treatment plan will be tailored to each individual’s needs and the severity of their condition.
Here are some common physical therapy interventions used in the treatment of Sprengel’s shoulder deformity:
- Range of motion exercises: Physical therapists will design exercises to improve the range of motion of the affected shoulder. These exercises may include shoulder flexion, abduction, external and internal rotation, and scapular movements.
- Strengthening exercises: Strengthening the muscles around the shoulder and scapula is important for improving stability and function. Specific exercises will target the deltoids, rotator cuff muscles, and scapular stabilizers.
- Postural training: Correcting posture is essential in managing Sprengel’s shoulder deformity. Physical therapists will work with patients to develop proper postural alignment and provide exercises to strengthen the muscles that support good posture.
- Stretching: Stretching exercises help to lengthen tight muscles and improve flexibility. Targeting tight muscles around the shoulder and upper back can help improve overall shoulder mobility.
- Manual therapy: Hands-on techniques may be used by physical therapists to mobilize and manipulate the shoulder joint and surrounding soft tissues, helping to improve joint mobility and reduce muscle tightness.
- Assistive devices: In some cases, assistive devices like slings or braces may be recommended to support the shoulder and provide stability during the healing process or while performing specific activities.
- Functional training: Physical therapists will focus on functional activities that simulate real-life movements to improve the patient’s ability to perform daily tasks and activities.
- Patient education: Educating the patient and their caregivers about the condition, proper body mechanics, and exercises to be performed at home is an essential component of physical therapy treatment.
- Progress monitoring: Throughout the treatment process, physical therapists will monitor progress and adjust the treatment plan as needed to ensure optimal outcomes.
It’s important to note that the effectiveness of physical therapy depends on the individual case and the commitment of the patient to the prescribed exercises and interventions. For some individuals with severe Sprengel’s shoulder deformity, surgical intervention may be necessary, and physical therapy may play a role in post-surgery rehabilitation. As always, the treatment plan should be developed in collaboration with a qualified healthcare professional specializing in orthopedic and musculoskeletal conditions.
Surgical Treatment of Sprengel’s Shoulder Deformity
The deformity caused by Sprengel’s shoulder is treated surgically using a variety of techniques. The most often used approaches are those developed by the Woodward procedure and modified Green scapuloplasty. These treatments involve translating the scapula inferiorly to a more caudad position and removing the projecting section of the scapula and omovertebral bone. Osteotomy of the clavicle can also be performed to prevent brachial plexus damage.
The best way to decide which surgical technique to use is in close consultation with the patient’s family, doctors, and other members of the healthcare team. Decisions should be based on the particulars of the patient’s case, a thorough discussion of the benefits and risks, including any potential long-term effects, and additional relevant considerations.
Operative Procedures
Woodward procedure
To enable the scapula to travel inferiorly and rotate into increased shoulder abduction, medial parascapular muscles at the root of the spinous process are separated and then reattached.
Modified Woodward combines surgical descent with excision of the scapula’s upper medial border.
Schrock, Green procedure
After inferior movement of the scapula using traction cables, there is an extraperiosteal separation of the paraspinal muscles at the scapular insertion and reinsertion.
Clavicle osteotomy
in association with the above surgical procedures conducted before moving the scapula in cases of severe deformity to prevent brachial plexus damage.
Bony resection
Extraperiosteal excision of the proximal scapular prominence may be carried out alone or in conjunction with other surgeries for cosmetic reasons.
Outcomes
Woodward procedure and Schrock, Green procedure can improve abduction range up to 40-50 degrees.
Rehabilitation Following Surgery
The patient’s shoulder was immobilized following surgery to aid in the healing process and minimize potential discomfort.
The goal of physical therapy is to reduce deformity and enable the shoulder to move naturally.
Transcutaneous electrical nerve stimulation (TENS):
Pain relief is provided by transcutaneous electrical nerve stimulation, which may be triggered during stretching activities.
Ultrasound:
Adhesions are easily broken by ultrasound.
Thermotherapy:
Before beginning an exercise regimen, muscles are relaxed with thermotherapy.
Mobilization:
After six weeks, physiotherapy with ROM exercises that are both passive and active will start. To increase the range of motion and flexibility of the shoulder, gradual relaxed passive mobilization of the shoulder and scapula is performed. early scapular and shoulder mobilization, including abduction and elevation motions.
Strengthening exercises
All muscle group strengthening activities help to strengthen the weaker muscles. isometric and isotonic movements such as shoulder shrugs, shoulder rotations, pushups, arm supports, forearm supports, bridging, etc. can help to strengthen the shoulder girdle muscles.
Stretching exercise for Upper trapezius muscle:
The kid takes a relaxed sitting position on a chair. His right hand is placed just below her buttocks. By gripping the scapula’s acromion and lateral border, the therapist supports the child’s shoulder. The child then turns his neck to the left and flexes his neck. The kid then lays her left hand just below her thighs. By gripping the scapula’s acromion and lateral border, the therapist supports the child’s shoulder. The kid then turns his neck to the right and flexes his neck. During stretching, the kid holds the neck in these postures for 10 seconds.
Stretching exercises for Levator scapulae:
The kid is prone and has her head turned to the opposite side, towards the right. With her left hand, the kid keeps her head in flexion while simultaneously abducting as much of her right shoulder as he can without lifting the scapula. By holding the scapula, the therapist prevents scapular elevation.
Cross-body stretching:
The kid is lying on his back. Then therapist holds the acromion and lateral border of the scapula. The kid then flexes his right shoulder and elbow to 90 degrees. The kid grasps his right elbow with her left hand before extending her elbow as far to the left as she can.
Protraction exercise scapula:
The kid is supine as it is. while her elbow was completely extended and her right shoulder was flexed by 90 degrees. The kid then thrusts his right elbow forward with all of his strength. To stop the child’s scapula from elevating and their trunk from rotating, the therapist holds the acromion and grasps the scapula.
Posterior tilt exercise for scapula:
The child is lying on his back with the humerus above, the shoulder abducted to 130° to 145°, and the forearm neutral. The kid then places her left hand beneath her forehead and rests her palm’s dorsum gently on her forehead. The therapist prevents scapular elevation by grabbing the superior angle of the scapula as the patient raises her right arm with his elbow extended.
Family Education
Parents are encouraged to watch their children carry out all of their exercises. Parents should watch their children when they exercise at home to ensure appropriate scapular mobility and to prevent scapular elevation. The activity should be discontinued and the child should try it again if the superior border of the scapula shifts upward.
Prognosis
The prognosis for individuals with Sprengel’s shoulder deformity can vary based on the severity of the condition and the effectiveness of treatment. Early diagnosis and intervention can lead to better outcomes and improved shoulder function. However, it is important to note that Sprengel’s shoulder deformity is a complex condition, and individual cases may differ in their presentation and response to treatment. If you or someone you know is affected by this condition, it’s crucial to seek medical evaluation and management from qualified healthcare professionals.
Summary
Sprengel’s shoulder deformity is a rare congenital condition where one shoulder blade is abnormally high on the back. It can cause asymmetry, limited shoulder movement, and associated anomalies. Imaging, a physical exam, and medical history all go into making a diagnosis. Physical therapy aims to improve shoulder function, range of motion, and posture. Surgery may be considered in severe cases. For improved results, early diagnosis and management are essential.
FAQs
What causes Sprengel’s deformity?
The exact cause of Sprengel’s shoulder deformity is not always clear, but it is believed to be a result of abnormal development during early embryonic stages. Some cases may be associated with other congenital anomalies or syndromes, such as Klippel-Feil syndrome, which affects the development of the cervical spine.
How do you treat Sprengel’s shoulder?
Treatment for Sprengel’s shoulder deformity typically involves a multidisciplinary approach, including input from orthopedic surgeons, physical therapists, and other specialists. The primary goal of treatment is to improve the range of motion and functional abilities of the affected shoulder. Conservative measures may include physical therapy to strengthen the muscles around the shoulder and improve posture.
In more severe cases or when conservative measures are insufficient, surgical intervention may be considered. Surgical procedures can involve repositioning the scapula, releasing soft tissue attachments that restrict movement, and addressing any associated anomalies.
What is Sprengel’s deformity of the scapula?
Sprengel’s shoulder deformity, also known as congenital high scapula or undescended scapula, is a rare congenital condition that affects the development and positioning of the shoulder blade (scapula) during early fetal development.
Additionally, this disorder results in localized muscular hypoplasia or atrophy, which impairs shoulder mobility and deforms the shoulder.
What is the Sprengel Woodward procedure?
After removing the omovertebral bone or any other fibrous bands holding the scapula together, the Woodward treatment involves removing the origins of the trapezius and rhomboid muscles from the spinous process and pushing them downward.
Is Sprengel’s shoulder a disability?
Congenital elevation of the scapula, also known as Sprengel’s deformity, is a complicated deformity of the pectoral girdle that causes both visual and functional dysfunction.



2 Comments