Parkinsonism & Physiotherapy Exercise:
What is a Parkinsonism?
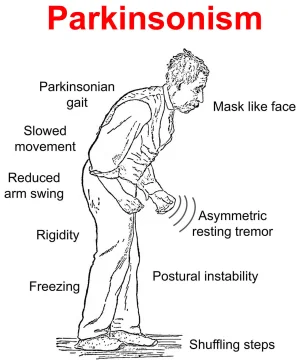
→ Parkinsonism is a clinical syndrome characterized by tremors, bradykinesia, rigidity, and postural instability.
→ Parkinsonism is any condition that causes a combination of the movement abnormalities seen in Parkinson’s disease — such as tremors, slow movement, impaired speech, or muscle stiffness — especially resulting from the loss of dopamine-containing nerve cells (neurons).
It has the name of James Parkinson, a physician who originally identified the illness in 1817.
Symptoms of Parkinson’s disease typically develop gradually and vary from person to person.
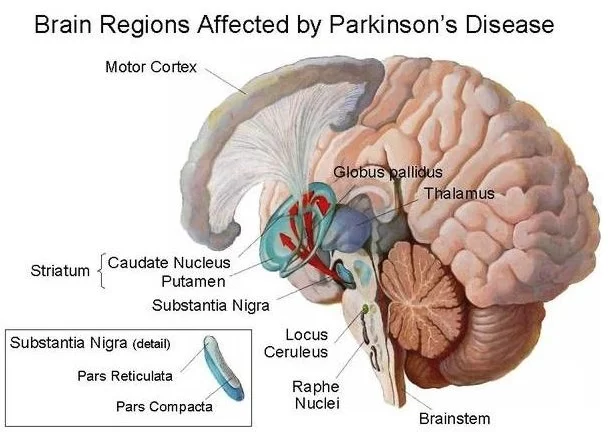
Related Anatomy:
→ Parkinsonism disease (PD) is a degenerative, progressive disorder that affects nerve cells in deep parts of the brain called the basal ganglia and the substantia nigra. Nerve cells in the substantia nigra produce the neurotransmitter dopamine and are responsible for relaying messages that plan and control body movement. For reasons not yet understood, the dopamine-producing nerve cells of the substantia nigra begin to die off in some individuals. When 80 percent of dopamine is lost, PD symptoms such as tremors, slowness of movement, stiffness, and balance problems occur.
→ Body movement is controlled by a complex chain of decisions involving inter-connected groups of nerve cells called ganglia. Information comes to a central area of the brain called the striatum, which works with the substantia nigra to send impulses back and forth from the spinal cord to the brain. The basal ganglia and cerebellum are responsible for ensuring that movement is carried out in a smooth, fluid manner.
Stages of Parkinsonism:
STAGE ONE – A Person usually has mild symptoms, such as tremors or shaking in a limb. Change such as poor posture, loss of balance, and abnormal facial expressions.
STAGE TWO – Symptoms affect both limbs and both sides of the body. The person usually has problems walking or balancing, and the inability to complete physical tasks becomes more apparent.
STAGE THREE – Symptoms can be severe and include the inability to walk straight or stand. there is a noticeable slowing of physical movements.
STAGE FOUR – The ability to walk is often limited
STAGE FIVE – The person is often unable to take care of herself and may not be able to stand or walk .she may need constant one on one nursing care.
Causes of Parkinsonism Disease:
The exact cause of Parkinson’s disease is still unknown, but it is believed to involve a combination of genetic and environmental factors. While most cases of Parkinson’s disease are sporadic, with no clear family history, a small percentage of cases are inherited.
→ Brain injury
→ Encephalitis
→ HIV/AIDS
→ Meningitis
→ Multiple system atrophy
→ Progressive supranuclear palsy
→ Stroke
→ Wilson disease
Other causes of secondary Parkinsonism include:
→ Brain damage caused by anesthesia drugs (such as during surgery)
→ Carbon monoxide poisoning
→ Certain medicines used to treat mental disorders or nausea
→ Mercury poisoning and other chemical poisonings
→ Overdoses of narcotics
→ MPTP (a contaminant in some street drugs)
Symptoms of Parkinson’s disease:
→ Symptoms of Parkinson’s disease differ from person to person. They also change as the disease progresses.
→ Symptoms typically begin appearing between the ages of 50 and 60. They develop slowly and often go unnoticed by family, friends, and even the person who has them.
→ The most common one is tremors.
Tremor. A tremor, or shaking, usually begins in a limb, often your hand or fingers. You may notice a back-and-forth rubbing of your thumb and forefinger, known as a pill-rolling tremor. One characteristic of Parkinson’s disease is a tremor in your hand when it is relaxed (at rest).
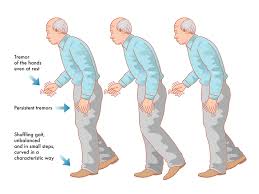
Slowed movement (bradykinesia). Over time, Parkinson’s disease may reduce your ability to move and slow your movement, making simple tasks difficult and time-consuming. Your steps may become shorter when you walk, or you may find it difficult to get out of a chair. Also, you may drag your feet as you try to walk, making it difficult to move.
Rigid muscles. Muscle stiffness may occur in any part of your body. The stiff muscles can limit your range of motion and cause you pain.
Impaired posture and balance. Your posture may become stooped, or you may have balance problems as a result of Parkinson’s disease.
Loss of automatic movements. In Parkinson’s disease, you may have a decreased ability to perform unconscious movements, including blinking, smiling, or swinging your arms when you walk.
Speech changes. You may have speech problems as a result of Parkinson’s disease. You may speak softly, quickly, slur or hesitate before talking. Your speech may be more of a monotone rather than with the usual inflections.
Writing changes. It may become hard to write, and your writing may appear small.
How to Diagnose Parkinson’s Disease?
→ Computed tomography (CT) scans of people with PD usually appear normal.
→ MRI has become more accurate in the diagnosis of the disease over time, specifically through iron-sensitive T2* and SWI sequences at a magnetic field strength of at least 3T, both of which can demonstrate the absence of the characteristic ‘swallow tail imaging pattern in the dorsolateral substantia nigra.
Treatment of Parkinson’s disease:
However, there is no permanent solution for this disease, various treatment options are useful to manage its symptoms and improve the quality of life for affected individuals.
Medical Treatment:
Medications such as levodopa, dopamine agonists, and MAO-B inhibitors are commonly prescribed to increase dopamine levels or mimic its effects. Physical therapy, occupational therapy, and speech therapy can help manage mobility issues and enhance daily functioning. In some cases, deep brain stimulation surgery may be considered to alleviate symptoms.
→ Carbidopa-levodopa.
→ Carbidopa-levodopa infusion.
→ Dopamine agonists.
→ MAO-B inhibitors.
→ Catechol-O-methyltransferase (COMT) inhibitors.
→ Anticholinergics.
→ Amantadine.
Physiotherapy Treatment in Parkinson’s Disease:
AIM OF PHYSIOTHERAPY-
→ Maintain and improve levels of function and independence, which will help to improve a person’s quality of life
→ Use exercise and movement strategies to improve mobility
→ Correct and improve abnormal movement patterns and posture, where possible
→ Maximize muscle strength and joint flexibility
→ Correct and improve posture and balance, and minimise risks of falls
→ Maintain a good breathing pattern and effective cough
→ Educate the person with Parkinson’s and their carer or family members
→ Enhance the effects of drug therapy
PLAN –
→ Visual cueing – a focus point to step over and initiate gait; strips of tape on the floor to initiate or continue walking through areas that cause slowing or freezing.
→ Auditory cueing – counting 1-2-3 to initiate walking; stepping to the beat of a metronome or specific music at a specified cadence to continue the rhythm of a walk.

→ Attention – Thinking about taking a big step; making a wider arc turn

Proprioceptive cueing – rocking from side to side ready to initiate a step; taking one step backward as a cue ready to then walk forwards.
Occupational therapy: Occupational therapy focuses on improving the performance of daily activities, such as dressing, eating, and bathing. It aims to enhance independence and compensate for any physical or cognitive challenges caused by Parkinson’s disease.
Speech therapy: Speech and swallowing problems are common in Parkinson’s disease. Speech therapy can help improve speech, articulation, and swallowing difficulties through exercises and techniques.
Deep brain stimulation (DBS): Deep brain stimulation is a surgical procedure in which electrodes are implanted in specific areas of the brain, such as the subthalamic nucleus or globus pallidus. These electrodes deliver electrical impulses to modulate abnormal brain activity and help reduce motor symptoms. DBS is typically considered for individuals who have experienced a good response to levodopa but have developed motor complications or fluctuations.
Lifestyle modifications: Certain lifestyle changes can help manage Parkinson’s disease symptoms. Regular exercise, a balanced diet, and sufficient rest can contribute to overall well-being. Avoiding excessive stress and maintaining a supportive social network are also beneficial.
Emotional and psychological support: Living with Parkinson’s disease can be emotionally challenging. Support groups, counseling, and other psychological interventions can provide emotional support, education, and coping strategies for both individuals with Parkinson’s disease and their caregivers.
Complications:
Parkinson’s disease can lead to various complications as the condition progresses. These complications can affect different aspects of a person’s physical and mental health. Here are some common complications associated with Parkinson’s disease:
- Falls and injuries: Balance and coordination problems, as well as the characteristic motor symptoms of Parkinson’s disease, can increase the risk of falls and injuries. Falling can cause fractures, head injuries, and other trauma, which may require medical intervention and rehabilitation.
- Swallowing difficulties: Parkinson’s disease can affect the muscles involved in swallowing, leading to dysphagia (difficulty swallowing). This can result in choking, aspiration (when food or drink enters the lungs), and malnutrition. Speech and swallowing therapy can help manage these difficulties.
- Cognitive changes and dementia: While not all individuals with Parkinson’s disease experience cognitive changes, some may develop difficulties with memory, attention, problem-solving, and other cognitive functions. In some cases, this can progress to Parkinson’s disease dementia, which includes symptoms such as confusion, hallucinations, and impaired judgment.
- Depression and anxiety: Parkinson’s disease can significantly impact a person’s emotional well-being. Many individuals with the condition experience depression, anxiety, and mood swings. These mental health issues can further affect quality of life and may require appropriate psychological support and treatment.
- Sleep disorders: Sleep disturbances are common in Parkinson’s disease. These can include insomnia, excessive daytime sleepiness, restless legs syndrome, and REM sleep behavior disorder, in which individuals act out their dreams physically.
- Freezing of gait: Freezing episodes involve sudden, brief periods where a person with Parkinson’s disease feels as though their feet are glued to the floor and cannot initiate or continue walking. Freezing of gait can lead to falls and contribute to mobility difficulties.
- Urinary problems: Parkinson’s disease can cause urinary issues such as urgency, frequency, and difficulties with bladder control. These problems can be managed with medications, physical therapy, and lifestyle modifications.
- Medication-related complications: Over time, individuals with Parkinson’s disease may experience complications related to their medications. These can include fluctuations in response to medication (resulting in “on-off” periods), dyskinesias (involuntary movements), and medication side effects such as nausea, hallucinations, or low blood pressure.
Summary:
Parkinson’s disease is a progressive neurological disorder characterized by the loss of dopamine-producing cells in the brain. It presents with symptoms such as tremors, slowness of movement, rigidity, and postural instability. In addition to these core symptoms, individuals may experience other motor and non-motor symptoms.
Medications, including levodopa and other dopamine-related drugs, are commonly prescribed to increase dopamine levels or mimic its effects. Physical therapy, occupational therapy, and speech therapy can assist in managing mobility issues and enhancing daily functioning.





Very Good Informative Information Rigarding Exercise Of Parkinson’s Disease