TROCHLEAR NERVE
INTRODUCTION :
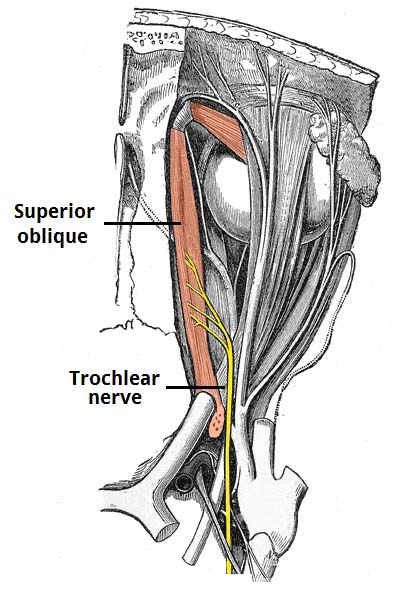
The trochlear nerve, also called the fourth cranial nerve or CN IV, is a motor nerve (a somatic efferent nerve) that innervates only a single muscle: the superior oblique muscle of the eye, which operates through the pulley-like trochlea.
The trochlear nerve is unique among the cranial nerves in several respects:
- It is the smallest nerve in terms of the number of axons it contains.
- It has the greatest intracranial length.
- It is the only cranial nerve that exits from the dorsal (rear) aspect of the brainstem.
- It innervates a muscle, the superior oblique muscle, on the opposite side (contralateral) from its nucleus.
The trochlear nerve decussates within the brainstem before emerging on the contralateral side of the brainstem (at the level of the inferior colliculus).
An injury to the trochlear nucleus in the brainstem will result in a contralateral superior oblique muscle palsy, whereas an injury to the trochlear nerve (after it has emerged from the brainstem) results in an ipsilateral superior oblique muscle palsy.
The human trochlear nerve is derived from the basal plate of the embryonic midbrain.
The words trochlea and trochlear (/’tr?kli?/, /’tr?kli?r/) come from the Ancient Greek trokhiléa, “pulley; block-and-tackle equipment”.
Anatomical Course :

The trochlear nerve arises from the trochlear nucleus of the brain, emerging from the posterior aspect of the midbrain (it is the only cranial nerve to exit from the posterior midbrain).
It runs anteriorly and inferiorly within the subarachnoid space before piercing the dura mater adjacent to the posterior clinoid process of the sphenoid bone.
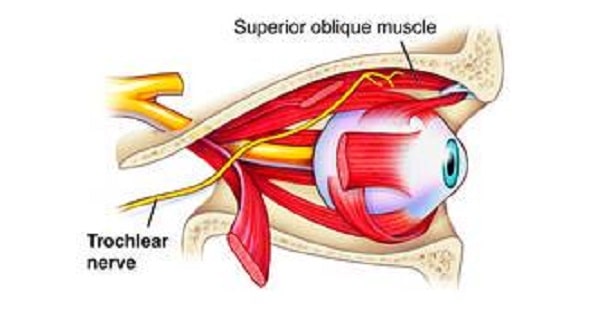
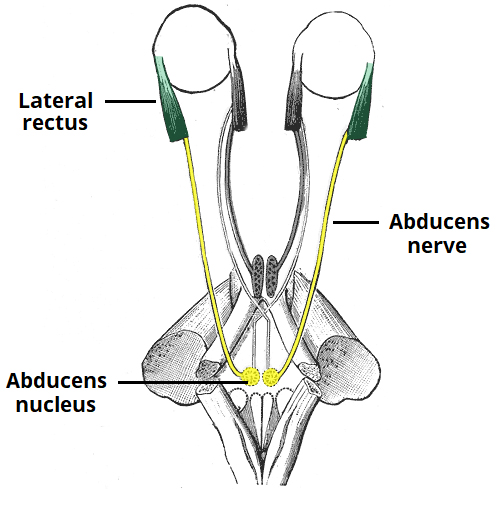
The nerve then moves along the lateral wall of the cavernous sinus (along with the oculomotor nerve, the abducens nerve, the ophthalmic and maxillary branches of the trigeminal nerve and the internal carotid artery) before entering the orbit of the eye via the superior orbital fissure.
Structure :
The Cavernous Sinus :
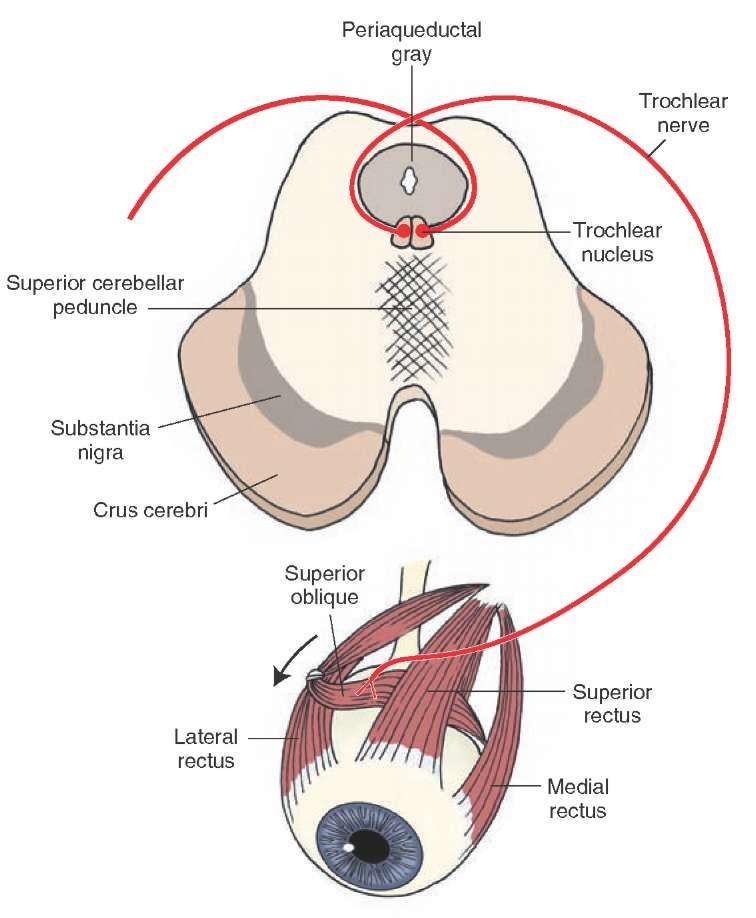
The trochlear nerve emerges from the dorsal aspect of the brainstem at the level of the caudal mesencephalon, just below the inferior colliculus.
It circles anteriorly around the brainstem and runs forward toward the eye in the subarachnoid space.
It passes between the posterior cerebral artery and the superior cerebellar artery, and then pierces the dura just under free margin of the tentorium cerebelli, close to the crossing of the attached margin of the tentorium and within millimeters of the posterior clinoid process.
It runs on the lateral wall of the cavernous sinus, where it is joined by the other two extraocular nerves (oculomotor—cranial nerve III and abducens—cranial nerve VI) and the first two branches of the trigeminal nerve (V), Ophthalmic (V1) and Maxillary (V2).
The internal carotid artery also runs within the cavernous sinus. Finally, it enters the orbit through the superior orbital fissure and innervates the superior oblique muscle.
Motor Function :
Superior oblique muscle and Function :
The trochlear nerve carries axons of type GSE, general somatic efferent, which innervate skeletal muscle of the superior oblique muscle.
The superior oblique muscle ends in a tendon that passes through a fibrous loop, the trochlea, located anteriorly on the medial aspect of the orbit.
Trochlea means “pulley” in Latin; the fourth nerve is named after this structure.
Actions of the superior oblique muscle :

Actions of the superior oblique muscle
In order to understand the actions of the superior oblique muscle, it is useful to imagine the eyeball as a sphere that is constrained :
Like the trackball of a computer mouse in such a way that only certain rotational movements are possible.
Allowable movements for the superior oblique Muscle :
(1) rotation in a vertical plane—looking down and up (depression and elevation of the eyeball)
(2) rotation in the plane of the face (intorsion and extorsion of the eyeball).
- The body of the superior oblique muscle is located behind the eyeball, but the tendon (which is redirected by the trochlea) approaches the eyeball from the front.
- The tendon attaches to the top (superior aspect) of the eyeball at an angle of 51 degrees with respect to the primary position of the eye (looking straight forward).
- The force of the tendon’s pull, therefore, has two components: a forward component that tends to pull the eyeball downward (depression), and a medial component that tends to rotate the top of the eyeball toward the nose (intorsion).
- The relative strength of these two forces depends on which way the eye is looking.
- When the eye is adducted (looking toward the nose), the force of depression increases.
- When the eye is abducted (looking away from the nose), the force of intorsion increases, while the force of depression decreases.
- When the eye is in the primary position (looking straight ahead), contraction of the superior oblique produces depression and intorsion in roughly equal amounts.
- The actions of the superior oblique muscle are (1) depression of the eyeball, especially when the eye is adducted (2) intorsion of the eyeball, especially when the eye is abducted.
- The clinical consequences of weakness in the superior oblique (caused, for example, by fourth nerve palsies) are discussed below.
- The tendon of the superior oblique inserts behind the equator of the eyeball in the frontal plane, so contraction of the muscle also tends to abduct the eyeball (turn it outward).
- In fact, each of the six extraocular muscles exerts rotational forces in all three planes (elevation-depression, adduction-abduction, intorsion-extorsion) to varying degrees, depending on which way the eye is looking.
- The relative forces change every time the eyeball moves—every time the direction of gaze changes.
- The central control of this process, which involves the continuous, precise adjustment of forces on twelve different tendons in order to point both eyes in exactly the same direction, is truly remarkable.
Clinical Relevance :
Examination of the Trochlear Nerve :
- The trochlear nerve is examined in conjunction with the oculomotor and abducens nerves by testing the movements of the eye.
- The patient is asked to follow a point (commonly the tip of a pen) with their eyes without moving their head.
- The target is moved in an ‘H-shape’ and the patient is asked to report any blurring of vision or diplopia (double vision).
Palsy of the Trochlear Nerve :
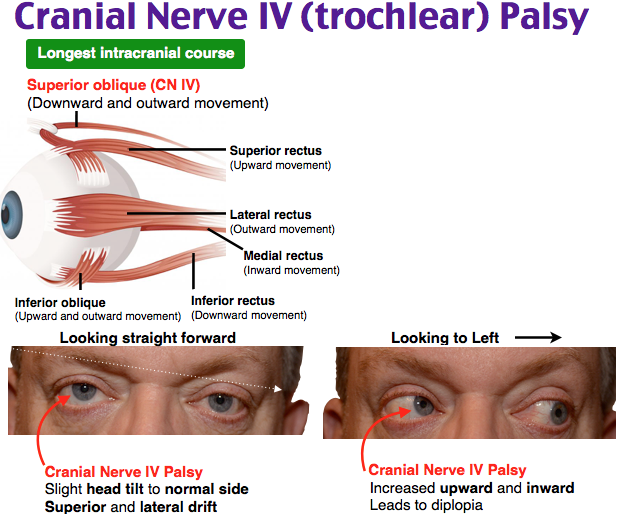
Trochlear nerve palsy commonly presents with vertical diplopia, exacerbated when looking downwards and inwards (such as when reading or walking down the stairs).
Patients can also develop a head tilt away from the affected side.
Vertical diplopia :
Vertical diplopia
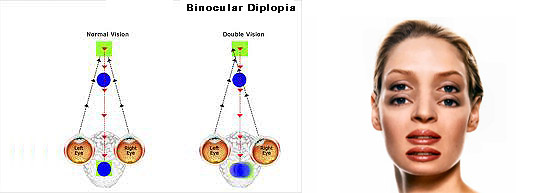
- Injury to the trochlear nerve causes weakness of downward eye movement with consequent vertical diplopia (double vision).
- The affected eye drifts upward relative to the normal eye, due to the unopposed actions of the remaining extraocular muscles.
- The patient sees two visual fields (one from each eye), separated vertically.
- To compensate for this, patients learn to tilt the head forward (tuck the chin in) in order to bring the fields back together—to fuse the two images into a single visual field.
Torsional diplopia :

Torsional diplopia
- Trochlear nerve palsy also affects torsion (rotation of the eyeball in the plane of the face). Torsion is a normal response to tilting the head sideways.
- The eyes automatically rotate in an equal and opposite direction, so that the orientation of the environment remains unchanged—vertical things remain vertical.
- Weakness of intorsion results in torsional diplopia, in which two different visual fields, tilted with respect to each other, are seen at the same time.
- To compensate for this, patients with trochlear nerve palsies tilt their heads to the opposite side, in order to fuse the two images into a single visual field.
- They are commonly caused by microvascular damage from diabetes mellitus or hypertensive disease.
- causes include congenital malformation, thrombophlebitis of the cavernous sinus, and raised intracranial pressure.



2 Comments