Pectoralis Minor Syndrome
What is a Pectoralis Minor Syndrome?
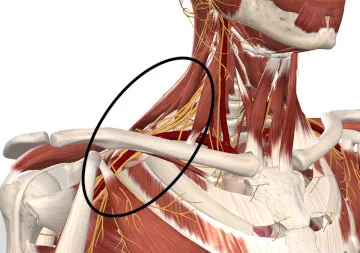
Pectoralis minor syndrome (PMS) is a condition that occurs when the pectoralis minor muscle, located under the chest wall, becomes too tight and compresses the nerves and blood vessels that pass underneath it. This can cause pain, numbness, and weakness in the shoulder, arm, and hand.
PMS is often caused by repetitive overhead activities, such as those performed in certain jobs or sports. It can also be caused by trauma to the chest or shoulder, or by poor posture.
Compression of the axillary artery, axillary vein, and brachial plexus (BP) nerves under the pectoralis minor muscle is known as pectoralis minor syndrome (PMS). PMS symptoms include arm, hand, shoulder, neck, and chest pain, as well as paresthesia and weakness in the arm and hand, which are signs of supraclavicular compression of the neurovascular bundle. PMS might be misdiagnosed as other upper extremity pain conditions. Along with the results of the physical examination, a thorough history that includes the patient’s work, regular activities, sports, and trauma is essential to the diagnosis.
The differential diagnosis can also benefit from radiological testing such as direct radiography, computed tomography, magnetic resonance imaging, and electrophysiological investigations. Doppler ultrasound of the arteries and veins, including dynamic imaging, can show arterial and venous compression. The final diagnosis is confirmed by injection tests. The majority of patients respond well to conservative treatment, and in cases where this is unsuccessful, surgical intervention is recommended.
The entrapment of the upper extremity neurovascular structures from the cervical area to the axilla results in thoracic outlet syndrome (TOS), which produces symptoms such as pain, paresthesia, weakness, numbness, swelling, coldness, tingling, and discoloration. It is categorized in a variety of ways. One claims that there are three anatomical levels where neurovascular compression might happen: the inter scalene triangle, the costoclavicular region, or the pectoralis minor (PM) area.
The interscalene triangle can entrap the brachial plexus and subclavian artery. The subclavian vein travels anterior to the triangle, not between the scalene muscles. The subclavian artery, vein, and blood pressure flow through the other entrapment location, which is the costoclavicular gap. In this area, subclavian vein compression is most common.
The coracoid process is attached to the PM space, which is directly behind the PM muscle. When the BP nerves, axillary artery (AA), and axillary vein (AV) are compressed in the PM region, pectoralis minor syndrome (PMS) results. Compression can happen above or below the clavicle, according to another TOS classification. Compression in the inter-scalene triangle and costoclavicular region occurs above the clavicle and causes TOS; compression in the PM space below the clavicle causes PMS.
The actual incidence of TOS in the general population is unknown in most cases. Since the diagnostic and categorization criteria are not yet thoroughly established, there are also some relatively incompatible results in the prevalence of neurogenic and vascular TOS and PMS. With the exception of abnormal cervical ribs, the cause of TOS and PMS is comparable. Acute traumas, repetitive everyday activities, exercises, sports, and employment are some of the factors that contribute to TOS and PMS. In the spectrum of neurogenic TOS, PMS can occur with the potential significance of neurovascular compression under the PM muscle tendon. In the majority of cases, TOS and PMS could be seen simultaneously, while pure PMS was present in 30% of the individuals exhibiting TOS symptoms.
The effectiveness of isolated PM muscle tenotomy to combined supraclavicular decompression (splenectomy, neurolysis, and first rib resection) and PM muscle tenotomy in patients with neurogenic TOS. This was done because of the significance of PMS in the presence of TOS symptoms. The authors noted similarities in the outcomes between the two groups and noted the significance of identifying PMS in order to successfully treat neurogenic TOS. However, conservative treatment is typically sufficient for PMS. These results are remarkable and emphasize the significance and frequency of PMS in patients presenting with symptoms of TOS. In direction to determine the location of the entrapment and administer the proper treatment, diagnostic injection tests are employed to make a diagnosis. Additionally important is differential diagnosis, which can be difficult for patients.
History
A list of current symptoms should be presented before the history. In this case, the term “present” indicates symptoms that have persisted for a few weeks or longer. After the presence of the current symptoms has been confirmed, the symptoms’ onset is reviewed.
When the first symptoms appeared and what was going on at the time, that is when the illness officially started. Was it the result of an accident, or chronic stress?
In order to find out whether the cause was a stretch injury to the scalene or pectoralis minor muscles that led to muscular fibrosis and brachial plexus nerve entrapment, or if a direct nerve stretch injury may have been the cause, this investigation is being conducted.
Trauma
Many patients have a history of a traumatic event, like a car accident, fall on ice, slippery floor, or downstairs. Patients should be asked about their profession, exercise routines, and participation in sports in the absence of a history of an accident in order to identify potential risk factors for repetitive stress injury (RSI). Multiple symptoms of RSI exist. Well-known RSI causes include using keyboards or production lines.
Sports that require lifting or throwing motions can potentially cause RSI. However, this RSI also contributes significantly to NPMS and not just NTOS. Repetitive arm and shoulder movements are the typical etiology of NPMS because the pectoralis minor muscle joins to the coracoid process of the scapula. This is especially valid for adolescents and young adults who take part in competitive sports. Swimming, baseball (particularly pitchers), volleyball, weightlifting, and other sports that involve scapular retraction and pectoralis minor muscle (PMM) stretching have all been linked to NPMS.
If there were previous problems or symptoms that were comparable to those of the current condition, that information should be included in the history. This includes previous injuries or surgeries performed for symptoms that are similar.
Nerve Injury
It’s important to keep in mind when symptoms start to appear after an injury. Paresthesia and/or weakness that develops right away after an accident may be caused on by spinal cord shock or brachial plexus nerve strain injuries. Spinal shock was the most likely diagnosis if the nerve symptoms disappeared within the first few days. Damage to the direct nerves is likely if the symptoms continue. As opposed to nerve damage, torn muscles causing nerve compression are the typical cause of paresthesia, which can appear days to months after an accident and typically improves over time.
Spontaneous
A small percentage of patients have no previous trauma or identified event that indicated the development of symptoms. A cervical rib or an abnormal first rib may be the cause of these patients’ symptoms. A few patients with rib abnormalities will develop symptoms themselves, though a majority of them remain asymptomatic for the rest of their lives. An uncomplicated chest X-ray or cervical spine X-ray can quickly identify this.
The advancement or regression of symptoms is decided upon when the order of symptom onset has been established. This might be connected to the current medical care. It’s critical to understand previous treatments and their outcomes before making a therapy recommendation to a patient. Physical therapy (PT) modalities that a patient has already used should be mentioned since some modalities of PT are more beneficial for NTOS and NPMS than others.
Cause and Pathophysiology
The PM muscle develops from the third, fourth, and fifth ribs’ anterior surfaces and joins the scapula’s coracoid process. The PM muscle acts as a “bridge” over the neurovascular pathways connecting the upper extremity to the thorax. The PM muscle functions as a scapula protractor, stabilizing the scapula by pulling it downward, in addition to guarding the neurovascular pathways throughout their route. Stretching of the PM muscles can occur during occupational and daily activities, and sports involving repetitive motions of the upper extremities, such as weightlifting, rowing, swimming, baseball, and volleyball. In the PM muscle, repetitive stress causes strain and myofascial trigger points, progressively shortening the muscle. These disorders could be the underlying causes of PM muscle and neurovascular compression discomfort.
Regular exercise or sports may also cause vascular PMS. During throwing and powerful overhead motions of the upper extremity, the PM muscle itself may compress portions of the veins or the head of the humerus may apply pressure on the vascular systems. Additionally, repeated compression causes intimal damage and thrombosis to follow. Due to the pressure caused by the pressure on the nerves caused by the proximity of nerves to vascular structures, it generally comes with neurogenic PMS symptoms. Acute traumas, car accidents, and hyperextension neck injuries like whiplash might also contribute to the etiology of PMS. Whiplash injuries have a complicated pathophysiology, and then reflex muscle spasms in the surrounding tissues are possible.
Scalene or PM muscles that are very tight all the time can compress the neurovascular bundle, resulting in TOS symptoms. Following a whiplash injury, patients were asked to look into the involvement of myofascial trigger points in the PM muscle. Myofascial trigger points in the PM muscle indicated TOS symptoms and all complaints decreased after conservative therapy.
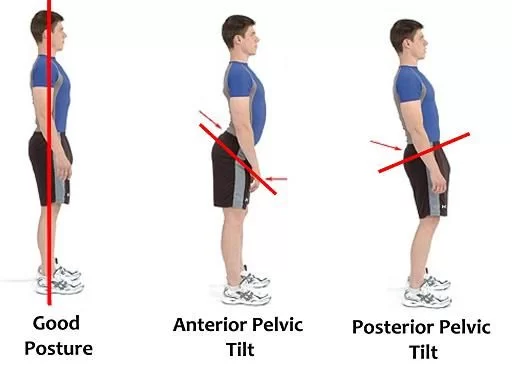
An important contributing factor to the pathogenesis of PMS is postural problems. Shortening of the pectoral muscles, protraction of the head, and elevation and protraction of the shoulders are all symptoms of the upper crossed syndrome. Due to the rise in desk-bound jobs and the usage of mobile phones, this syndrome has recently become more prevalent. One of the most important things to keep in mind is that none of these ailments only affect the pectoral muscles.
Paraspinal muscles, close muscles, and shoulder joint stabilizers may all be affected. All of the cervical and periscapular muscles can develop myofascial trigger points, therefore each one must be examined to determine the best course of action.
Spasticity is an additional factor in PMS. Upper motor neuron lesions that affect the upper extremities and cervicothoracic area might cause spasticity in PM muscles. A hemiplegic patient with upper extremity flexor spasticity caused on by a stroke has been diagnosed with PMS. Botulinum toxin (BTX) injections in the PM muscle under ultrasound (US) guidance helped the patient recover. The fourth and fifth fingers of the affected upper extremities are numb, tingling, and weak due to PMS. Pressure applied to the PM muscle aggravated the symptoms, and they confirmed the PMS diagnosis.
Symptoms of Pectoralis Minor Syndrome
The typical symptoms include pain, numbness and/or tingling, and weakness.
Pain
According to a patient’s statement of the pain’s quality, the locations of the pain are more useful in the diagnosis. The divide between “nerve” and “muscular” pain may occasionally be helpful, but it rarely matters. In NTOS, occipital headaches and neck pain are frequent. Strongly suggestive of NPMS is discomfort or swelling in the axilla and the anterior chest wall right below the collarbone. In both of these disorders, pain in the shoulder, upper arm, and forearm is common.
Paresthesia
Over 90% of NTOS and NPMS patients have paresthesia. All five fingers are typically affected, however, the 4th and 5th fingers in the ulnar nerve distribution are frequently where it is most severe.
Weakness
In contrast to pain and paresthesia, weakness is usually observed. Dropping objects and having weak grips are indicators of weakening.
Other symptoms can include:
- Pectoral Muscle Pain – Chest pain
- Shoulder pain
- Small and ring finger ache, inner elbow pain, and inner arm pain.
- redness or swelling in your hand or arm
- Your hand looks slightly bluish.
- a sensation of weightiness in your hand or arm
- Easily fatigued arms and hands
- Superficial vein distention in your hand
- Your hand-grip muscles are losing away and becoming weaker.
- Difficulty with hand-fine coordination
Clinical presentation
According to reports, the symptoms have lasted a long time because of the slow diagnosis. Knowing the symptoms and warning signs of PMS well is essential to prevent ignoring the syndrome. With pain in the arm, shoulder, neck, chest, and scapular area as well as weakness, paresthesia, edema, and coldness in the upper extremity, there is a wide range of clinical presentation. The age range of the patients is another important factor to consider. Every age and gender may have symptoms of pectoralis minor syndrome. When children exhibit PMS symptoms, playing sports and trekking should be questioned.
In all upper body regions, including the chest, neck, and upper extremities, pain is frequently the first symptom to be experienced. Pain in the supraclavicular area, anterior chest wall, scapular part, and shoulder toward the arm and hand are common complaints from patients. Most people can experience chest pain, which occasionally looks like angina symptoms.
In the majority of cases, a decrease in cervical lordosis is seen. Occipital discomfort can be associated with neck and chest pain in people with PMS. Clinically, neck pain and headache are more severe when BP branches are stuck above the collarbone.
In PMS, shoulder pain also occurs rather frequently. There may be pain in the upper arm, including the rhomboid, trapezius, and shoulder girdle muscles. Other common symptoms include paresthesia, tingling, and numbness. Despite the fact that the fourth and fifth fingers frequently have paresthesia, the entire hand may experience problems. In chronic illnesses, weakness and muscle atrophy are common. It is possible to observe hand weakness, such as dropping objects and weak control.
Due to the close proximity of the BP branches to the AA and AV, neurological symptoms are common in vascular entrapment, but it differs from pure neurogenic entrapment in some ways. Discoloration, swelling, discomfort, and heaviness of the affected arm are common symptoms of venous PMS. The chest wall or upper arm’s venous collaterals are visible. In addition to the AV being compressed under the PM muscle, the subclavian vein can also be restricted to the costoclavicular area.
Therefore, these two areas must be taken into account for entrapment whenever there is a venous blockage. Blood flow to the extremities is reduced as a result of axillary artery stenosis caused by PMS. Exercise-induced fatigue is a warning indication of AA stenosis. Digital ulcerations are a sign of development, as are arm claudication and eventually discomfort, numbness, and freezing. Non-thrombotic blockages cause intermittent symptoms, which are more noticeable while the extremity is elevated and go away when the extremity is at rest. When thrombosis occurs, the symptoms are more severe and prolonged, lasting for days or weeks. The necessity of a pulse check cannot be overstated, and it is best to collect objective hemodynamic data while positioning the arms to simulate probable ischemia symptoms.
Physical Examination
Pathologies that result in neurogenic compression in various upper extremity regions frequently produce pain, paresthesia, and weakness. The ulnar nerve is entrapped at the elbow, the median nerve is compressed at the wrist and in the pronator muscle, and the upper extremity neurovascular structures are compressed in the inter scalene triangle, the costoclavicular, and the retro pectoral area.
Nerve entrapment symptoms frequently resemble one another. To find painful spots and positive Tinel signs, a physical examination should therefore include palpation and a Tinel test at the aforementioned potential entrapment locations. By palpating and applying pressure on the pectoral muscles, the symptoms become aggravated if the neurovascular structures are trapped under the PM muscle.
When PMS is present, pain frequently happens with shoulder abduction and retraction. Positive outcomes are sometimes obtained from subacromial impingement maneuvers like the Neer and Hawkins tests. The patient may have subacromial impingement syndrome (SIS), which has been misdiagnosed, along with these physical examination findings and shoulder pain. Despite not being adequate for a conclusive diagnosis of SIS, shoulder impingement tests are crucial for clinical evaluation. The conclusive diagnosis of SIS can be made with a subacromial injection test. Additionally, PMS may come with SIS. According to PMS, subacromial impingement tests were positive in 66.6% of the patients and subacromial injection tests were positive in 33.3% of the patients.
Subacromial impingement syndrome may be connected to the shoulder impingement and PMS caused by overuse injuries to the shoulder muscles. The degradation of shoulder biomechanics caused by the shortened or constricted PM muscle is another factor. A subacromial injection test may be applied to rule out SIS in such painful conditions.
It is important to properly assess the cervical area as well. It is important to rule out cervical radiculopathy and supraclavicular entrapments. Because the symptoms of PMS and cervical radiculopathy are similar, PMS cases are sometimes mistaken as cervical radiculopathy. An electrodiagnostic test was recommended for a case with neck pain, numbness in the upper extremities, and positive magnetic resonance imaging (MRI) results of cervical disc herniation. Regarding cervical radiculopathy, the electrodiagnostic examination was unremarkable. An initial diagnosis of TOS was made after re-evaluation with provocation maneuvers and the reproduction of symptoms by applying pressure to the PM muscle. A diagnostic injection test verified the new final diagnosis of PMS.
Vascular diseases are characterized by swelling, redness, cyanosis, and coldness in the hand and full arm. Check the radial and ulnar pulses. Provocation tests should be included in the physical examination because they can be useful for diagnosing TOS and PMS. These tests, however, should not be regarded as conclusive proof of PMS or TOS on their own. The compression of neurovascular structures at the entrapment location serves as the foundation for the provocation testing.
Adson’s test, costoclavicular maneuver, neck rotation test, and head tilt test are all used to determine whether the neurovascular bundle is entrapped supraclavicularly. In patients with pure PMS, the physical examination typically results in weak or no responses to these maneuvers.
Wright’s test, the patient’s upper extremity is moved backward into abduction and extension as the examiner feels the radial pulse’s intensity. The arm can be abducted and the forearm can be flexed as an alternative position for Wright’s test. When the radial pulse decreases and the symptoms increase, the test is said to be positive.
Another important test for PMS is the upper extremity tension test. Three steps are taken to complete this test: First, the arms are raised to 90 degrees parallel to the floor with the elbows extended.
The wrists are in the second position, which is dorsiflexion.
The third position involves angling the shoulders and head to either side. If there is BP compression, this procedure immediately causes pain and paresthesia. Another provocation test for PMS is a 90° abduction or elevated arm stress test, sometimes referred to as the Roos test. The patient waits for three minutes while holding both arms in 90° abduction and external rotation. It is necessary to flex and extend the fingers of the hand.
Diagnosis
Due to its uncommon inclusion in a doctor’s differential diagnosis, pectoralis minor syndrome is frequently disregarded. Therefore, it is unknown how frequently PMS actually occurs in people who have symptoms of upper extremity discomfort and paresthesia. For a treatment to be successful, a proper diagnosis is required. To pinpoint the site of the compression of neurovascular structures and distinguish it from disorders with similar symptoms, a thorough history and physical examination are essential. Patients should be questioned about their jobs, hobbies, and exercise routines to identify the root cause of repetitive stress and injury.
Electrodiagnostic
Electromyography (EMG)
In most NTOS and NPMS patients, EMG is said to be normal. The medial antebrachial sensory cutaneous nerve was measured for the first time. Normal ranges and this technique were created. The vast majority of patients who underwent surgery for NTOS and NPMS had good results from this test.
Stimulation of the C8 Nerve Root
Although it is extremely useful, this test is rarely utilized because it hurts more than most other ways to assess nerves. It is carried out by directly stimulating the C8 nerve root in the back of the neck, just outside the cervical spine. It gauges the amount of time it takes for the C8 nerve root to reach a chosen location in the arm or neck.
To show structural lesions, computed tomography (CT) and magnetic resonance imaging (MRI) are helpful. An easy and affordable approach to determine whether a first rib is cervical or abnormal is to take an anterior-posterior and lateral X-ray of the cervicothoracic area. In cases when supraclavicular entrapment is suspected, this discovery is important. The usual lordotic neck curve may also be seen straightening in the lateral view. In cases with cervical vertebra issues, PMS, and TOS, a reduction in cervical lordosis may be beneficial. However, in the majority of PMS cases, an MRI of the BP indicates normal anatomy rather than signs of nerve compression. This imaging method provides insightful data for spinal or foraminal stenosis and herniated cervical discs.
Electromyography and nerve conduction are two examples of electrodiagnostic equipment. The diagnosis of TOS is supported by the decreased amplitude of medial antebrachial cutaneous nerve and ulnar nerve sensory nerve action potentials. It is impossible to distinguish between the compression at the scalene triangle and the PM space when an electrodiagnostic test for BP involvement is positive. Additionally, even if the patient exhibits neurological symptoms, the majority of electrodiagnostic findings in people with neurogenic PMS and TOS are within the normal range. These patients were previously given the disputed neurogenic TOS diagnosis. Patients with characteristic TOS symptoms and provocation tests producing TOS symptoms were given the clinical diagnosis of disputed neurogenic TOS. Clinical criteria and diagnostic injections have recently become more significant in the diagnosis of TOS and PMS.
The presence of three of the following four criteria, as determined by the most recent criteria, defines neurogenic TOS/PMS:
- The scalene triangle in the case of TOS and the pectoralis muscle site in the case of PMS, as well as pain on palpation of the region that is affected, are symptoms that are consistent with irritation at the site of compression.
- Numbness, discomfort, paresthesia, vasomotor abnormalities, and weakness (with muscle wasting in severe cases) are all symptoms of brachial plexus compression.
- absence of further diagnoses that could have been made (brachial neuritis, shoulder disease, carpal tunnel syndrome, chronic regional pain syndrome, and cervical disc disease)
- a successful injection test.
Electrophysiological testing can be requested to rule out neurological diseases such as cervical disc herniation, ulnar and medial nerve entrapments, brachial plexopathy, and polyneuropathies.
Using specific, sensitive test methods, electrodiagnostic can identify minor median nerve entrapments at the wrist and ulnar nerve entrapments at the elbow. High-frequency US can also be utilized to accurately diagnose entrapment neuropathies. For diagnosing peripheral nerve entrapment, it is important to consider the cross-sectional area of the nerve at the thought location, its echostructure, its instability in a dynamic US scan, and the pain response to nerve compression with a US examination.
The non-invasive subclavian and axillary artery and vein Doppler US examination demonstrates dynamic maneuvers that compress vascular systems in real-time. In unsure circumstances, dynamic venography and arteriography are diagnostic. MR/CT angiography can be used to diagnose arterial or venous TOS and PMS, and magnetic resonance neurography can be utilized to visualize blood pressure. Finger plethysmography and pulse oximetry are two examples of hemodynamic testing that may be a valuable, non-invasive, quick, and affordable clinical tool for identifying TOS. It demonstrates upper extremity hypoperfusion during stimulating activities or exercise.
Diagnostic injection tests
When a diagnosis is suspected based on clinical signs, diagnostic injection tests such as scalene muscle and PM muscle blocks are used to confirm the diagnosis. To create the best treatment plan, locating the neurovascular compression is essential. After each muscle block, the physical examination and provocation tests are performed, and the degree of improvement in symptoms such as pain, soreness, numbness, and weakness is noted. Muscle injections used for diagnosis should make use of ultrasound.
Pectoralis minor muscle block
Performing a PM muscle block is necessary to diagnose PMS. After 30 to 40 minutes following injection, considerable symptom alleviation and a reduction of soreness across the PM muscle are considered excellent responses. The US-guided block is dependable, practical, and affordable, and it enables visualization of neurovascular structures to reduce risks. The patient is positioned supine throughout the treatment. The infraclavicular area is the location of the US probe. On the pectoral region, the pectoralis major muscle, PM muscle, AA artery, and AV can be seen. The in-plane approach allows for the visualization of the needle during injection. Recognition of anatomical differences, PM thickness, and relationships with neighboring structures are all made possible through assessment.
In diagnostic blocks, a 4 mL dose of 1% lidocaine short-acting local anesthetic is frequently utilized. The in-plane approach is used to administer the injection, which uses a linear probe at a 45° angle to the region of greatest tenderness. The size of the needle used depends on the depth of the muscle. If symptoms and indications improve after the injection, the diagnosis of PMS is verified, and the scalenus anticus (SA) block is skipped. This approach is preferred for the diagnosis of TOS. If the indications or symptoms continue, an SA block is administered and the physical examination is redone.
Scalenus anticus muscle block
The patient is positioned against a wall with their back. Initially, a linear US probe is used to detect supraclavicular blood pressure. The interscalene region is then visible as the probe is pointed cephalad. The jugular vein and carotid artery can be seen, together with the BP at the level of C6 and the nearby SA. As the needle is inserted into the SA’s body, it is visualized either out-of-plane or in-plane (medial to lateral or lateral to medial). Lidocaine 1% is injected into the SA under real-time imaging after negative aspiration to make sure the injection fluid stays inside the muscle.
Differential Diagnoses for PMS:
Rotator cuff tear: This is a tear in one or more of the tendons that attach the muscles of the rotator cuff to the humerus (upper arm bone). Four muscles make up the rotator cuff, which aids in stabilizing the shoulder joint.
Bursitis: This is inflammation of a bursa, which is a small fluid-filled sac that cushions bones, tendons, and muscles. There are several bursae in the shoulder joint, and inflammation of any one of them can cause pain and discomfort.
Tendonitis: This is inflammation of a tendon, which is a cord of tissue that connects muscle to bone. There are several tendons in the shoulder joint, and inflammation of any one of them can cause pain and discomfort.
Arthritis: This is inflammation of a joint. The shoulder joint can be affected by different types of arthritis, including osteoarthritis, rheumatoid arthritis, and psoriatic arthritis.
Cervical radiculopathy: This is a condition in which a nerve root in the neck is compressed or irritated. This can cause pain, numbness, and tingling in the shoulder, arm, and hand.
Thoracic outlet syndrome: This is a condition in which the nerves and blood vessels that pass through the thoracic outlet (the space between the collarbone and the first rib) are compressed. This can cause pain, numbness, and tingling in the shoulder, arm, and hand.
Treatment of Pectoralis Minor Syndrome
Nonoperative Treatment
The most effective treatment route is conservative when there are no venous or arterial thromboses. Early diagnosis and treatment are important. Activity regulation and activity modification are the two most critical therapeutic components. The majority of patients respond well to non-operative care.
Physical therapy, rehabilitation, and pharmaceutical treatments such as analgesics, muscle relaxants, and anti-inflammatory medications make up non-operative management.
The foundation of conservative treatment is a rehabilitation program that includes shoulder stability, postural correction, and stretching of the PM muscles. A home-based self-treatment approach that is personalized for each patient is taught to them. The keys to a successful treatment are good posture and PM muscle stretching exercises. It is essential for managing PMS and needs to be suggested to all people with the condition.
PMS is initially treated non-operatively, with a priority on posture correction and stretching of the periscapular muscles. The aim is to retrain scapular mechanics and scapulohumeral rhythm while increasing PM length and flexibility. The coracoid insertion is relocated farther from the anterior rib origin in order to lengthen and stretch PM. There are examples of specific procedures, and additional workouts to retrain scapular kinematics are also included.
By keeping shoulders in passive retraction, orthotic bracing (figure eight) can be used for treating chronic scapular protraction. Brace with a figure-8 design. For the purpose of preventing resting scapular protraction, the brace continuously applies posterior pressure on the scapula. This helps with postural retraining and eliminates compression caused by a protracted scapular position in the retropecotalis minor region.
Center spine towel roll stretch. When the patient is lying supine with a towel rolled between their shoulder blades, the anterior shoulders, chest, and pectoralis muscles are stretched by allowing the scapula and shoulders to migrate posteriorly.
Corner stretch. The patient stands facing the wall with the opposite foot forward and the arm externally turned 90 degrees. In order to stretch the pectoralis muscles, the anterior shoulder, and the chest, the patient moves their body away from the wall.
Butterfly stretch. The patient is positioned between their shoulder blades on a foam roller or towel that has been rolled up. Stretch starts with arms outstretched to the sides and gradually goes to an overhead position by abducting the arms in controlled movements.
Wall Wash. The patient presses a folded towel against the wall, pushing it horizontally up and forward with extended scapulae before reversing the motion downward and in extension with contracted scapulae.
Scapular retraining exercises. performed while upright, arms raised in front of you, and hands forced up against a wall. Scapular elevation and depression. Retraction and protraction of the scapula.
Stretching exercises for the scapula. Supine shoulder flexion stretches with a stick in both hands allow the healthy arm to help the impaired arm achieve maximum overhead flexion stretch.
External rotation stretching is done while supine so that the opposing arm can help achieve the maximum external rotation stretch for the anterior shoulder structure. Stretching the posterior shoulder structure while sleeping is done in the lateral decubitus position.
Different stretching methods for PM lengthening have been described with varying degrees of success.
A unilateral self-stretch was determined to be superior to a supine or sitting manual stretch after testing three distinct methods. PM lengthening also results in increased posterior scapular tilting and upward scapular rotation after stretching. Active patients who underwent scapular retraining and stretching experienced improvements in shoulder function, discomfort, and scapular posture.
A stretching exercise at home every day helps patients with shoulder pain work better and have much less pain, according to research on the effects of stretching on PM muscle function, muscle length, and scapular kinematics in individuals. Standing in an open doorway with the hands at shoulder level resting on the door jambs is an effortless approach to stretch PM muscles. Three times a day, three times every session, seven days a week, patients are advised to stretch, hold each stretch for 15 to 20 seconds, rest for the same amount of time, and repeat. For two to three months, this should be done.
Patients participate in the physical therapy and rehabilitation program even if they are unable to perform the exercises properly or if they do not gain enough from them. In each session, the pectoral region and shoulder girdle can receive therapeutic US, traditional transcutaneous electrical nerve stimulation, or hot packs. The therapist gently stretches the shortened shoulder girdle, cervical muscles, and pectoral and scalene muscles. Exercises for post-isometric relaxation and shoulder proprioceptive neuromuscular facilitation are also beneficial.
If necessary, local anesthetic injections or dry needling of the PM muscle can be done; corticosteroid injection is not advised. Injections of BTX into the muscles reduced muscle spasms by preventing the release of acetylcholine at the neuromuscular junction, which is a frequent treatment for localized spasticity. Adductor spasticity and PMS symptoms were noted in a case of hemiplegia with upper extremity spasticity caused by a stroke. BTX injections in the PM and pectoralis major muscles, as well as the subscapularis and latissimus dorsi muscles, revealed symptoms. Injections of botulinum toxin can be used to target muscle relaxation in cases of resistance and spasticity. An observational cohort study of PMS patients who had BTX injections in the PM muscle under US guidance indicated good results of symptom relief in patients without spasticity.
Kinesio taping (KT) applications have become very popular recently for relieving muscular tension and releasing fascial stress. According to research on KT of the PM muscle, KT of the shoulder combined with stretching of the PM muscle considerably improved the length of the PM muscle and significantly lowered the measurement of rounded shoulders when lying flat.
Surgical Treatment
The results of pectoralis minor stretching are currently effective. Many people with NPMS as their primary diagnosis have seen significant progress after only one or two months of stretching. These patients are still progressing well. These people exhibited symptoms for a shorter period of time than a year. Patients halted the repetitious behavior that had caused their symptoms as part of their treatment. They were able to resume that activity afterward, though with reduced intensity.
Pectoralis minor tenotomy with partial myomectomy is the surgical procedure. Either a thoracic or transaxillary technique can be used to perform this. In to thoroughly excise the clavipectoral fascia and any bands or accessory muscles, such as Langer’s axillary, we prefer the transaxillary method because it allows for a greater exposure arch, around the axillary neurovascular bundle.
A 4–7 cm transverse incision is made starting from the anterior axillary fold through the axilla, 1-2 cm above the bottom of the axillary hairline. The pectoralis minor muscle can be identified by its connection to the coracoid process from the pectoralis major muscle, which is retracted. To prevent the muscle from reconnecting with the brachial plexus, the pectoralis minor origin is separated at the coracoid and a 1-2 cm portion of the detached muscle end is removed. The lateral pectoral nerves leading to the pectoralis major are protected with care. These nerves pass through the pectoralis minor, and cutting them causes the pectoralis major to atrophy. The clavipectoral fascia, any bands, and any muscle fibers are removed after closure to release the neurovascular bundle from any compressive tissue.
The pectoralis muscle’s remaining body attaches to the anterior chest wall after surgery. For two to three months following surgery, the patient should stay away from raising their arm above shoulder level to help them stick to this regimen. To prevent a frozen shoulder, the patient should raise the arm 180 degrees once daily.
Post-operative physiotherapy treatment
Postoperative protocol: Under the direction of a therapist, an early range-of-motion and targeted stretching program is started. A figure-of-eight brace is also used to correct the extended resting scapular position. Comprehensive PM stretching, posture retraining, and scapulohumeral rhythm retraining are all part of these procedures. Between 4 and 6 weeks after surgery, aggressive periscapular muscle strengthening begins. By 3 to 4 months after surgery, the majority of patients are able to resume overhead activity, including sports. During recovery, core, hip, and lower extremity strengthening and coordination are strictly focused on.
Patients are given a sling to wear as comfort during the first day or two following the surgical release of the PM tendon. At the end of the second postoperative week, sutures are removed, and motion and strength exercises in physical therapy are started. Strengthening and coordinating the periscapular muscles is given special focus.
In individuals with a painful static prolonged scapula or throwing athletes with recalcitrant dyskinesis, the arthroscopic PM release is typically an additional surgery. The regular rehabilitation and return to throw postoperative regimen shouldn’t be altered by the PM’s release. Any dyskinesis rehabilitation must include periscapular control and strengthening. Paying close attention to your balance, hip and lower extremity mobility, and core strength is also important.
Weeks 0-2
Phase 1: Immobilization -Simple sling immediately postoperatively-Transition to Figure-of-Eight brace at the first postoperative visit and active elbow, wrist, and hand motion
Weeks 2-6
Phase 2: Range of motion and scapula retraining -Progress from passive to active assisted to active shoulder motion-Periscapular strengthening, retrain scapular kinematics, and pectoralis minor stretching-Continue using Figure-of-Eight brace-Pool therapy encouraged
Weeks 6-12
Phase 3: Strengthening -Full active/passive shoulder movement aggressive strengthening with progression to eccentric strengthening-Continue postural retraining and scapulohumeral rhythm kinematics, continue the use of Figure-of-Eight brace
Weeks 12-16
Phase 4: Sport and activity specific -Continue Phase 3 therapy use of Figure-of-Eight brace-Gradual return to sport and activity
Conclusion
Pectoralis minor syndrome (PMS) is a rare condition that causes compression of the neurovascular bundle at the retro pectoralis minor space. This can lead to a variety of symptoms, including pain, numbness, weakness, and swelling of the upper extremity.
PMS is most commonly caused by repetitive overhead activities, such as those performed in certain sports or jobs. It can also be caused by trauma, congenital abnormalities, or spasticity of the pectoralis minor muscle.
The diagnosis of PMS is based on a detailed history and physical examination. Imaging studies, such as ultrasound or MRI, may be used to confirm the diagnosis and rule out other causes of the patient’s symptoms.
Conservative treatment is usually the first line of therapy for PMS. This may include physical therapy, stretching exercises, and massage. If conservative treatment is not effective, surgery may be recommended to release the pectoralis minor muscle.
Overall, the prognosis for PMS is good. Most patients respond well to conservative treatment. Most of the time, surgery is only required in a tiny proportion of situations.
PMS is an overlooked syndrome that is easily overlooked and confused with other painful neurovascular compression syndromes of the upper extremity. The foundation of the diagnosis is a thorough history, physical examination, and diagnostic principles. Conservative treatment is usually successful, and surgical treatment should be considered in unresponsive cases.
FAQs
Which nerves control the pectoral muscles?
Lateral Pectoral Nerve C5. The pectoralis major and minor are supplied by the pectoral nerves. The largest of the two pectoral nerves, the lateral pectoral nerve originates from the fifth through seventh cervical nerves (C5-C7). It comes from the lateral cord or the upper and middle trunks’ anterior divisions.
Can breast pain be caused by pectoral muscle?
Additionally, according to experiencing muscle-like soreness, it’s probably due to a torn chest muscle. “Breasts are mostly fat and veins, but they’re resting on a muscle,” Your pain may be coming from your pectoralis major muscle in particular.
What other names are given to the pectoralis minor?
Your chest contains a little, flat, triangular muscle called the pectoralis minor. The muscle also referred to as the “pec minor,” is situated below its counterpart, the “pectoralis major,” and it moves your shoulder blade and ribs.
What condition causes the pectoralis major to be absent?
The sternocostal head of the pectoralis major muscle is one of the anatomical abnormalities that make up Poland syndrome, along with other diverse presentations such as hypoplasia or absence of the minor muscle and digital anomalies like syndactyly.
How is the pectoralis minor nerve controlled?
pectoral nerve in the middle
Before obtaining a connecting branch from the lateral pectoral nerve, the medial pectoral nerve rises behind the axillary artery and turns forward between the axillary artery and the vein. The medial pectoral nerve passes into the pectoralis minor muscle and emerges as a number of branches that supply the power.
References
Abdallah, M. H., Wehbe, M. R., Elias, E., Kutoubi, M. A., & Sfeir, R. E. (2016). Pectoralis Minor Syndrome: Case Presentation and Review of the literature. Case Reports in Surgery, 2016, 1–3. https://doi.org/10.1155/2016/8456064
Donahue, D., & Auchincloss, H. (2020). Thoracic Outlet Syndrome, An Issue of Thoracic Surgery Clinics, E-Book. Elsevier Health Sciences.
Illig, K. A., Thompson, R. W., Freischlag, J. A., Donahue, D. M., Jordan, S. E., Lum, Y. W., & Gelabert, H. A. (2021). Thoracic Outlet Syndrome. Springer Nature.
Kaye, A. D., & Shah, R. V. (2014). Case studies in pain management. Cambridge University Press.
Sanders, R. J., & Annest, S. J. (2014). Thoracic outlet and pectoralis minor syndromes. Seminars in Vascular Surgery, 27(2), 86–117. https://doi.org/10.1053/j.semvascsurg.2015.02.001
Sanders, R. J., & Annest, S. J. (2017). Pectoralis minor Syndrome: subclavicular brachial plexus compression. Diagnostics, 7(3), 46. https://doi.org/10.3390/diagnostics7030046
Sanders, R. J., Annest, S. J., & Goldson, E. (2013). Neurogenic thoracic outlet and pectoralis minor syndromes in children. Vascular and Endovascular Surgery, 47(5), 335–341. https://doi.org/10.1177/1538574413481858
Sanders, R. J., & Rao, N. (2010). The Forgotten Pectoralis Minor Syndrome: 100 operations for Pectoralis minor syndrome alone or accompanied by neurogenic thoracic outlet syndrome. Annals of Vascular Surgery, 24(6), 701–708. https://doi.org/10.1016/j.avsg.2010.02.022



2 Comments