Hip Fracture
Introduction
Hip fractures are one of the most frequent fractures presented to the emergency department and orthopedic trauma teams. No difference exists between a “hip fracture” and a “neck of femur fracture.”Both terms describe a fracture of the proximal femur between the femoral head and 5 cm distal to the lesser trochanter.
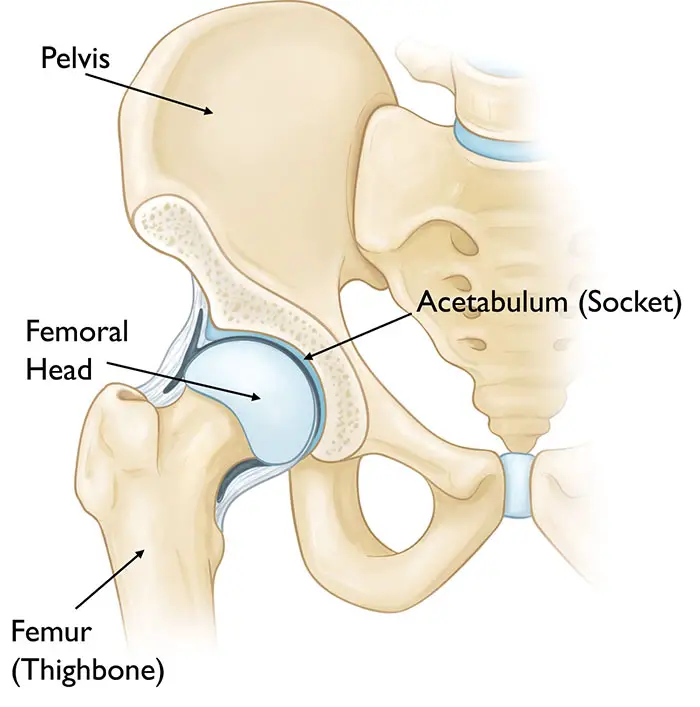
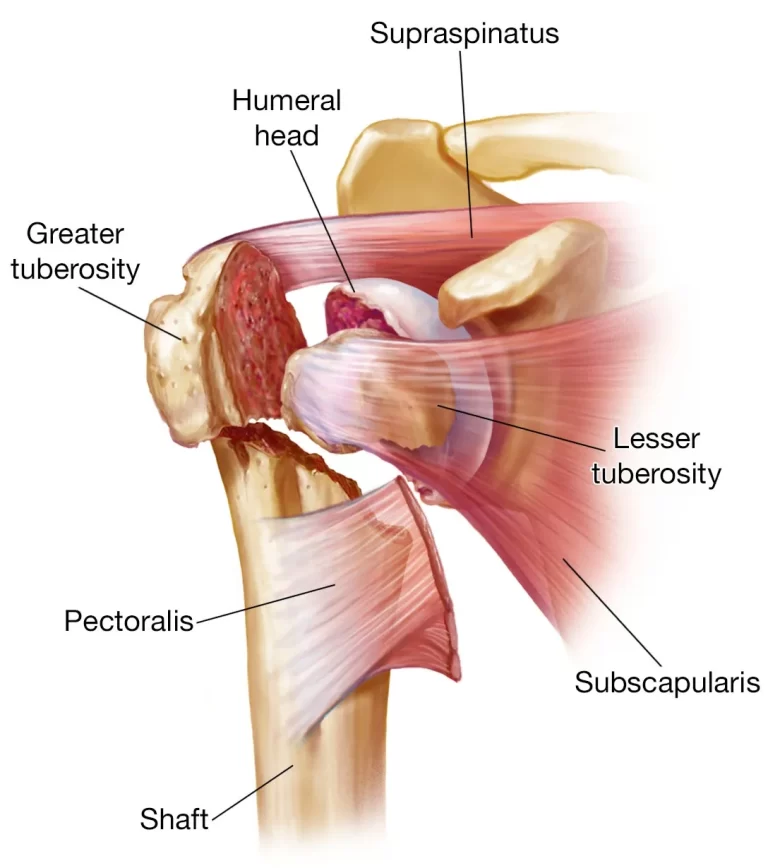
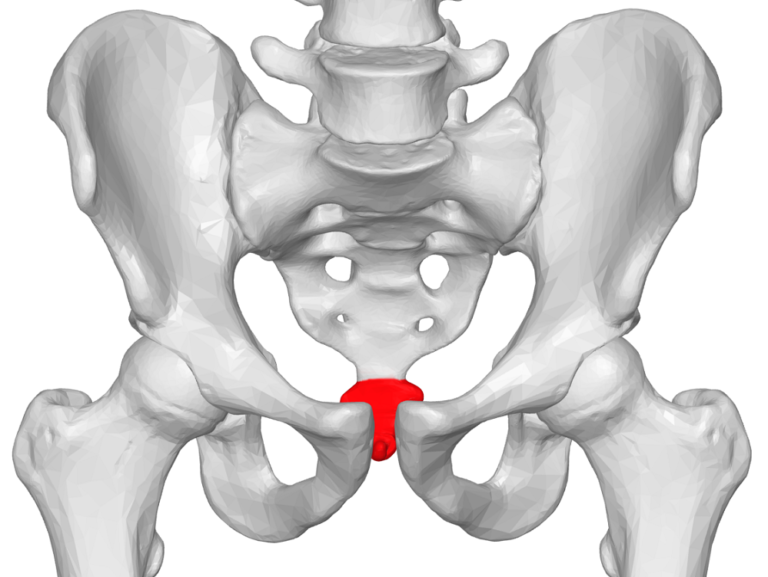
Anatomy
The hip is a ball-and-socket joint. The ball is the head of the femur, the upper part of the thighbone. The socket is called the acetabulum. One component of the pelvic bone is the acetabulum. Its rounded form accommodates the femoral head.
Hip capsule
The capsule of the hip is attached proximally to the margin of the acetabulum and transverse acetabular ligament. Distally, to the bases of the greater and lesser trochanters, to the intertrochanteric line, and posteriorly to the femoral neck(1/2 inch from the trochanteric crest). The retinal vessels, which play a significant role in the blood flow to the femoral head, are located there.
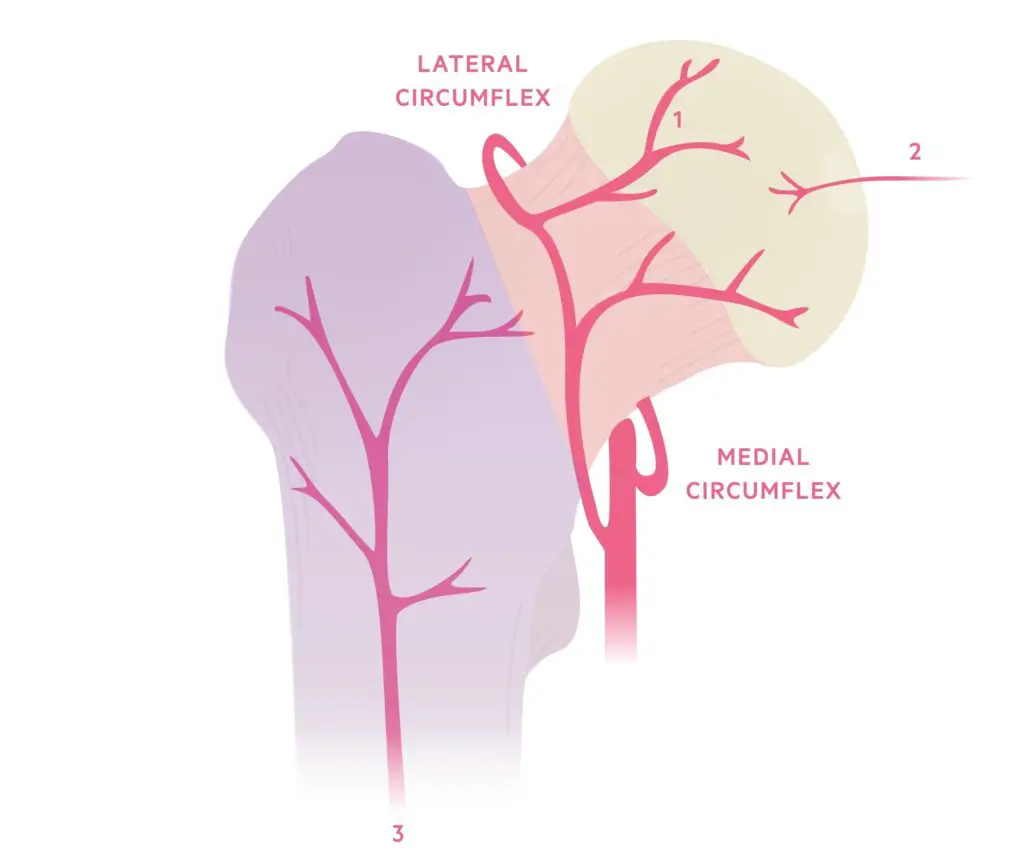
Blood supply to the femoral head
Three sources of blood supply the femoral head:
- Retinacular vessels – main blood supply. Originates from an extra-capsular arterial ring, supplied by medial and lateral circumflex vessels ( profundas femoris A) and strengthened by the internal iliac arteries (the superior and inferior gluteal arteries).
- The foveal artery – is not a major source. provides a tiny quantity of blood to the epiphysis during the development of the skeleton. believed to completely disappear in adulthood (ligamentum teres).
- Metaphyseal vessels – not a major source. Metaphysical arteries supply blood to the femoral head after skeletal maturity.
Causes
Hip fractures are most common in people 65 years of age and older, usually caused by falls. As you age, your bones naturally deteriorate and become more fragile, even from minor falls. Sports injuries, car crashes, and bicycle accidents are the main causes of hip fractures in children and young adults.
Other things that break your hip include:
- Being assigned female at birth.
- Your genetic makeup: are you tall or thin, or do you have relatives who suffered from fractures later in life?
- You are not getting enough calcium and vitamin D for strong bones.
- Staying inactive. Walking and other weight-bearing exercises maintain strong bones.
- History of smoking.
- Ailments like arthritis can impede steady and safe movement or ailments that result in vertigo or balance issues.
- Taking specific medications, such as long-term steroid medications for COPD or asthma.
Risk Factors
Age & Sex
People’s bone density and muscle mass tend to decrease with age. In addition to vision and balance issues, older adults may experience an increased risk of falls.
Women suffer hip fractures approximately three times more frequently than men do. Because menopause causes a drop in estrogen levels, which accelerates bone loss, women lose bone density more quickly than men do. But men can also experience dangerously low bone density.
Medical Conditions
The following conditions may raise your risk of hip fracture:
- Osteoporosis. Bones weakened by this condition are more prone to break.
- Thyroid problems. Fragile bones may be the result of an overactive thyroid.
- Intestinal disorders. Conditions that reduce the absorption of vitamin D and calcium also can cause weakened bones.
- Problems with balance. Peripheral neuropathy, Parkinson’s disease, and stroke can all raise the chance of falling. Blood pressure and blood sugar levels that are too low might significantly raise the risk of falling.
Certain Medications
Long-term use of cortisone medications, like prednisone, can weaken bones. Dizziness can be brought on by some medications alone or in combination, which raises the possibility of falling. The drugs that are most frequently linked to falls are sedatives, antipsychotics, and sleep aids.
Nutritional Problems
Young people’s peak bone mass is lowered and their risk of fracture later in life is increased when they don’t get enough calcium and vitamin D in their diet. To try to maintain bone density as you age, it’s also critical to get adequate calcium and vitamin D. Loss of bone mass is also increased in underweight individuals.
Lifestyle Choices
Weakened bones and muscles from not getting regular weight-bearing exercise, like walking, increase the risk of fractures and falls.
Alcohol and tobacco can obstruct the natural processes that build and maintain bone, which can lead to bone loss.
Types Of Hip Fracture
A partial or total break in a bone is called a fracture. A bone may break into multiple pieces or just one large break. The type and location of the break in the bone determine the classification of a hip fracture.
These are the most typical kinds of hip fractures:
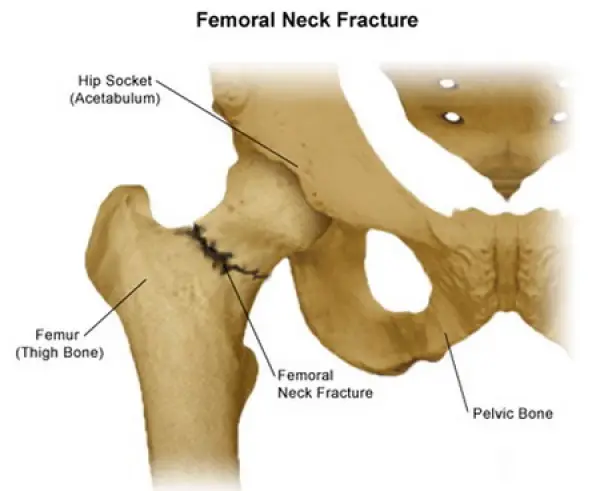
Femoral neck fracture: One to two inches away from the hip joint is where a femoral neck fracture happens. These fractures, which are linked to osteoporosis, are frequent in the elderly. Because the break typically stops the blood supply to the head of the femur, which forms the hip joint, this kind of fracture may result in complications.
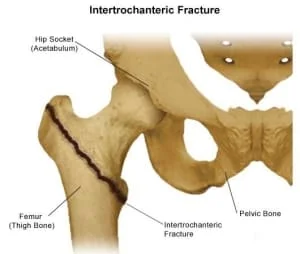
Intertrochanteric hip fracture: Three to four inches out from the hip joint is where an intertrochanteric hip fracture happens. This fracture type does not interrupt the blood supply to the bone and may be easier to repair.
Symptoms
Hip fracture symptoms usually appear suddenly. They might, however, begin softly and worsen over time. Hip fracture symptoms include:
- Pain: Usually, hip pain is severe and sharp. However, it can also be achy or mild. The majority of people experience pain in the groin, pelvis, outer hip, and thigh. Sciatica can cause pain that travels from your buttocks to your legs. You might experience knee pain as well.
- Limited mobility: Most hip fracture victims are unable to walk or stand. Walking may be feasible at times, but bearing weight on the leg causes excruciating pain.
- Physical changes: You may have a bruise on your hip. You might have one leg that looks shorter than the other. The hip might look out of position, twisted, or rotated.
Diagnosis
Physical Examination
Your hip and pelvis are examined by a physician to determine the degree of soreness, bruising, and swelling. He or she enquires as to the location and degree of your pain. Your doctor will diagnose an open fracture—a fracture where a bone protrudes through the skin—quickly and will frequently perform surgery right away.
Radiography
X-ray pictures To locate a fractured bone in the hip or pelvis, use electromagnetic radiation. They also assist your doctor in determining whether a bone has multiple fractures and whether any of the broken bone pieces have been repositioned.
CT Scans
To investigate a possible fracture pattern or determine the degree of hip joint damage, your doctor might prescribe a CT scan. A CT scan allows medical professionals to view a fracture from a variety of perspectives by using X-rays and a computer to produce two- and three-dimensional images of the hip and pelvic bones. Small bone fragments that could become lodged in the hip joint and need to be surgically removed may also be found during this test.
After reassembling a fractured bone, doctors utilize CT scans to make sure the pieces fit correctly.
MRI Scans
Your doctor might advise an MRI if they believe you have a stress fracture in your hip or pelvis that is not visible on an X-ray, or if your symptoms point to additional damage to your blood vessels, ligaments, tendons, or nerves. In this test, computerized, three-dimensional images of the soft tissues surrounding the joint are produced using radio waves and a magnetic field.
An MRI may show strained or torn tendons, ligaments, or a bone fragment pressing against a nerve. If an X-ray shows no signs of trauma but your symptoms point to a fracture, doctors may also order an MRI.
Your doctor might advise an MRI if they believe you have a stress fracture in your hip or pelvis that is not visible on an X-ray, or if your symptoms point to additional damage to your blood vessels, ligaments, tendons, or nerves. In this test, computerized, three-dimensional images of the soft tissues surrounding the joint are produced using radio waves and a magnetic field.
An MRI may show strained or torn tendons, ligaments, or a bone fragment pressing against a nerve. If an X-ray shows no signs of trauma but your symptoms point to a fracture, doctors may also order an MRI.
Bone Scans
Your doctor might suggest a bone scan if you have pain and swelling that point to a fracture but are unable to have an MRI due to an implanted pacemaker or other medical devices.
A technician will inject a tiny amount of dye into a vein in your arm to conduct this test. This dye, known as a tracer, passes through the bloodstream and gathers in the areas where your tissues and cells are mending.
A radiologist uses a specialized camera to take pictures of the tracer while scanning your body after it has been in your bloodstream for one or two hours. You might have a fracture if it gathers more in some areas of the hip or pelvis than in others.
Treatment
The goal of conservative treatments is to reduce hip pain symptoms. When compared to surgical treatment, the functional outcome is often not significantly different.
In the majority of other cases, surgery will be required to treat the broken hip. For an elderly patient who is functionally healthy, doctors will probably advise surgery to expedite healing and recovery. Hip fractures are typically treated with surgery, medication, and rehabilitation following surgery.
Non-Surgical Treatment
Maybe you don’t need surgery for your broken hip. You won’t need surgical treatment if you’ve had a fracture for a while and only saw your doctor once the bone had begun to heal. Nonetheless, it’s not a good idea to ignore a hip fracture. It could result in a serious and long-lasting disability.
Additionally, some patients might decline to have surgery. That is the role of conservative therapies. These consist of particular treatments and tools that assist in reducing pain or discomfort and averting additional harm.
Assistive Devices
Take it easy for a minimum of six weeks after suffering a hip break. Up until it heals, you must avoid demanding activities and bearing weight on the injured hip.
That does not imply that you must stay in bed all day. It would be beneficial to move around to avoid deep vein thrombosis and blood clots due to immobility. You can get around for the time being with assistive technology like a walker, crutches, or cane. These gadgets make it easy to move around without straining your hips.
Electronic And Ultrasonic Bone Stimulation
Bone stimulation is used to treat newly fractured, nonunion, or incorrectly fusing bones. Your bone can receive extracorporeal shock waves, low-intensity ultrasound, or low-electric current via a device. It’s claimed to expedite the healing process for hip fractures.
Despite the potential for reduced pain and enhanced function, an analysis of the trial revealed no appreciable results for bone healing. Further research is needed to confirm this treatment’s efficacy.
There are no known side effects of bone stimulators. Doctors advise against the treatment for children and pregnant women, though, as more clinical trials are needed to confirm bone stimulation’s safety and effectiveness in these populations.
Physical Therapy (PT)
Before and after surgery, your physician might recommend that you see a physical therapist. Exercise helps your injured bone heal more quickly by supplying it with nutrients and oxygenated blood.
Your physician and physical therapist may occasionally approve of bed rest combined with weight-bearing activities. You can learn how to do basic range-of-motion and stretching exercises from your physical therapist.
Three ways exist for you to gain from PT. It keeps your muscles from weakening in the first place. It also makes you more flexible. Thirdly, it expands your range of mobility. Your condition will determine the length and frequency of your physical therapy sessions. Seeing a physical therapist will help your hip fracture heal and maintain the strength of your muscles.
Traction
Your surgeon can stretch the muscles surrounding your fractured hip using pulleys and weights. When you are in the hospital, they are fitted and fastened to your leg. Your muscles remain in place while the fracture heals thanks to the traction. In some circumstances, such as those involving intertrochanteric fractures (see below), this kind of non-surgical hip fracture treatment is used.
Surgical Treatment
Your femur or thigh bone, which together make up your hip joint, is housed in a socket in your hip bone. There are three fracture sites, with the femur being the most common. There are various surgical techniques for treating various kinds of fractures.
Intracapsular fracture: A fracture at the femur’s neck or ball. Another name for this is a femur neck fracture. Options for surgery include:
- Internal fixation: Your surgeon will use pins, screws, and a metal plate that runs down your femur to hold the fractured femur together while it heals if you have a displaced femoral neck fracture.
- Hemiarthroplasty: Partially replacing a hip or joint is called hemiarthroplasty. Your surgeon may choose to remove the ball of your fractured femur and replace it with a metal one if the damage is limited to the end of the bone. For patients with additional medical conditions or those who do not live independently, surgeons typically advise a partial hip replacement.
- Hip replacement: Unlike hemiarthroplasty, a total hip replacement, or arthroplasty, involves the hip socket. By fusing an artificial socket into your hip, your surgeon reconstructs your joint. After that, a ceramic or metal ball that fits the artificial socket is used to replace the damaged femoral ball.
Total hip replacement is the gold standard for treating hip fractures in otherwise healthy, self-sufficient patients.
Intertrochanteric fracture – An interruption between the greater and lesser trochanters of the femur’s neck is known as an intertrochanteric fracture.
Subtrochanteric fracture: An unusual fracture at the femur’s lower trochanters.
The gold standard procedure for treating subtrochanteric fractures is internal fixation. To fasten an intramedullary nail or long pin, your surgeon will use screws. According to a study, the length of your hospital stay and surgery reduces the likelihood of failure.
Complication
A hip fracture can lead to serious complications. Veins can clot with blood, usually in the legs. A clot may fragment and end up in a blood vessel in your lung. A pulmonary embolism, as this obstruction is known, can be lethal.
Additional issues may consist of:
- Pneumonia
- Muscle atrophy (wasting of muscle tissue)
- Postoperative infection
- Nonunion or improper union of your bone
- Mental deterioration after surgery in older patients
- Bed sores from staying still and moving very little
Prevention
- Eating right: Calcium and vitamin D-rich diets help build stronger bones.
- Getting regular checkups: See your doctor about bone density tests that identify osteoporosis symptoms. Medication called bisphosphonates, which strengthen and slow bone loss, may be suggested by your doctor.
- Preventing accidents: Remove any potential fall hazards from your house, such as throw rugs. Exercise caution when utilizing stairs or strolling on icy surfaces. Consult your healthcare provider about maintaining your body and preventing falls if you have Parkinson’s disease.
- Staying healthy: Don’t smoke, keep your weight in check, and limit your alcohol intake.
FAQs
How do you care for a fractured hip?
Your doctor might suggest that you avoid bearing any weight on the fractured hip for at least six weeks following a hip or pelvic fracture. The bone can mend as a result. To assist you in moving around, your doctor may provide you with a wheelchair, walker, cane, or crutches.
What should you avoid after a hip fracture?
To lower the risk of dislocation following a total hip replacement, you need to adhere to these precautions for a full year following the procedure: Avoid crossing your legs, flexing your hips past 90 degrees, and twisting, swiveling, and pivoting on the leg that is being operated on.
Can a broken hip heal without surgery?
Surgery is usually used to treat hip fractures. Your doctor will create a customized treatment plan based on the location and stability of the fracture, taking into account your age, physical condition, and medical history. If a non-surgical course of treatment is advised, physical therapy might be an option.
What is the hip fracture treatment that is most frequently used?
Your hip will probably need to be fixed surgically. Surgery is usually successful, but recovery from this procedure will likely be gradual. When a hip fracture is identified, surgery is performed as soon as possible—typically within 24 hours.
What causes a hip fracture?
Hip fractures are most common in those 65 years of age and older, and they are usually caused by falls. As you age, your bones naturally deteriorate and become more fragile, even from little falls. Sports injuries, car crashes, and bicycle accidents are the main causes of hip fractures in children and young adults.
What age are you at risk for a hip fracture?
The majority of hip fractures happen to older adults (52% after age 80 and 90% after age 50).
References
- Emmerson, B. R. (2023, August 8). Hip Fracture Overview. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK557514/
- Team, P. (n.d.). Hip fractures notes. Pulsenotes. https://app.pulsenotes.com/surgery/orthopaedics/notes/hip-fractures
- Hip Fractures – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/hip-fractures/
- Hip fracture – Symptoms & causes – Mayo Clinic. (2022, May 5). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/hip-fracture/symptoms-causes/syc-20373468
- Causes. (n.d.). Stanford Health Care. https://stanfordhealthcare.org/medical-conditions/bones-joints-and-muscles/hip-fracture/causes.htm
- Professional, C. C. M. (n.d.). Hip Fracture. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17101-hip-fracture
- Diagnosing Hip & Pelvic Fractures. (n.d.). NYU Langone Health. https://nyulangone.org/conditions/hip-pelvic-fractures/diagnosis



One Comment