Structure Of Bone Tissue
Introduction
The structure of bone tissue is a connective tissue that is metabolically active, helps with mobility, supports structure, and shields important organs. Osteocytes, bone cells, and extracellular matrix make up bone. The correct circumstances cause bone tissue to go through a mineralization process where calcium is deposited and hardens the tissue. Because of its inherent toughness, bone serves a variety of purposes.
An adult human’s skeleton consists of 206 bones. There are roughly 270 bones at birth, and as the skeleton grows and matures, some of these bones merge, resulting in a lower final adult count. Bone remodels continuously throughout life; the adult skeleton is mostly regenerated every ten years or so.
The structure of bone tissue has both a supporting and a motor role. In addition to supplying the body’s structural framework, bones serve as attachment points for muscles, tendons, and ligaments, which permit movement. Moreover, bones support breathing, safeguard important organs, enable movement, contribute to homeostasis, and generate a range of bone marrow cells that are essential for existence. The ability of the structure of bone tissue to regenerate and return to its pre-injury, fully functional state makes it special.
Types of Bone
One type of connective tissue that makes up the endoskeleton is bone or osseous tissue. It is made up of specialized cells and a collagen-fiber and mineral-salt matrix.
The mineral hydroxyapatite, which is made of calcium phosphate, is the main component of the mineral salts. The process of mineral salts depositing on the collagen fiber matrix to cause the tissue to crystallize and harden is known as calcification. Calcification can only take place when collagen fibers are present.
The human skeleton’s bones are categorized according to their shapes: sesamoid, long, short, flat, sutural, and irregular bones.
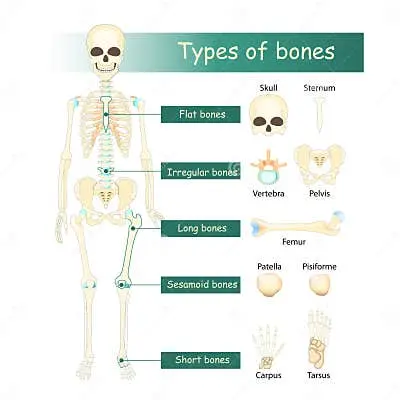
Long bones have a shaft and two ends and are longer than wide. There is bone marrow in a marrow cavity located in the diaphysis, or central shaft. The epiphyses, or rounded ends, are packed with red bone marrow that creates blood cells and is covered in articular cartilage. The majority of limb bones, such as the radius, ulna, tibia, and femur, are long bones. The patella and the wrist and ankle bones are examples of exceptions to this rule.
Bones that have the same breadth and length, or cuboidal bones, are known as short bones because of their cube-like shape. The ankle (tarsals) and wrist (carpals) are two examples of short bones.
When large surfaces for muscle attachment or substantial organ protection are needed, flat bones—which are thin and comparatively broad—are present. The roof of the skull, ribs, scapulae (shoulder blades), and sternum (breast bone) are a few examples of flat bones.
Bones with complicated forms are called irregular bones. The surfaces of these bones could be short, flat, ridged, or notched. The hip bones, various skull bones, and the vertebrae are a few examples of irregular bones.
Sesamoid bones resemble sesame seeds in appearance and are small, flat bones. The sesamoid bones are called patellae. Sesamoid bones can be found close to the knees, hands, and feet. They form inside tendons.
Small, flat, asymmetrically formed bones are known as sutural bones. They could be located in the space between the skull’s flat bones. Their quantity, form, size, and placement all differ.
Gross Anatomy Of Bone
Two primary areas of a long bone are the diaphysis and the epiphysis. The hollow, tubular shaft that connects the proximal and distal ends of the bone is called the diaphysis. The medullary cavity, which houses the adult’s yellow bone marrow, is located inside the diaphysis. Compact bone, a type of osseous tissue, is dense and hard, making up the outer walls of the diaphysis (cortex, cortical bone).
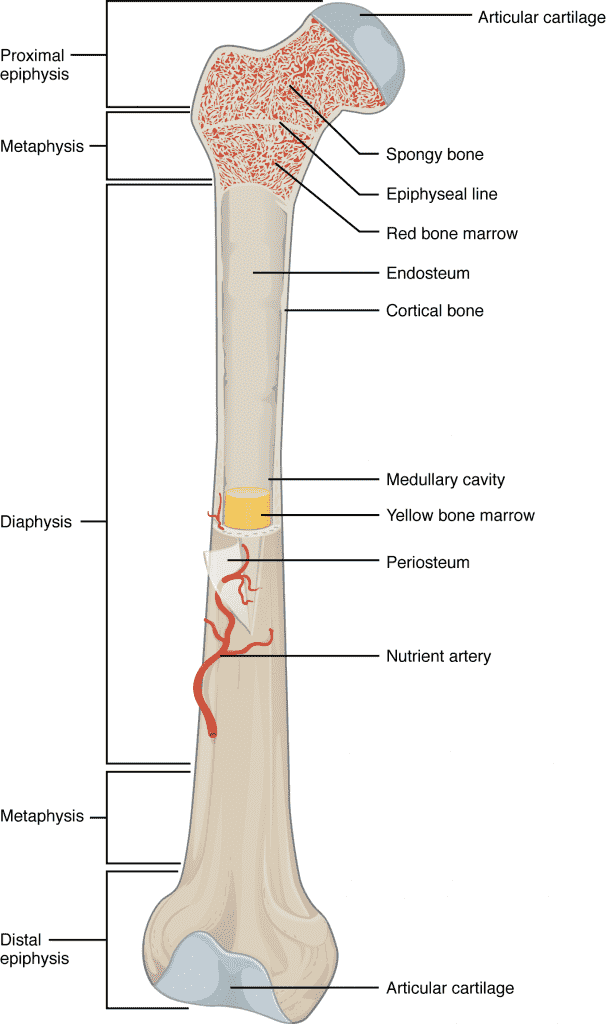
The term epiphysis (plural: epiphyses) refers to the broader part at each end of the bone that is internally filled with spongy bone, another kind of osseous tissue. In certain lengthy bones, the crevices between the spongy bones are filled with red bone marrow. At the metaphysis, each epiphysis and diaphysis collide.
The epiphyseal plate, the location of long bone elongation discussed later in the chapter, is located in the metaphysis throughout growth. In early adulthood (about 18–21 years), the bone stops developing, and the epiphyseal plate transforms into the epiphyseal line that is depicted in the image.
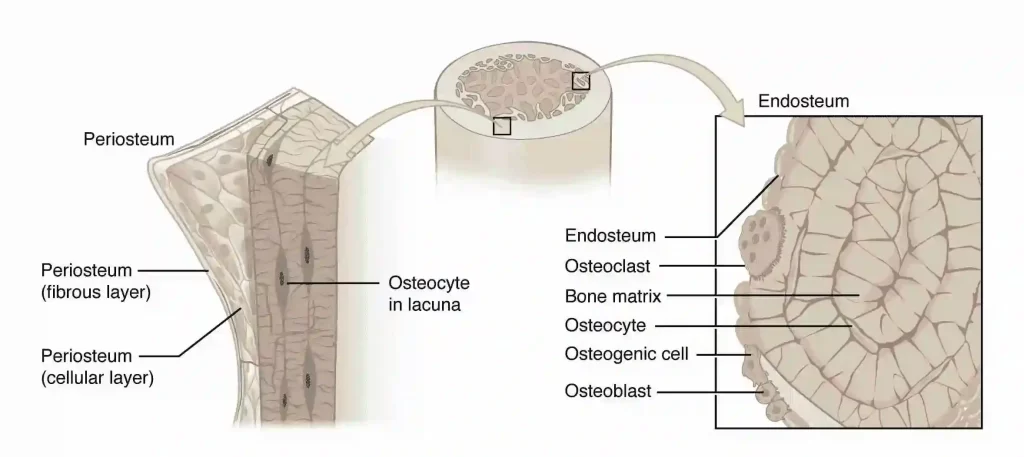
The endosteum (endo- = “inside”; osteo- = “bone”) is a layer of bone cells that lines the inside of the bone next to the medullary cavity. Throughout life, the bone grows, repairs, and remodels because of these bone cells (more on those later). There is an additional layer of cells that grow, repair, and remodel bone on the outside of bones. These cells are a component of the periosteum, an exterior double-layered structure (peri–meaning “around” or “surrounding”).
The outer fibrous layer of dense, uneven connective tissue covers the cellular layer, which is located next to the cortical bone. In addition, the periosteum is home to lymphatic, neuron, and blood arteries that support dense bone. The periosteum is where ligaments and tendons join to bones. The whole exterior is covered in periosteum, except for joints formed by the junctions of epiphyses and other bones. Articular cartilage, a thin coating of hyaline cartilage that serves as a shock absorber and minimizes friction, covers the epiphyses in this area.
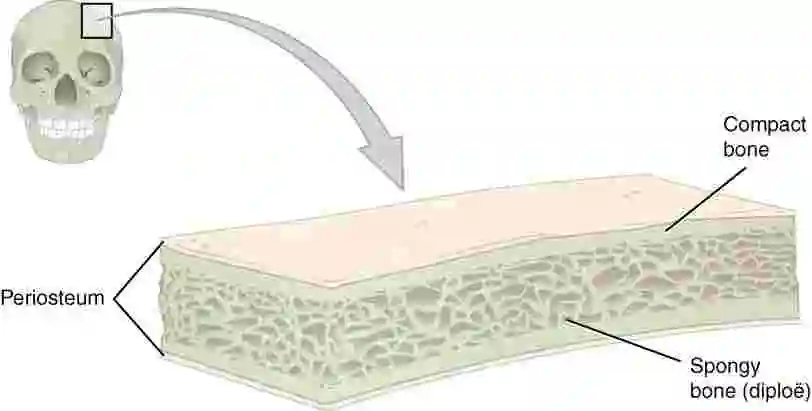
Compacted bone covers the diploe (spongy bone) layer on both sides of flat bones, such as those seen in the cranium. Together, the interior spongy bone and the two layers of compact bone shield the internal organs. The undamaged inner layer of a skull bone continues to protect the brain even in the event of an outer layer fracture.
Structure Of Bone Tissue
Compact and spongy osseous tissue makes up the majority of the structure of bone tissue, however, the distribution and concentration of this tissue change depending on the overall function of the bone. While both compact and spongy bones consist of the same cells and matrix components, their anatomical configurations differ. While spongy bone, also called cancellous bone, contains open gaps, is supporting, lightweight, and easily adaptable to meet changing body needs, compact bone is dense enough to endure compressive forces.
An osteon, also known as a Haversian system, is the microscopic structural unit of compact bone. Lamellae (singular: lamella) are concentric rings of the calcified matrix that make up each osteon. The Haversian canal, or central canal, is located in the middle of each osteon and is home to lymphatic, nerve, and blood vessels. To reach the periosteum and endosteum, these vessels and nerves split out at right angles via perforating canals, also referred to as Volkmann’s canals.
Osteocytes are situated inside what are known as lacunae (singular: lacuna), which are gaps that are present at the edges of neighboring lamellae. Canaliculi link to the canaliculi of different lacunae and ultimately to the central canal, as was previously mentioned. Waste products can be taken out of the osteocytes and nutrients can be delivered to them via this system.
Compact Bone
The two forms of osseous tissue, compact bone is the denser and stronger type. It immediately contacts the periosteum and constitutes the outer cortex of every bone. In long bones, the transition from the inner medullary cavity to the outer cortical solid bone occurs in a spongy manner.
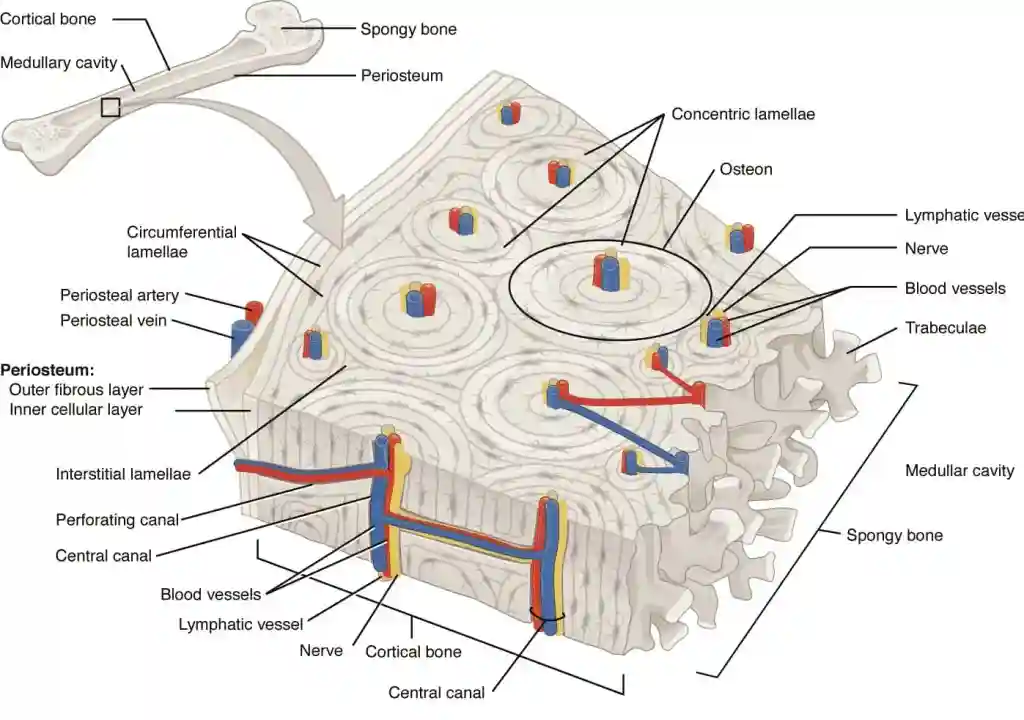
Examining compact bone under a microscope reveals a very well-organized pattern of tree-trunk-like concentric rings. An osteon, also known as a Hadrian system, is the microscopic structural unit of compact bone composed of each group of concentric circles, or each “tree.” Each ring of the osteon is referred to as a lamella (plural: lamellae) and is composed of collagen and calcified matrix.
Because the collagen fibers in adjacent lamellae are oriented perpendicular to one another, osteons can withstand twisting stresses in several directions each osteon has a central canal, also known as the Haversian canal, that is home to lymphatic, nerve, and blood vessels. To reach the periosteum and endosteum, these vessels and nerves split out at right angles via perforating canals, also referred to as Volkmann’s canals. Additionally, the endosteum lines each central canal, facilitating the gradual removal, remodeling, and rebuilding of osteons.
Spongy (Cancellous) Bone
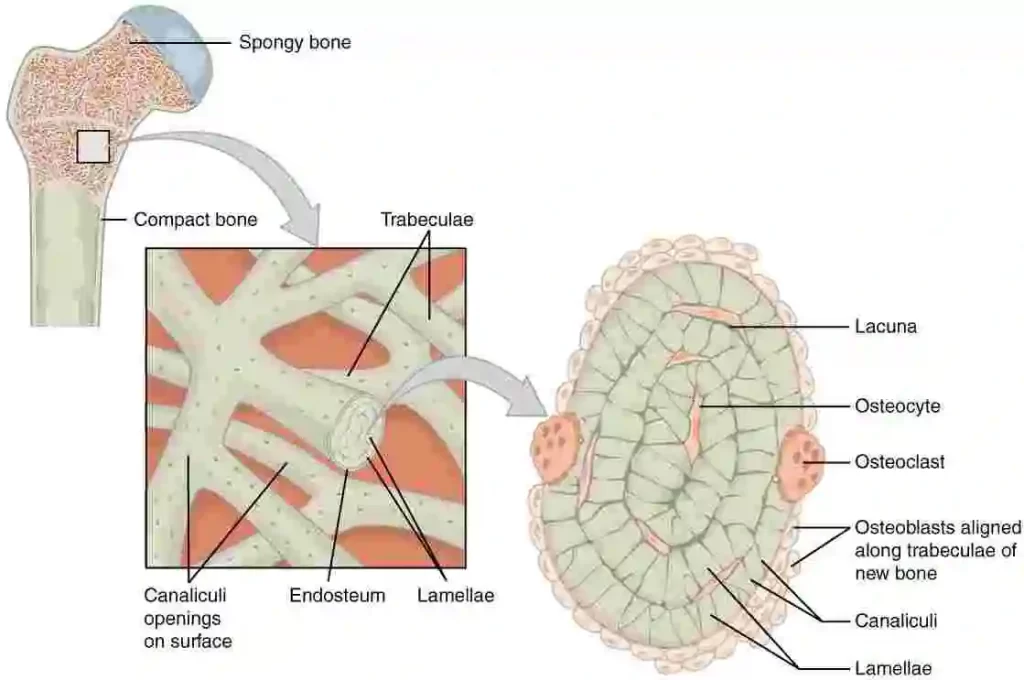
Osteocytes in cancellous bone, commonly referred to as spiky bone, are contained in lacunae similar to those in compact bone, but they are not grouped in concentric rings. Rather, a lattice-like network of matrix spikes known as trabeculae (plural: trabecula) contains the lacunae and osteocytes.
The endosteum, which covers the trabeculae, is easily able to reconstruct them. Although the trabeculae may seem to be a random network, each one forms along stress lines to send forces outward to the more compact, solid bone, which gives the bone strength. Spongy bone makes bones lighter so that muscles may move them more freely, balancing the dense and heavy compact bone. Furthermore, hematopoiesis takes place in the red bone marrow that is housed in the crevices between some spongy bones and is shielded by trabeculae.
Aqueous flow via the compact bone supplies nutrients to the medullary cavity and spongy bone. The arteries enter through tiny apertures in the diaphysis called nutritional foramen (plural: foramina). Blood that circulates in the marrow cavities and periosteum blood capillaries that pierce spongy bone nourish the osteocytes within. Veins gather the blood as it travels through the marrow cavities and exits the bone through the foramina.
Nerves enter the bone along the same pathways as blood vessels, with the tendency to cluster in the areas of the bone that are more metabolically active. In addition to sensing pain, nerves appear to have an impact on bone formation and blood flow, which explains why they are concentrated in areas of the bone that are metabolically active.
Bone Matrix
Three primary components make up the specialized connective tissue known as bone:
- Calcified extracellular substance
- Bone matrix
- Bone cells (osteocytes, osteoblast and osteoclast)
The intercellular material that makes up the majority of a bone’s bulk is called the bone matrix. Its makeup is made up of both organic and inorganic components.
The bulk of the bone is composed of inorganic matter. Although calcium hydroxyapatite makes up the majority of it, large levels of bicarbonate, citrate, magnesium, potassium, and sodium ions are also present.
Collagen fibers (type I), proteoglycans, and glycoproteins (such as osteonectin and osteocalcin) make up the organic component of the bone matrix. The osteoblasts generate and secrete the organic substance. Osteoblasts have a cuboid shape and basophilic cytoplasm when they are actively producing the components of the bone matrix. On the other hand, they flatten and lose some of their basophilic characteristics when they are dormant.
The primary role of the bone matrix is to give the bones mechanical support.
Bone Cells
The cells that comprise bone tissue are called bone cells. The three primary purposes of bone, a highly specialized connective tissue, are to protect internal organs, provide a stiff framework for muscle activity, and store minerals like calcium and phosphorus.
Types of Bone Cells
The four cell types that makeup bone tissue are osteoblasts, osteoclasts, osteocytes, and osteoprogenitor cells. Together, these cells—each with a distinct function—maintain the homeostasis of the bone tissue using bone remodeling, which is the process of replacing deteriorated bone tissue with new bone tissue. They control the morphology and functionality of bone tissue in this way.
Osteoblasts
Cuboidal cells called osteoblasts are layered closely together along the surface of the bone. Their primary job is to create new bone tissue, and they make up 4–6% of all bone cells. With a big Golgi apparatus for copious protein production and an expansive rough endoplasmic reticulum, osteoblasts are uniquely suited for this job.
Numerous chemicals, including collagen, different proteins, and calcium salts, are secreted by these cells. These components come together to produce the bone matrix, a sophisticated scaffolding that supports the skeletal system. Because it produces chemicals that affect bone cell activity and, consequently, the remodeling of bone tissue, the bone matrix is also essential to maintaining bone homeostasis.
Osteoblasts don’t split apart. The cells are trapped in the center while the bone matrix calcifies and develops around them over time. The osteoblast undergoes a structural transformation as a result, developing into an osteocyte [a mature kind of bone cell].
Osteocytes
Osteocytes, essentially osteoblasts encircled and imprisoned by the materials they secrete, make up the bulk of bone cells. Every osteocyte is located in a little area encircled by bone tissue, known as a lacuna.
95% of the cells in bone tissue are called osteoclasts. They live for up to 25 years and do not divide, just like osteoblasts.
Osteocytes have many crucial roles in preserving the mineral makeup of bone tissue. They may deposit and reabsorb bone, and if there is even the slightest damage to the bones, they will alert other osteocytes. They control the calcium reserve in the bone and the activity of osteoblasts and osteoclasts. Osteocytes are therefore essential to the remodeling of bone.
Through lengthy passageways called canaliculi found in the bone matrix, osteoblasts exchange messages with one another and transfer waste materials and nutrients.
Osteoclasts
Large cells called osteoclasts are primarily responsible for breaking down and reabsorbing bone tissue. They come from white blood cells (monocytes and macrophages) rather than from other bone cells and are present on the surface of bone tissue.
Whereas osteoblasts create new bone tissue, osteoclasts continuously degrade and reabsorb existing bone tissue. These two cells work together to regulate the progressive reshaping of the bones.
Osteoprogenitor cells
The stem cells present in bone tissue are called osteoprogenitor cells. From osteoprogenitor cells in the bone marrow, specialized bone cells (osteocytes and osteoblasts) develop. Osteoclasts begin as blood stem cells in the bone marrow and do not grow from osteogenic cells.
Bone marrow
The spongy material inside your bones is called bone marrow. After producing blood cells, it takes on the role of storing fat and specific stem cells. Many different disorders are associated with malfunctioning bone marrow.
The skeleton’s bones provide a variety of vital roles for the body, including enabling movement and providing support. They are also crucial for the synthesis of red blood cells and the storage of fat.
There are two varieties of bone marrow:
- Red bone marrow: production of blood cells.
- Yellow bone marrow: fat storage.
Red Bone Marrow
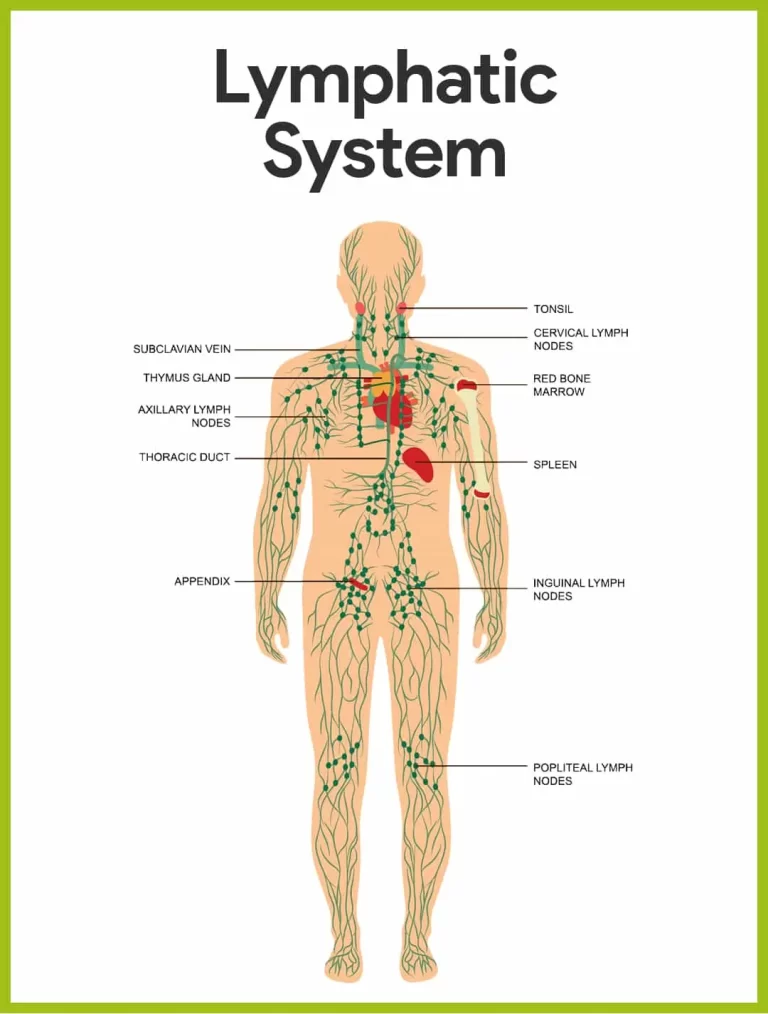
Hematopoietic cells, or stem cells that generate blood, are found in the fibrous tissue that makes up red bone marrow, also known as myeloid tissue. In adults, the red bone marrow produces all red blood cells, platelets, and between 60% and 70% of white blood cells.
The remaining early white blood cells, known as lymphocytes, start as red bone marrow-derived precursors before maturing into fully formed tissues in organs such as the spleen, thymus, and lymph nodes.
Yellow Bone Marrow
The fattier yellow bone marrow contains mesenchymal or marrow stromal cells. These stem cells give rise to the body’s connective tissues, which include muscle, bone, fat, and cartilage.
For the red bone marrow to employ and sustain bodily processes, the yellow bone marrow also stores fat and nutrients. In times of stress, such as during an illness or significant blood loss, the body’s yellow bone marrow can change into red bone marrow and assume its role.
Fats are kept in reserve in the yellow bone marrow. Adipocytes are the cells in the yellow bone marrow that store fat. When needed, this fat can be utilized as a source of energy.
Mesenchymal stem cells are seen in yellow bone marrow as well. These are the cells that can differentiate into muscle, fat, cartilage, or bone.
The majority of the bones in an adult body contain yellow bone marrow because yellow bone marrow gradually replaces red bone marrow.
Function of Bone marrow
The production of bone marrow stem cells and blood products is one of the body’s most important uses for bone marrow. The process by which the bone marrow makes platelets, white blood cells, and red blood cells is known as hematopoiesis. Bone marrow comes in two primary varieties, and each has a distinct function.
- Red blood cells. These are the cells that function to transport blood enriched with oxygen to the body’s cells. Red bone marrow can also break down old red blood cells, however, this process is primarily carried out in the liver and spleen.
- Platelets. Blood clots are aided by platelets. This stops bleeding that isn’t regulated.
- White blood cells. White blood cells are classified into various categories. Each one of them aids in the body’s defense against infections.
Your red bone marrow eventually gives way to yellow bone marrow as you become older. Only a few bones remain with red bone marrow in adulthood, these being the:
- Skull
- Vertebrae
- Sternum
- Ribs
- The humerus’s (upper arm bone) extremities
- Pelvis
- The ends of the femur (thigh bone)
- The ends of the tibia (shin bone)
Blood and Nerve Supply to the Bones
Since bones are active organs, they need an abundance of nutrients and oxygen. Blood goes to the bones from the heart at a rate of 5–10% of total cardiac output. The periosteal arteries, metaphyseal and epiphyseal arteries, and the nutrient artery are the three primary sources of a normal long bone.
Nutrient Artery
The principal blood vessel that passes through the nutrient foramen and into the diaphysis is the nutrient artery. Large bones, like the femur, may have two nutrition foramen, but the majority of long bones only have one. The primary ascending and descending branches of this high-pressure artery system travel parallel to the long axis of the bone. The inner two-thirds of compact bone and the bone marrow in the medullary cavity are supplied by these radially branching out into smaller vessels.
Metaphyseal and Epiphyseal Arteries
To give blood to the spongy bone, the metaphyseal arteries transversely penetrate the bone at the metaphyses. The trabeculae of the spongy bone are supplied by the numerous divisions of these arteries, which create a dense network of tiny blood vessels. The metaphyses are the most vascularized area of the bone as the blood vessels join and integrate with the dense network that arises from the main nutrient branches. The red bone marrow and spongy bone are supplied by a network of tiny vessels formed by the entry of another set of arteries, known as the epiphyseal arteries, into the epiphyses.
Periosteal Arteries
Many of the blood arteries that are present near the periosteum on the surface of the bone enter transversely through Volkmann’s canals. Through the Haversian canals of the osteons, this low-pressure system provides blood to the outer part of the compact bone.
Venous System
Via a system of veins that resembles the arterial system, blood from the bone drains away. The epiphyses and metaphyses, respectively, are the draining organs for the epiphyseal and metaphyseal veins. One or two nutrient veins emerge from the diaphysis’s radial vasculature and leave the bone through the nutrient foramen. Many periosteal veins drain blood from the exterior compact bone and exit through the periosteum.
Nervous System in Bones
Rich nerve supply that travels along similar pathways as blood vessels are found in the bone. The periosteum of the bone has a disproportionately high density of these sensory nerves. The brain receives pain signals from the nerves, which are responsible for detecting injuries like tearing or stress. As a result, bone injury, particularly that which affects the periosteum, can be quite painful. For instance, the patient experiences discomfort when the needle punctures the periosteum during a bone marrow biopsy. However, the level of discomfort lessens as it passes through and enters the spongy bone marrow.
Ossification & Remodeling Of Bone
Ossification
Endochondral or intramembranous osteogenesis (ossification) are the two processes that initiate bone development in a growing embryo. A hallmark of intramembranous ossification is the direct emergence of bone tissue from mesenchyme. This procedure forms flat bones like the occipital and parietal bones.
Conversely, endochondral ossification relies on a model of cartilage. Phalanges and the femur are examples of long and short bones that develop from a cartilage model created by endochondral ossification. There are no different kinds of bone tissue implied by the differences between these two forms of osteogenesis.
The identical bone tissue is produced by both procedures, but they differ in whether or not a cartilage model is present.
Intramembranous Ossification
During intramembranous ossification, sheets of mesenchymal (undifferentiated) connective tissue immediately give rise to compact and spongy bone. Intramembranous ossification is the process by which the clavicles (collarbones), the majority of the cranial bones, and the flat bones of the face form.
Mesenchymal cells in the embryonic skeleton come together and start to differentiate into specialized cells, which is when the process starts. While some of these cells will evolve into osteogenic cells and eventually osteoblasts, others will become capillaries. The ossification core is the cluster in which early osteoblasts appear, albeit the production of bone tissue will eventually disperse them.
Osteoid, an uncalcified matrix secreted by the osteoblasts, calcifies (hardens) in a matter of days upon the deposition of mineral salts, trapping the osteoblasts inside. The osteoblasts become osteocytes after they are confined. Osteogenic cells in the surrounding connective tissue differentiate into new osteoblasts as osteoblasts change into osteocytes.
A trabecular matrix is produced by osteoid (unmineralized bone matrix) released around capillaries, and osteoblasts on the surface of spongy bones form the periosteum. Next, a compact bone layer that is superficial to the trabecular bone is formed by the periosteum. Neighboring blood veins become crowded by the trabecular bone and eventually condense into red marrow.
Endochondral Ossification
Bone takes the place of hyaline cartilage during endochondral ossification. Bone does not grow from cartilage. Rather, cartilage acts as a template for new bone to grow in its place. Compared to intramembranous ossification, endochondral ossification occurs far more slowly. Osteochondral ossification is the process by which long bones and the skull base develop.
For instance, in a long bone, some mesenchymal cells transform into chondrocytes, or cartilage cells, which create the cartilaginous skeletal precursor of the bones, approximately 6 to 8 weeks after conception. The cartilage-covering membrane known as the perichondrium soon emerges.
The chondrocytes in the cartilaginous model’s core enlarge as more matrix is created. The chondrocytes are deprived of nutrition as the matrix hardens. Their demise and the surrounding cartilage’s breakdown follow from this. The resulting voids are invaded by blood arteries, which not only cause the cavities to enlarge but also bring osteogenic cells, many of which will develop into osteoblasts. The combination of these expanding areas ultimately forms the medullary cavity.
Cavities pierce the cartilage as it matures. The perichondrium begins to change into the periosteum, which makes bones, as a result of this penetration. Here, the osteoblasts encircle the diaphysis cartilage with a compact bone periosteal collar. The main ossification core, located deep within the periosteal collar, is the result of an increase in bone cell growth and ossification during the second or third month of fetal life.
As these profound alterations take place, cartilage, and chondrocytes continue to proliferate at the extremities of the bone (the future epiphyses), lengthening the bone while also replacing the cartilage in the diaphyses. By the time the fetal skeleton is fully developed, the cartilage only survives as articular cartilage at the joint surface and as the epiphyseal plate, which is in charge of the longitudinal growth of bones, between the diaphysis and epiphysis.
The same series of events—matrix mineralization, chondrocyte death, periosteum-derived blood vessel invasion, and osteogenic cell seeding that develops into osteoblasts—occur in the epiphyseal regions after birth. These areas of activity are collectively known as secondary ossification centers.
Remodeling
Bone modeling is the process of resorbing a matrix on one surface of a bone and depositing it on another. Most modeling occurs when a bone is growing. But during the remodeling process of adult bone, old or damaged bone is resorbed on the same surface where osteoblasts form new bone to replace the resorbed material.
Remodeling is caused by injuries, exercise, and other activities. These factors are covered later in the chapter, but even in the absence of trauma or exercise, the annual remodeling of 5–10% of the skeleton consists of the simple removal of old bone and replacement of it with new bone.
Function Of Bone Tissue
Support, Movement, and Protection
Some skeletal system functions are easier to see than others. You can feel how your bones support you, allow you to move more easily, and shield your body’s sensitive organs when you move. Your skeletal system’s bones and cartilage make up the structure that supports the rest of your body, much like a building’s steel beams do to hold its weight. You wouldn’t be more than a limp mass of muscles, skin, and organs without the skeletal system. Because they are places of attachment for your muscles, bones help you move.
Internal organs are likewise protected from harm by the covering or encirclement of bones. For instance, the bones of your cranium (head) shield your brain, the bones of your vertebral column (spine) protect your spinal cord, and your ribs shield your heart and lungs.
Mineral and Fat Storage, Blood Cell Formation
Bone tissue carries out numerous vital metabolic processes. One benefit of bone tissue is that it serves as a storage space for various minerals, including phosphorus and calcium, vital to bodily functions. Once assimilated into bone tissue, these minerals can be released back into the bloodstream to sustain the necessary concentrations for supporting bodily functions. For example, calcium ions play a crucial role in transmitting nerve impulses and are necessary for muscular contractions.
Additionally, fat is stored and blood cells are produced in the bones. Bone marrow is the special connective tissue that lines the inside of most bones. There are two distinct types of bone marrow: red and yellow.
Adipose tissue, or yellow bone marrow, can release its stored triglycerides into the adipocytes, which can then supply energy to other body tissues. The process of producing red blood cells is known as hematopoiesis (hemato- = “blood,” -poiesis = “to make”). The erythrocyte produces red blood cells, white blood cells, and platelets.
FAQs
What is the bone’s composition and purpose?
The body uses bones for support, form, and to shield some internal organs. In addition, bone provides the marrow needed for blood cell growth and storage as well as a place to store minerals.
Which is the fundamental structural component of bone tissue?
Osteons are structural and functional units of compact bone, to sum up. Each osteon is composed of four components: perforating canals, lamellae (bone matrix structures), osteocyte-containing cavities (holes), and the central canal, which houses blood vessels and nerves.
What makes a bone a structure?
The framework that keeps the body together and permits movement is made up of bones. However, in addition to these important functions, bones also store minerals, protect essential organs, and provide an environment in which bone marrow is formed. The body continuously remodels the living, active tissues that make up bones.
Which two forms of bone tissue are there?
Compact bone tissue sometimes referred to as hard or cortical bone, and spongy bone tissue, also known as cancellous or trabecular bone, are the two distinct forms of osseous tissue.
What kind of structure do long bones have?
Long bones have an inner medullary cavity that contains bone marrow and a thick covering of compact bone on the outside. An epiphyseal line and spongy bone can be found at the ends of lengthy bones. The epiphyseal line is what’s left of an area where hyaline cartilage expands to extend the bone throughout childhood.
What is the tissue of bones?
Four different cell types can be found in bone, which is a mineralized connective tissue: osteoblasts, osteocytes, osteoclasts, and bone lining cells. Important bodily roles that bones perform include supporting and shielding soft tissues, storing calcium and phosphate, and housing bone marrow.
Reference
- Bone. (n.d.). Physiopedia. https://www.physio-pedia.com/Bone
- Biga, L. M. (2019, September 26). 6.3 Bone Structure. Pressbooks. https://open.oregonstate.education/aandp/chapter/6-3-bone-structure/
- Types of Bone | Biology for Majors II. (n.d.). https://courses.lumenlearning.com/wm-biology2/chapter/types-of-bone/
- Grujičić, R. (2023, October 30). Bone matrix. Kenhub. https://www.kenhub.com/en/library/anatomy/bone-matrix
- Latham, K. (2021, May 11). Bone Cells. Biology Dictionary. https://biologydictionary.net/bone-cells/
- Bsn, R. Z. (2023, June 20). The Anatomy of Bone Marrow. Verywell Health. https://www.verywellhealth.com/bone-marrow-anatomy-5076272
- Seladi-Schulman, J. (2022, February 7). What Is Bone Marrow, and What Does It Do? Healthline. https://www.healthline.com/health/function-of-bone-marrow#yellow-bone-marrow
- Blood and nerves supply to the Bones. (n.d.). JoVE. https://www.jove.com/science-education/14014/blood-and-nerve-supply-to-the-bones
- Betts, J. G. (2022, April 20). 6.4 Bone Formation and Development – Anatomy and Physiology 2e | OpenStax. https://openstax.org/books/anatomy-and-physiology-2e/pages/6-4-bone-formation-and-development
- Biga, L. M. (2019, September 26). 6.1 The Functions of the Skeletal System. Pressbooks. https://open.oregonstate.education/aandp/chapter/6-1-the-functions-of-the-skeletal-system/