Popliteus tendinitis and Physiotherapy management
- Popliteus tendinitis is inflammation of the popliteus muscle which is present in the back of the knee. Popliteus tendonitis is an uncommon pathology that often occurs in athletes and people with a history of other knee ligament injuries.
- The pathology involves popliteus muscle which is present on the posterolateral aspect of the knee region.
- The Popliteus muscle is a key stabilizer of the knee and plays an important role in maintaining proper mechanics at the knee during walking, running, and climbing stairs.
Anatomy related to Popliteus tendinitis
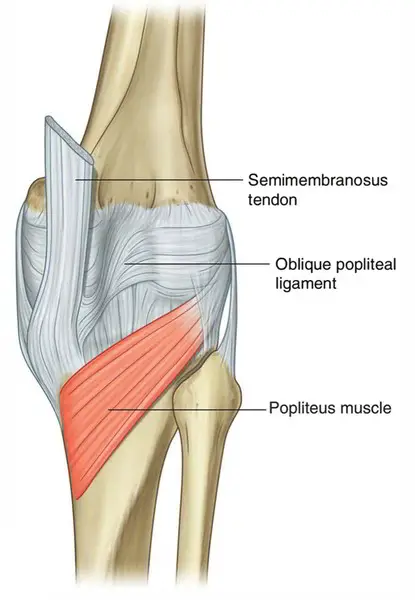
- Popliteus muscle originates from the lateral femoral condyle [strongest origin], just anterior and inferior to the lateral collateral ligament origin, from the fibula, and from the posterior horn of the lateral meniscus.
- The muscle inserts on the posterior surface of the tibia above soleal or popliteal line occupying about 10 to 12 cms of the tibia.
- The popliteus tendon runs deep to lateral collateral ligament and passes through a hiatus in the coronary ligament to attach to the femur.
- It is supplied by the Tibial nerve (L4, L5, S1). The blood supply of the popliteus muscle is from the medial inferior genicular branch of the popliteal artery and the muscular branch of the posterior tibial artery.
- Popliteus is an internal rotator of the knee. It assists in initiating knee flexion and early rotational unlocking from the tibia. Unlocking is accomplished contour of articulation & retraction of the posterior aspect of the lateral meniscus.
- It rotates the tibia medially on the femur or femur laterally on the tibia depending on which one is fixed. It also works to withdraw the meniscus during flexion in some persons and provides rotatory stability to the femur on the tibia.
- In addition, popliteus also acts as secondary restraint in preventing posterior tibial translation on the femur.
- It prevents posterior translation of the tibia on the femur.
- Apart from these, popliteus prevents excessive external rotation of the tibia.
Causes of Popliteus tendinitis
- popliteus tendinitis commonly occur when one feet roll inward.
- running downhill puts extra pressure on popliteus tendon which also causes tendinitis.
- pressure is placed on popliteus tendon during such everyday movement as the feet hitting the ground.
- running downhill can put an inordinate strain on the tendon if practiced excessively.
- this occurs more often than general sprinting because the surface is not flat.
- other factors that can contribute to straining the tendon include overuse, running with fatigued muscles, for too great a length of time, or without suitable warm-ups or stretches.
- injury is regularly felt after the ankle rolls unusually inward, causing a tear in the tendon.
Clinical presentation of Popliteus tendinitis
- Knee pain which is aggravated by the movement of the knee.
- Additional symptoms include redness, swelling, and tenderness in the back knee.
- The swelling will be outside of the knee. pain will be enough that you can not walk comfortably.
- Popliteus tendon will immediately be swollen and will be very tender.
- Pain is of insidious onset and present along with a posterolateral portion of the knee. The occurrence of the pain is mainly during weight-bearing when the knee is between 15-30 degrees of flexion [during the early swing phase].
- History might further reveal a recent activity like downhill running, running on banked surface or backpacking downhill.
- The pain is aggravated by running and relieved by rest.
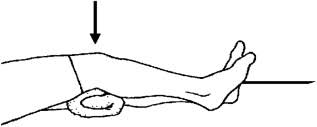
- There is tenderness at tendinous insertion at lateral femoral condyle. For palpating the popliteus the lower limb is kept in “fig of 4”.
- Findings may absent during rest period and having patient run downhill prior to examination may be helpful.
- Joint effusion absent unless concomitant problem.
Medical management of Popliteus tendinitis
- The treatment for popliteus tendinitis includes rest, ice application, elevation, an elastic wrap, physical therapy, and nonsteroidal anti-inflammatory medication for pain, such as aspirin or ibuprofen. Additional treatment for popliteus tendinitis may include oral corticosteroids or corticosteroid injections.
- Many individuals find a compression bandage or a knee sleeve very useful to reduce symptoms. Alternatively, in order to reduce the pain, the physician may also recommend taping the area of the injury.
- But when it comes to severe tendinitis(symptoms persist for more than 6 months), surgery has to be performed to remove the tendon sheath.
Physiotherapy management of Popliteus tendinitis
- Pain-relieving modalities such
- ULTRASOUND THERAPY: UltraSound is a therapeutic modality that generates ultrasound causes deep heat, provides micro-massage to soft tissue, increases flexibility, promotes healing of tissue as well improves localized blood supply to the area, and ultimately pain relief.
- SHORT WAVE DIATHERMY: short wave diathermy is a deep heating modality that uses heat to provide pain relief, it improves the blood supply to targeted muscle, removal of waste products.

- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.
- Cold therapy: used to relieve inflammation and reduce pain, Ice Massage- Ice on the area of inflammation for anti-inflammatory effects. Use ice in a paper or Styrofoam cup (peeled away) for 5-7 minutes, make sure to avoid frostbite.
ACUTE PHASE

- Rest: Rest prevents the worsening of the initial injury. By placing the injured extremity to rest the first 3-7 days after the trauma, we can prevent further retraction of the ruptured muscle stumps (the formation of a large gap within the muscle), reduce the size of the hematoma, and subsequently, the size of the connective tissue scar.
- During the first few days after the injury, a short period of immobilization accelerates the formation of granulation tissue at the site of injury, but it should be noted that the duration of reduced activity (immobilization) ought to be limited only until the scar reaches sufficient strength to bear the muscle-contraction induced pulling forces without re-ruptureAt this point, gradual mobilization should be started followed by a progressively intensified exercise program to optimize the healing by restoring the strength of the injured muscle, preventing the muscle atrophy, the loss of strength and the extensibility, all of which can follow prolonged immobilization.
- Ice or cold application: It is thought to lower intra-muscular temperature and decrease blood flow to the injured area. Regarding the use of cold on injured skeletal muscle, it has been shown that early use of cryotherapy is associated with a significantly smaller hematoma between the ruptured myofiber stumps, less inflammation and tissue necrosis, and somewhat accelerated early regeneration. However, according to the most recent data on the topic, icing of the injured skeletal muscle should continue for an extended period of time (6 hours) to obtain a substantial effect on limiting the hemorrhaging and tissue necrosis at the site of the injury.
- Compression: This may help decrease blood flow and accompanied by elevation will serve to decrease both blood flow and excess interstitial fluid accumulation. The goal is to prevent hematoma formation and interstitial edema, thus decreasing tissue ischemia. However, if the immobilization phase is prolonged, it will be detrimental to muscle regeneration. Cryotherapy, accompanied by compression, should be applied for 15–20 min at a time with 30–60 min between applications. During this time period, the quadriceps should be kept relatively immobile to allow for appropriate healing and prevent further injury.
- Elevation: The elevation of an injured extremity above the level of the heart results in a decrease in hydrostatic pressure, and subsequently, reduces the accumulation of interstitial fluid, so there is less swelling at the place of injury. But it needs to be stressed that there is not a single randomized, clinical trial to validate the effectiveness of the RICE principle in the treatment of soft tissue injury.
REHABILITATION PHASE
- Isometrics exercise of quadriceps will help to maintain muscle power of quadriceps muscle, Isometrics: Initial isometrics with quadriceps contractions done with the knee fully extended and in different positions at 20-degree increments as knee flexion improves May discontinue isometrics when the patient can sit comfortably.
- Straight leg raises: Sit flat on the floor with the legs straight out in front of you. Raise one leg off the floor keeping the knee straight. Hold for 3 to 5 seconds before lowering back to the ground. Repeat 10 to 20 times. This exercise can be done daily. Progress the exercise by increasing the length of hold and the number of reps.

- Strengthening exercises and stretching: when the pain has reduced sufficiently, strengthening and stretching exercises can begin and these can then be built up gradually. The most effective form of muscle training in cases of tendon problems is eccentric training because the collagen fibers will be set in the right/functional direction.
- For the popliteus, eccentric strengthening (closed kinetic chain) of the quadriceps is effective in reducing strain on the popliteus.
- Patients should not run until the knee is free of pain, then they should limit their workouts and downhill running for at least 6 weeks. During the treatment, cycling provides a good alternative exercise.
Strengthening Exercises
Here are three exercises to strengthen the affected popliteus muscle:
- Exercise 1: Reverse heel tap
- Attach a resistance band onto the forefoot of the non–weight-bearing leg (NWBL).
- The foot on the NWBL moves behind the stance leg via external rotation of the hip and knee flexion.
- The foot of the NWBL continues to move behind the stance leg with increasing internal tibial rotation.
- Completion of the concentric exercise. The return to the start position provides an eccentric muscle effort.
- Exercise 2: Step task
- In this exercise, the patient has to do a quick loading-unloading step exercise. This means that the exercise will be done as fast as possible, without losing the integrity of the exercise.
- Put the foot of the NWBL posterior and lateral of the stance leg
- Put the foot of the NWBL forward
- Put the foot of the NWBL posterior and medial of the stance leg
- Put the foot of the NWBL forward
- Put the foot of the NWBL sideward of the stance leg
- Exercise 3
- A stepping task performed on an unstable surface.




One Comment