Causes of Edema
Introduction
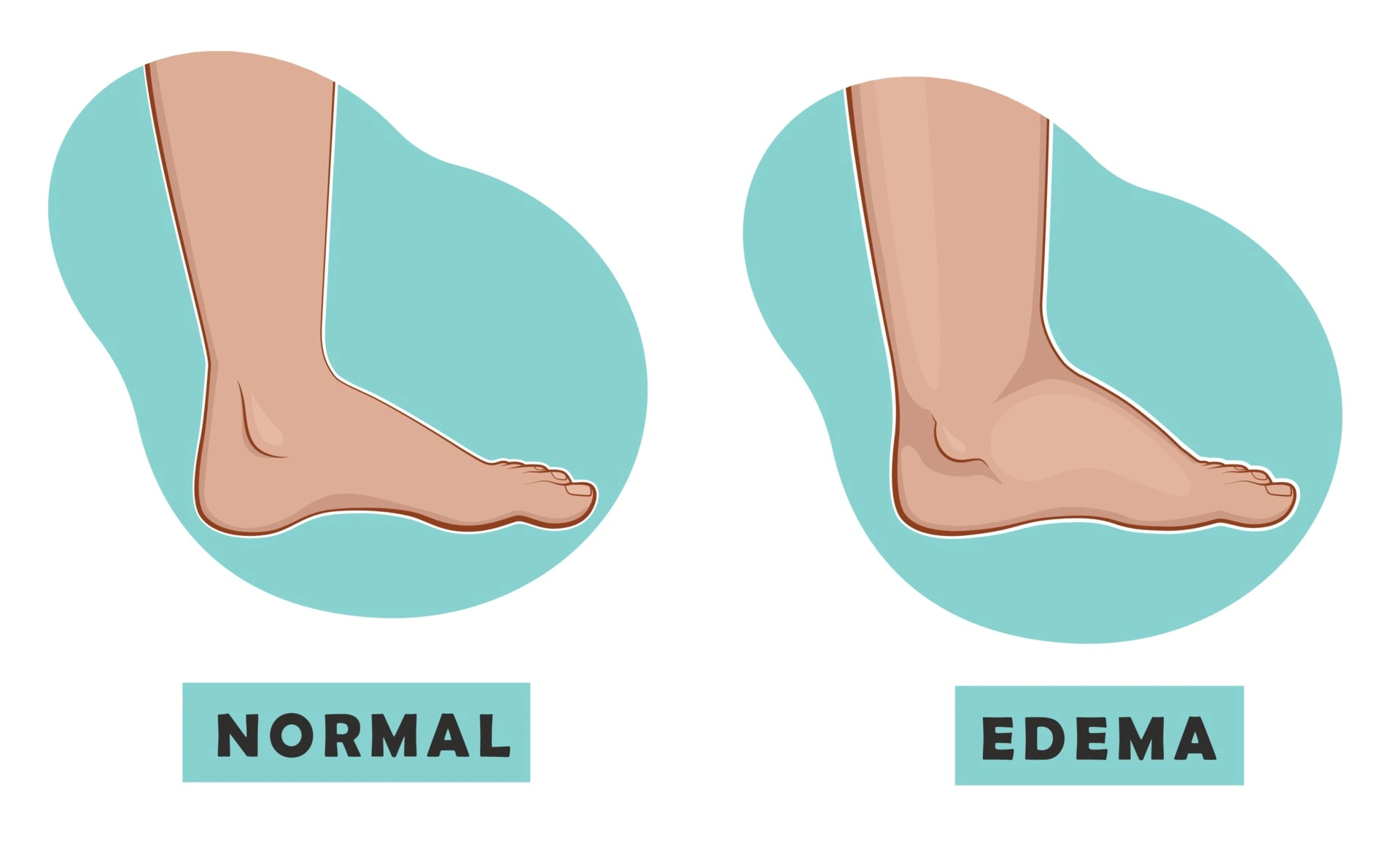
Edema refers to swelling occurring in various parts of the body, most commonly the lower extremities, due to fluid accumulation in the tissues. This excess fluid congestion results from physiological dysfunction that upsets the complex balance within the cardiovascular system and fluid regulation mechanisms in the body.
Edema itself is not a singular disease but rather a condition secondary to a host of potential underlying disease states. Understanding the root causes facilitating edema development is essential for proper diagnosis and treatment.
Causes of Edema
Heart Failure
Heart failure occurs when the heart muscle is too weak to pump enough blood to meet the body’s needs. This reduces blood flow out of organs like the lungs and liver, increasing pressure and causing fluid to leak into surrounding tissues like the legs and abdomen.
Kidney Disease
Chronic kidney disease and conditions like nephrotic syndrome impair the kidneys’ ability to filter wastes and balance electrolytes and fluid. Damaged kidneys cannot properly eliminate excess fluid, leading it to accumulate in tissue and create edema.
Liver Disease
The liver synthesizes albumin and other proteins that exert a strong osmotic pressure in the blood vessels. Liver dysfunction allows the protein to escape into the intestines, reducing blood oncotic pressure. Fluid subsequently leaks out of the vessels into the abdominal cavity (ascites) and lower extremities.
Blood Clots
Deep vein thrombosis in the legs or clots in the superior vena cava obstructs the drainage of blood from the extremities or upper body. The blood backs up and pressure increases, forcing fluid out of the veins into nearby tissues.
Inflammation
Inflammation from immune reactions, infections, burns, surgery, etc. makes blood vessels more permeable so leukocytes can enter tissues. But this also allows protein and fluid to leak into the extracellular space, causing inflammation-induced edema.
Medications
Drugs like corticosteroids, NSAIDs, anti-hypertensives, and immunosuppressants have effects like altering fluid/electrolyte balance, reducing kidney function, and widening blood vessels that can worsen edema.
Venous Insufficiency
Faulty valves inside leg veins allow blood to improperly flow backward and pool in extremities when upright. The pressure and volume stresses push fluid into surrounding tissues.
Low Protein Levels
Reduced blood albumin and globulin in protein-loss states like malnutrition decreases colloid osmotic pressure in the blood. Fluid moves out of the vessels into edematous tissues to equalize concentration gradients.
Pregnancy
Hormonal changes enhance sodium and fluid retention to support increased blood volume. Capillary permeability increases, especially in the lower extremities, allowing fluid to accumulate.
Excess Sodium/Fluid Intake
Ingesting more fluid and electrolytes than the kidneys can excrete strains the organ’s filtering capacity. Excess sodium and water retention worsens edema.
Prolonged Standing
Gravity and hydrostatic pressure from standing upright for long periods displace fluid downward from the bloodstream into the interstitial spaces, leading to lower extremity/ankle edema.
Cancer
Tumors can physically compress veins and lymphatic vessels, hindering drainage and increasing pressure for localized edema. Systemic factors like low albumin also contribute.
Hypothyroidism
Reduced thyroid hormone leads to widespread effects including a depressed cardio-circulatory system. Poor cardiac output contributes to heart failure and fluid imbalances.
Allergic Reactions
Inflammatory mediators released during allergic reactions increase blood vessel permeability, allowing leakage of proteins and fluids into tissues that manifest as edema.
Symptoms of Edema
The primary symptom of edema is observable swelling in various parts of the body, most commonly the limbs and extremities. This can manifest as a puffy appearance, enlarged circumference, or indentation with applied pressure at the swelling site. Other associated symptoms include:
- Tight, stiff, heavy sensation in the affected area
- Aching or cramping
- Decreased flexibility and range of motion
- The shiny, stretched appearance of skin over the swollen region
- Impaired circulation with bluish/purplish skin discoloration
These symptoms tend to gradually develop over time as fluid accumulates, though certain health events can cause rapid onset. Keeping an eye out for swelling onset facilitates prompt treatment to minimize discomfort.
Diagnosis
Since edema represents an outward manifestation of internal processes gone awry, healthcare providers take a systematic approach when evaluating its origin. This includes obtaining a thorough medical history to identify risk factors and narrow down culprit disease areas that may be causing fluid dysfunction. Physical examination documents the extent and location of swelling present, comparing sides of the body for asymmetry.
Part of the diagnostic work-up also involves laboratory tests on body fluid samples. These tests evaluate biomarkers like protein levels, kidney and liver enzyme activity, inflammatory markers, electrolyte/mineral balances, etc. that provide insight into which organ systems are struggling to maintain fluid homeostasis. The analysis includes blood tests, urine analysis, and sampling of fluid directly from swollen areas when applicable.
Imaging modalities can also aid diagnosis by revealing underlying causes like heart failure, blood clots, venous insufficiency, and more. Chest X-rays and leg vein ultrasounds are common first steps.
Other options include CT scans to assess tumors or tissue structure issues and MRI to evaluate heart structural problems that reduce pumping adequacy. Identifying the source fluid issue facilitates rapid, tailored treatment to relieve patient suffering.
Treatment of Edema
The cornerstone of edema treatment involves addressing the underlying condition facilitating fluid accumulation rather than just the swelling itself. Relieving the root cause restores balance to the cardiovascular and kidney systems, allowing proper fluid movement back into circulation.
Diuretics
These medications increase urination to eliminate excess fluid from the body. They act by inhibiting sodium and water reabsorption at different sites of the kidneys. Types include thiazide diuretics, loop diuretics like furosemide, and potassium-sparing variants. Though very effective for reducing swelling, they do not treat the source issue.
Compression Stockings
Special stockings apply gradient pressure, highest at the ankles, to help drain fluid trapped in extremities back into circulation. This also prevents additional backflow into tissues. Gradient compression stockings between 20-30 mmHg or 30-40 mmHg gradient work well depending on severity.
Dietary Changes
Eating less processed sodium-rich foods and increasing foods rich in magnesium, potassium, vitamin B6 and other nutrients needed for fluid balance can significantly aid edema management through dietary means alone. Limiting fluid intake may also assist short term.
Underlying Condition Treatment
Whether heart failure, kidney disease, cancer, or other inciting illnesses, treating the specific disease state is crucial for lasting edema relief by restoring internal balance. This may involve medications, surgery, dialysis, chemotherapy, or lifestyle changes among other interventions tailored to the condition.
Heart Failure
Treating heart failure as the inciting edema centers on medications to reduce fluid overload and improve heart function. Diuretics help flush out excess fluid through increased urination. ACE inhibitors and beta blockers dilate blood vessels and help the heart pump more effectively. In severe cases, mechanical pumps may temporarily support heart function until transplant.
Kidney Disease
Kidney treatment focuses on the specific type of disease present. Medications aid kidney function and regulate fluid balance. Severe disease may require dialysis to filter wastes and fluids until transplant or recovery. Controlling factors like diabetes and hypertension that contribute to kidney dysfunction is key.
Medications
Adjusting dosages or switching medications entirely may alleviate medication-induced edema. Substituting or providing supplements to offset deficiencies is an option.
Inflammation
Anti-inflammatory medications like NSAIDs and steroids help resolve inflammatory edema. Treating infections with appropriate antimicrobials is necessary. Lifestyle changes like weight loss and physical therapy help some joint issues.
Nutritional Deficiency
Replacing deficient proteins, and minerals like thiamine and magnesium through diet changes or supplementation restores normal blood composition. Improving nutrition overall prevents further fluid shifts into tissues.
Physiotherapy
Physical therapy using massage, compression, exercise, and positional changes promotes drainage of swelling in edematous limbs. It also helps strengthen muscles to improve supporting blood and lymph flow long-term.
In most refractory edema cases, recommendations may include medication changes, specialist referral, or escalation to surgical procedures like implanting venous pumps or creating additional lymphatic drainage pathways. Utilizing several modalities often provides edema reduction while managing underlying factors.
How to Prevent Edema?
While individuals with chronic diseases often cannot prevent secondary edema completely, the following methods can help reduce edema risk and severity:
- Eating a diet low in processed foods and sodium
- Consuming a diet low in sodium and processed foods
- Staying adequately hydrated with fluids
- Engaging in regular physical activity to support circulation
- Avoiding prolonged standing/sitting
- Properly managing existing health conditions
- Taking medications as prescribed
- Preventing injuries and promptly treating wounds/infections
- Wearing compression stockings to support venous/lymphatic flow
Making sensible lifestyle choices reduces strain on the cardiovascular system and kidneys, preserving their ability to balance fluid levels. This can decrease the tendency for overflow into tissues leading to swelling episodes. However, edema due to existing illness may still require diligent treatment.
Summary
Edema arises from a variety of diseases and conditions that disrupt the body’s normal fluid regulation in the cardiovascular system, kidneys, liver, and more. The manifestations are visible swelling under the skin, most prominently in the lower legs and feet. Edema itself represents a secondary condition rather than a singular disease entity.
Determining the underlying trigger, whether heart failure, inflammation from autoimmune disease, medication side effects, or renal disorders, is necessary to guide appropriate alleviating treatment. Typical treatment modalities involve diuretic medications, compression garments, dietary changes, and focused therapy for the causative illness. Addressing the source of fluid imbalance facilitates longer-term resolution by restoring homeostasis.
FAQs
What are the most common causes of edema?
The most prevalent diseases causing edema are heart failure, kidney disease, liver disease, blood clots, chronic venous insufficiency, and medication side effects. Inflammatory conditions, nutritional deficiencies, and fluid/sodium excess also contribute.
Where does edema commonly manifest?
Peripheral edema occurs in the legs, feet, ankles, and sometimes hands. Generalized edema can cause swelling in the abdomen, arms, and other areas. Organs like the lungs and brain can also develop edema but have more severe manifestations.
What is the standard treatment for edema?
Loop diuretics, compression stockings, leg elevation, low-sodium diet, and targeted therapy for underlying illness causing the fluid shifts. Draining excess fluid through paracentesis or gentle diuretics relieves swelling.
What causes edema in the legs and feet?
overindulging in salty food; being overweight; being pregnant; and using specific medications, such as antidepressants, steroids, hormone treatment, blood pressure medications, or tablets for contraception.
How can I reduce edema naturally?
Apply pressure. Wearing gloves, sleeves, or compression stockings may help if edema affects an arm or leg. Using the muscles in the swollen area of the body—especially the legs—may help move fluid back toward the heart. Massage. Decrease salt.
References
Edema – Symptoms and causes – Mayo Clinic. (2023, July 28). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/edema/symptoms-causes/syc-20366493
Heitz, D. (2023, December 21). What You Should Know About Edema. Healthline. https://www.healthline.com/health/edema
Hoffman, M. (2009, October 22). What Is Edema? WebMD. https://www.webmd.com/heart-disease/heart-failure/edema-overview
Professional, C. C. M. (n.d.). Edema. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/12564-edema