Diastasis Recti Exercises: Your Guide to a Stronger Core
Generally, diastasis recti exercises focus on strengthening the deep core muscles while avoiding movements that can further strain the abdominal separation. These exercises may include gentle breathing techniques, pelvic floor exercises, and specific core-strengthening movements. In addition to exercise, proper posture and body mechanics are also essential for managing diastasis recti.
Introduction
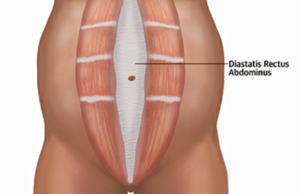
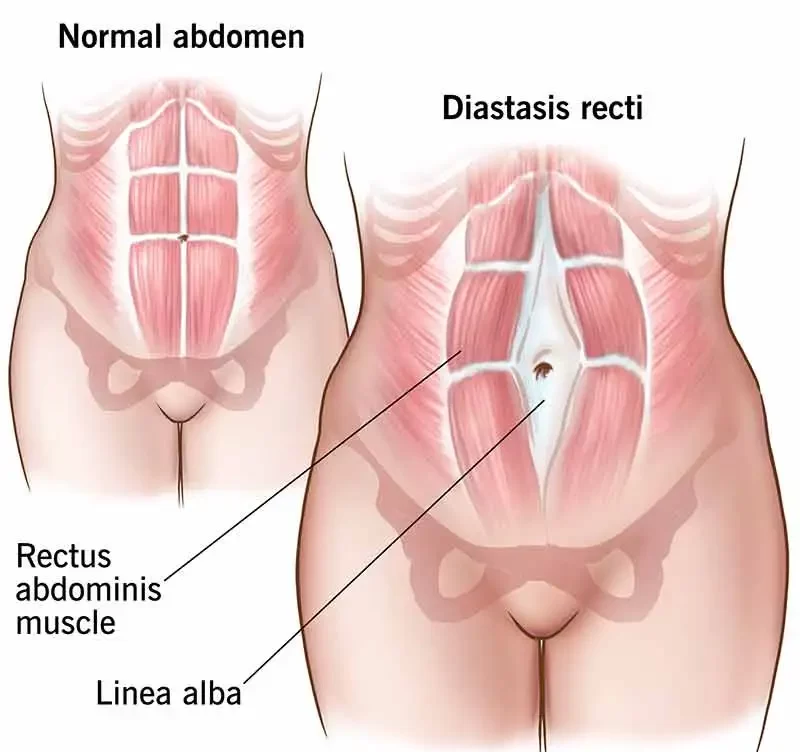
Diastasis recti, also known as rectus diastasis or divarication of the recti, is a condition characterized by the stretching of the linea alba, leading to an abnormal widening of the gap between the two medial sides of the rectus abdominis muscle, resulting in an increased inter-recti distance.
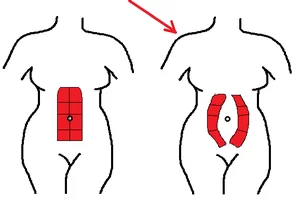
The precise criteria for diagnosing diastasis recti have been a subject of debate, with some experts emphasizing the degree of abdominal protrusion as a defining factor rather than the degree of widening. Nevertheless, a gap exceeding 15-25 mm is generally considered abnormal, taking into account factors such as gender, parity, and the time elapsed since childbirth in postpartum cases. Furthermore, it’s worth noting that the normal width of the linea alba can vary depending on the measurement location, being narrower at the xiphoid region and gradually widening as it approaches the pubic symphysis, with its widest point typically occurring at the level of the umbilicus.
The variation in the degree of diastasis can be attributed to the attachment of the rectus muscles to bony prominences such as the pubic symphysis, as well as muscle attachments from the internal and external oblique muscles. The upper and middle portions of the rectus muscle lack direct bony attachments. In radiographic assessments, the most pronounced diastasis is often observed above, particularly at the level of the umbilicus.
Epidemiology
Diastasis recti is a condition that primarily affects newborns and pregnant women, although it can also occur in men and postpartum women.
Causes of Diastasis recti
The underlying cause of diastasis recti is excessive intra-abdominal pressure. During pregnancy, the abdominal muscles and connective tissues undergo stretching due to the expanding uterus, a process facilitated by pregnancy hormones like relaxin and estrogen. Additionally, the act of pushing during delivery can contribute to the development of diastasis recti. Some degree of abdominal separation is considered normal during and after pregnancy.
In the past, factors such as body mass index (BMI), weight gain during pregnancy, the baby’s weight, and maternal age were believed to be risk factors for diastasis recti. However, a study conducted in 2015 did not find a significant association between these factors and the likelihood of pregnant women experiencing the condition.
In some cases, newborn babies are born with diastasis recti, especially if they are premature. This is because their abdominal muscles are not fully developed and connected at birth. Fortunately, in most instances, this condition resolves itself over time.
Pathology

- In Newborns:
- The rectus abdominis muscle is not always fully developed, and it may not be completely fused at the midline.
- This condition is more frequently observed in premature infants and is somewhat more prevalent among Black newborns.
- In Pregnant or Postpartum Women:
- The expanding uterus exerts significant pressure on the rectus abdominis muscles, leading to stretching.
- Diastasis recti tends to be more prevalent in multiparous women (those who have had multiple pregnancies) due to the repetitive stretching of the abdominal muscles during each pregnancy.
Diastasis Recti Abdominis and Pregnancy
During pregnancy, the linea alba (LA) undergoes softening due to hormonal changes and mechanical stretching caused by the growing fetus. Consequently, there is a gradual increase in the width of the linea alba, also known as Inter-Recti Distance (IRD), throughout the trimesters, with the highest incidence typically occurring in the third trimester.
A recent study conducted by da Mota and colleagues in 2015, which examined 84 first-time pregnant women, discovered that 100% of these women had Diastasis Recti Abdominis (DRA) by gestational week 35, using a diagnostic criterion of 1.6cm at 2cm below the umbilicus. The prevalence of DRA decreased to 52.4% at 4-6 weeks postpartum and continued to decrease to 39% at 6 months.
While this finding aligns with other studies that have also noted a decrease in prevalence at 4 weeks and 8 weeks postpartum, a study conducted by Coldron and colleagues in 2008 reported that the healing process reached a plateau at 8 weeks postpartum. They observed that IRD, as well as rectus abdominis thickness and width, did not return to the control values even one year later.
Diagnosis of Diastatic Recti
In adults, the diagnosis of Diastasis Recti Abdominis (DRA) is typically based on the presence of an increased Inter-Recti Distance (IRD), which is characterized by a visible and palpable separation between the two segments of the rectus abdominis muscle.
There is no universal consensus on what specific IRD measurements are considered pathological. Various parameters have been proposed, including 10 mm above the umbilicus, 27 mm at the umbilical ring, and 9 mm below the umbilicus (for individuals below 45 years of age), and 15 mm, 27 mm, and 14 mm, respectively (for those above 45 years of age). Additionally, some studies have suggested an IRD criterion of >2 mm at 3 cm below the umbilicus, >20 mm at the umbilicus, and >14 mm at 3 cm above the umbilicus as indicative of Diastasis. It’s worth noting that clinical practice may employ various methods for measuring Inter-Recti Distance.
The lack of a universally accepted measurement standard highlights the complexity and variability in diagnosing Diastasis Recti Abdominis.
Physical Therapy Treatment of Diastatic Recti
Abdominal muscles serve a crucial role in maintaining posture, ensuring trunk and pelvic stability, enabling trunk movement, and facilitating respiration.
A study conducted by Gilleard and Brown in 1996 highlighted that structural changes occurring in abdominal muscles during pregnancy can restrict their functionality. This limitation can reduce the abdominals’ ability to provide stability to the pelvis against resistance, both during pregnancy and up to 8 weeks postpartum.
Supporting this finding, research by Liaw and colleagues has indicated a negative correlation between the size of Inter-Recti Distance (IRD) and abdominal muscle function.
In 2018, Hills and colleagues discovered that women with Diastasis Recti Abdominis (DRA) exhibited reduced capacity to generate trunk rotation torque and perform sit-ups. This observation was substantiated by a negative correlation between Inter-Recti Distance and trunk rotation peak torque generating capacity and sit-up test scores.
Several studies have suggested that weak abdominal muscles may contribute to abdominal and lumbopelvic pain and dysfunction during pregnancy.
Additionally, it has been theorized that weak abdominal muscles can lead to ineffective pelvic floor muscle (PFM) contractions.
Initiating exercises during pregnancy can potentially help maintain the tone and control of abdominal musculature, thereby reducing stress on the linea alba.
Early literature indicates that changes in the line of action of abdominal muscles may compromise their functional capacity. Since then, Chiarello and colleagues (2005) have found that the occurrence and size of DRA are more prevalent in pregnant women who do not engage in exercise. Given the critical role of abdominals in exercise, it is essential to screen women for the presence of DRA.
Recent evidence suggests that a program focusing on deep core stability, involving three sessions per week for eight weeks, in addition to bracing, can improve inter-recti separation and enhance the quality of life as assessed by the Physical Functioning Scale (PF10). This program incorporates exercises such as diaphragmatic breathing, pelvic floor contractions, planks, isometric abdominal contractions, and traditional abdominal exercises.
However, an alternative perspective presented by Lee and Hodges in 2016 suggests that simply narrowing the IRD may not be the most effective approach. They propose that pre-activation of the Transverse Abdominis (TrA) can enhance tension and reduce distortion of the linea alba, allowing for more efficient force transmission across the midline.
In contrast, a study by Gluppe and colleagues in 2018 found that a supervised exercise class conducted once a week for 16 weeks, coupled with daily home training, did not lead to a reduction in the prevalence of DRA at 6 months postpartum. This program primarily focused on strengthening the pelvic floor, relaxation, stretching, and the strengthening of the abdominals, back, arms, and thighs.
Patient Education:
Educating patients about diastasis recti abdominis (DRA) during and after pregnancy is essential to manage their expectations, alleviate fear and anxiety, and prepare them for the changes their bodies will undergo during pregnancy and childbirth. Mota and colleagues (2015) have indicated that nearly all women, approximately 100%, will experience an increased Inter-Recti Distance (IRD) in the third trimester, which is characteristic of diastasis recti abdominis. However, the use of terms like “gap” and “separation” when describing diastasis recti abdominis can be highly anxiety-inducing, potentially leading to elevated stress levels in patients. Such stress can have adverse physiological and psychological effects on both the mother and baby.
Therefore, it is crucial to remind patients, whether they are attempting to conceive or are already pregnant, that a woman’s body is naturally designed to expand and accommodate a growing fetus. Pregnancy-related hormonal changes lead to increased connective tissue laxity, which widens the Linea Alba (LA) to create necessary space for the baby. This process is a normal and essential part of pregnancy, providing the baby with adequate room to develop.
In the postpartum phase, patients and physical therapists often focus on managing diastasis recti abdominis to optimize function. diastasis recti abdominis is defined by a pathological increase in the distance between the two rectus abdominis muscles, resulting from stretching, thinning, and/or widening of the Linea Alba.
Consequently, it may seem logical to target a reduction in Inter-Recti Distance as the primary rehabilitation objective, a strategy commonly supported by clinicians who assume that restoring the alignment of the rectus abdominis muscles by decreasing Inter-Recti Distance will also restore muscle function. However, Lee and Hodges (2016) propose that maintaining Linea Alba tension, rather than decreasing Inter-Recti Distance, might be more crucial for supporting abdominal contents and facilitating effective force transfer between opposing abdominal muscles. In individuals with diastasis recti abdominis, reducing Linea Alba tension can lead to a distorted or slackened Linea Alba when Inter-Recti Distance decreases.
On the other hand, pre-activating the Transverse Abdominis (TrA) before engaging the rectus abdominis muscles can increase Inter-Recti Distance while simultaneously increasing Linea Alba tension. Therefore, educating patients about the potential benefits of increasing Linea Alba tension may be more effective in managing and rehabilitating diastasis recti abdominis than solely focusing on closing the “gap” and decreasing Inter-Recti Distance. Such an approach is less likely to optimally support abdominal contents, potentially resulting in a less desirable cosmetic appearance, and could compromise mechanical function.
The video below, created by a Canadian physiotherapist, offers an excellent analogy to explain the concept of diastasis recti abdominis.
Diastasis recti abdominis can impact cosmetic appearance due to the extension and loss of tension in the LA, leading to a bulging of the abdominal wall. This bulging, often referred to as “mummy tummy,” can be observed when women transition from lying down to sitting, engaging in exercise, or even during rest. An increased Inter-Recti Distance is positively associated with worsened body image in women with diastasis recti abdominis. Therefore, it may be advisable to include body image and body satisfaction assessments and management strategies when treating pregnant and postpartum women with diastasis recti abdominis.
There is a growing consensus suggesting that diastasis recti abdominis is not necessarily a condition that physiotherapists and patients need to prevent or treat. Instead, it is a normal aspect of pregnancy, as women’s bodies are naturally designed to create space for a growing baby. However, physiotherapists can prescribe various techniques to help pregnant and postpartum patients maintain and optimize strength and function. Pelvic floor physiotherapists are qualified to develop exercise and movement strategies aimed at promoting optimal physical function throughout pregnancy, reducing the risk of functional impairment, and preparing for childbirth. Furthermore, physiotherapists must engage in open discussions with patients about their concerns, expectations, and goals. This ensures the creation of individualized and targeted management and treatment plans. Tailoring rehabilitation for diastasis recti abdominis and addressing any postpartum concerns is essential, and a comprehensive subjective history, coupled with discussions about expected outcomes and goals, can aid physiotherapists in creating personalized management and rehabilitation plans for each patient.
Effective Postpartum Exercises:
Exercises Targeting the Inner Unit
A comprehensive study by Dufour and colleagues (2019) underscores the importance of incorporating inner unit exercises during various phases of pregnancy and the postpartum period for the management of Diastasis Recti Abdominis (DRA). This aligns with the findings of Mesquita and colleagues (1999), who recommended the initiation of inner unit exercises immediately after delivery. Additionally, a recent investigation by Thabet and Alshehri (2019) highlighted the effectiveness of a deep core stability exercise program, encompassing diaphragmatic breathing, pelvic floor contraction, plank exercises, and isometric abdominal contractions, in treating DRA and enhancing postpartum quality of life.
The inner unit, comprising muscles like the transverse abdominis, multifidus, diaphragm, and pelvic floor muscles, plays a pivotal role in core stabilization. When commencing inner unit exercises, it is imperative to begin by mastering controlled isolation of each muscle within the unit, followed by progressing to coordinated co-activation of these inner unit muscles. During prenatal, early postpartum, and late postpartum stages, it’s crucial to steer clear of exercises that engage the superficial abdominal muscles, such as sit-ups. Once mastery of inner unit isolation is achieved, exercises should evolve to include engagement of the outer unit (a method detailed below) and incorporate functional movements.
- Step-by-Step Inner Unit Exercises:
- Step 1: Tupler Technique – Solo Contraction of Transverse Abdominis Muscle
- Step 2: Add a Posterior Pelvic Tilt to Step 1
- Step 3: Combine Steps 1 and 2, approximating both sides of the abdomen to the center
- Step 4: Add Head Lifting to Step 3
- Transverse Abdominis (TA):
- Patient Position: Begin with the individual lying in a supine crook-lying or side-lying position, maintaining a neutral spine. Instruct the individual to locate their TA muscle by gently palpating it using their index and middle fingers, just medial to their front pelvic bones (ASIS).
- Technique: The individual should then draw in their abdomen and contract their TA muscle while practicing relaxed breathing. Utilize columns like Imagine you are pulling your pelvic bones together in a straightforward line/Bring your belly button towards your spine. Maintain the contraction for 3-5 seconds while exhalation, relaxing during inhalation. Perform 3 sets of 10 repetitions, 3-4 times weekly, ensuring there are no compensatory strategies like posterior tilting of the pelvis, ribcage depression, breath-holding, or abdominal bulging.
- Multifidus:
- Patient Position: Position the individual supine or on their side, maintaining a neutral spine. Ask them to visualize a line connecting the left and right sides of their posterior pelvis.
- Technique: Instruct the individual to contract their multifidus muscles, attempting to bring together their left and right halves along the imagined line. Emphasize relaxed breathing, with the multifidus contracting during exhalation. Hold the contraction for 3-5 seconds, performing 3 sets of 10 repetitions, 3-4 times per week. Ensure there is no anterior tilting of the pelvis, hip flexion, or movement in the thorax or lower back.
- Pelvic Floor Muscles (PFM):
- Patient Position: Supine, crook-lying, or side-lying.
- Technique: Guide the individual to envision closing off their urethra, as if halting the flow of urine. Alternatively, have them imagine lifting their anus toward their pubic bone. As suggested by Diane Lee (2019), another position for isolating the PFM involves sitting on a small, soft ball to provide feedback. Observe the PFM’s movement during deep inhalation and exhalation. A correct contraction should generate a very gentle tension deep in the abdomen without involving the buttocks, leg movements, or spinal and pelvic adjustments. Hold the contraction for 3-5 seconds, perform 3 sets of 10 repetitions, 3-4 times weekly.
- Diaphragm:
- During pregnancy, the diaphragm undergoes upward displacement, approximately 5 cm, to accommodate the growing uterus. This increased workload on the diaphragm can lead to compensatory mechanisms and heightened recruitment of accessory muscles.
- Given these changes, it is advisable to adopt a tension-free diaphragmatic breathing pattern during prenatal, early postpartum, and late postpartum periods. This means that, during inhalation, the diaphragm should descend downward, causing the lateral costal rib cage to expand outward.
- To facilitate this breathing pattern, consider the following exercises:
- Diaphragmatic Breathing:
- Position: Lie supine with knees bent and a pillow under the knees for support.
- Technique: Place one hand on the chest and the other over the highest point of the abdomen. Instruct the individual to breathe into the hand on their abdomen with short, shallow breaths, ensuring that only the abdomen, not the chest, rises. Encourage inhalation via the nose & exhalation via the mouth. Alternatively, prompt the individual to “sniff” into the hand on their abdomen to encourage diaphragmatic breathing. Practice this technique for 5-10 minutes at a time, 1-4 times per day, gradually increasing duration.
- Lateral Costal Breathing:
- Position: Lie supine with knees bent and a pillow under the knees for support.
- Technique: Guide the individual to place their hands on the sides of their ribcage. Instruct them to take a deep breath through the nose, expanding the ribcage into their hands. After inhalation, have the person exhale gradually via their mouth. Practice this technique for 5-10 minutes at a time, 1-4 times daily, gradually extending the duration.
- Diaphragmatic Breathing:
Throughout postpartum recovery and DRA management related to pregnancy, it is essential to encourage modifications in activities, and static and dynamic postures to minimize repeated increases in intra-abdominal pressure (IAP). For example, advise rolling onto one side before rising from bed and using a squatty potty to optimize rectal angles and reduce straining. Once mastery of controlled activation of each inner unit muscle is attained, progression can involve co-activation of the inner unit and functional exercises. Furthermore, postpartum patients should avoid high-impact exercises until 9-12 months postpartum and refrain from exercises that compromise continence mechanisms.
Proper Body Mechanics:
Throughout pregnancy, childbirth, and the postpartum journey, it’s crucial to steer clear of movements that consistently raise intra-abdominal pressure. This precaution is reinforced by the discoveries of Sperstad and colleagues, who found that pregnant women engaged in heavy lifting exceeding 20 repetitions per week faced an elevated risk of developing Diastasis Recti Abdominis (DRA).
Education on posture and body mechanics should encompass various aspects, including:
- Lifting and Carrying: Regardless of the weight of the object, it’s vital to employ effective body mechanics. Encourage individuals to get as close as possible to the object they intend to lift. They should inhale as they grip the object, widen their stance with their knees bent while maintaining a neutral spine, and, as they lift, straighten their knees while exhaling. Ensure they keep their spine in a neutral position when lowering the object.
- Getting Out of Bed: Teach individuals to roll to their side before pushing off the edge of the bed using their top arm. This technique minimizes strain on the abdominal muscles.
- Toilet Use: Emphasize the importance of avoiding excessive straining on the toilet, as it can contribute to increased intra-abdominal pressure.
- Posture Maintenance: Encourage the maintenance of a neutral spine alignment in both dynamic and static postures. When standing for extended periods, suggest placing one foot slightly higher than the other to alleviate pressure on the lower back.
Common Techniques:
- Bed Mobility: To exit the bed, advise individuals to first roll onto their side and then use their top arm to push themselves off the edge. This gentle movement reduces stress on the abdominal muscles.
- Lifting: Whether it involves lifting a light or heavy object, always stress the importance of proper body mechanics. Instruct individuals to follow the steps mentioned earlier, emphasizing proximity to the object and the use of their knees and a neutral spine.
Postural Awareness:
After pregnancy, some women may develop an exaggerated anterior pelvic tilt, thrusting their pelvis forward. This posture can lead to rigidity in the upper lumbar and lower thoracic regions, as well as increased tension in the buttock muscles. Diane Lee describes this phenomenon as ‘back clenching and buttock gripping behavior.’ Before introducing strength-building exercises, it may be necessary to incorporate manual therapy and relaxation exercises to address these issues.
Abdominal Support Options:
While experts caution against relying solely on external support, such as abdominal binding, for Diastasis Recti Abdominis (DRA) rehabilitation, there are instances where it can complement exercises effectively. Abdominal binding can offer additional support and comfort, aiding in cueing and proprioception, especially for women in the early postpartum phase. It can also boost confidence when attempting to activate abdominal muscles. A randomized controlled trial conducted by Cheifetz and colleagues (2010) suggests that abdominal support can effectively manage distress and enhance the overall experience of patients recovering from major abdominal surgery, a finding that may be relevant for DRA patients following cesarean delivery.
It’s worth noting that certain clinical experts recommend using elastic binders rather than non-elastic ones. Non-elastic binders may increase intravesical pressure (IVP), potentially affecting bladder function. Elastic binders, on the other hand, allow for greater mobility and do not impede breathing.
If an abdominal wrap or binding is considered, it should be initiated immediately postpartum and worn for approximately eight weeks or until the patient regains the ability to activate the inner unit during physical activity. It’s essential to combine external support with inner unit activation and exercises to restore control and co-activation of the inner unit muscles. Additionally, when applying abdominal bindings, always start from the bottom and work upwards to prevent increased pressure on the uterus and pelvic organs, which could lead to pelvic organ descent or prolapse. The abdominal wrap should provide gentle compression, as excessive compression can elevate intra-abdominal pressure (IAP).
Recommended Exercises:

- Umbrella Breathing with Kegel
- Start in a standing position with slightly bent knees or sit on a yoga ball or chair.
- Visualize your ribcage expanding like an umbrella opening 360 degrees during inhalation.
- Initiate your exhale by performing a Kegel contraction. Empty your lower belly, then the middle, and finally the chest, engaging your abdominal muscles as you progress.
- Perform 10 focused breaths while standing and continue this breathing pattern throughout the exercises.

- Pelvic Tilts on Hands and Knees
- Start on hands & knees in a neutral spine place.
- Inhale deeply into the sides of your ribcage, then exhale while performing a Kegel, tucking your tailbone down and under to create a curved spine.
- Inhale as you return to a neutral position. Ensure your glutes are relaxed, and focus on moving from your lower abs. Avoid arching your back into the cow position, especially if you have severe diastasis recti.
- Perform 10 tilts, moving slowly and with control.

- Kneeling Leg & Arm Extension with Knee Tap
- Start on hands and knees, exhale, and engage your core muscles.
- While maintaining core contraction, inhale and extend your right arm forward and your left leg straight behind you.
- Exhale as you tap your right elbow to your left knee, then inhale as you lengthen both limbs and return to a neutral position.
- Alternate sides and complete 10 reps on each side.

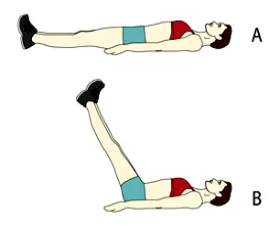
- Toe Taps Lying on Back
- Lie flat on your back with your legs in a tabletop position, and knees directly over your hips. Ensure your back isn’t arched or your pelvis tucked.
- Inhale into your ribcage, and as you exhale, tap your right foot down to the floor, engaging your core and maintaining pelvic alignment.
- Inhale to return to a neutral position.
- Perform 10 reps on each side.

- Single Leg Reach Lying on Back
- Begin in a tabletop position, keeping your pelvis stable. On the exhale, reach your right leg diagonally upward while keeping your pelvis still.
- Inhale as you return to neutral.
- Complete 10 reps on each side.
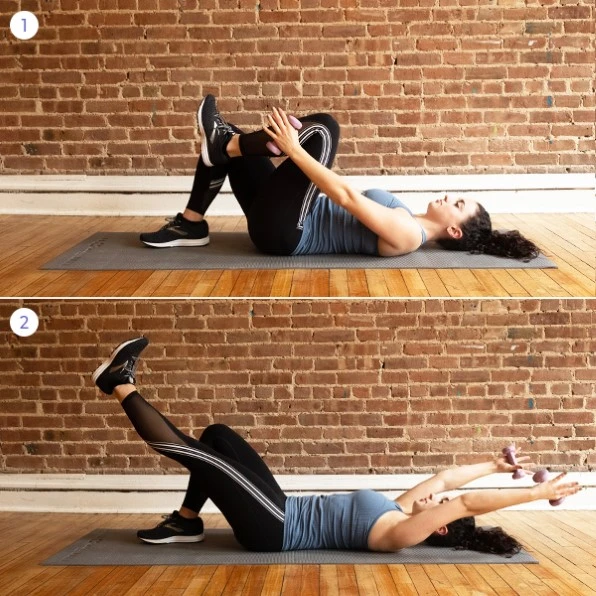
- Leg Extension with Weights
- Start lying flat on your back with feet hip-width apart. Inhale & pull your right knee to the tabletop, with arms bounding your knee.
- Exhale and extend your leg on a high diagonal while reaching your arms slightly overhead, without arching your back.
- Inhale and return to a tabletop.
- Perform 10 reps on each side. Begin without weights and add 1- to 2-pound weights when you feel stable.
- Double Leg Extension
- Once you’re comfortable with single-leg extensions, attempt this exercise without weights initially, then add them if you’re ready.
- Start with both legs in a tabletop position. Inhale while your arms frame your knees, then exhale as you extend your legs on a high diagonal while keeping your back flat and pelvis stable.
- Inhale and return to the starting position.
- Complete 10 reps.

- C-Curving
- Begin in a seated position with your sit bones elevated, feet apart, and hands behind your knees.
- Gently lean backward without rounding your back excessively.
- While leaning back, exhale and pulse backward, focusing on contracting your lower belly.
- Aim for 20 to 30 pulses.

- Side Plank
- Side plank is a suitable alternative to high plank when instructed in a workout class. It can be incorporated throughout your postpartum journey, while high plank and elbow plank should be avoided until you have nearly healed your diastasis recti and have a strong transverse abdominis (TVA).
- Place your elbow directly under your shoulder and stack your top leg in front of the bottom leg, with both feet touching the floor.
- Ensure your shoulders and hips are aligned with your head and feet.
- Continue to breathe and engage your core muscles as you hold this position. Do not exceed 15 to 20 seconds when starting.
Preventing Diastasis Recti
Diastasis recti is a common occurrence during pregnancy, but there are measures you can take to reduce your risk of developing it:
- Maintain Healthy Pregnancy Weight Gain: Ensure you achieve a healthy weight gain during pregnancy by incorporating regular exercise and a balanced diet into your routine.
- Prioritize Good Posture and Deep Breathing: Stand with proper posture, keeping your shoulders back. Practice deep breathing techniques that expand your ribcage rather than solely focusing on your belly.
- Choose Safe Core Exercises: After the 12-week mark of pregnancy and during the postpartum period, steer clear of exercises like sit-ups and crunches, which can exert pressure on your abdominal muscles.
- Lift Safely: Be mindful of everyday activities that involve lifting, such as carrying grocery bags or lifting your children, as they can strain your abdominal muscles.
- Practice the Log Roll: When getting out of bed during pregnancy or postpartum, use the log roll technique. Roll onto your side and utilize your arms to assist you when rising from the bed.
FAQ
Can diastasis recti be corrected with exercise?
Yes, it is feasible to treat diastasis recti without surgery. Rarely is surgery needed to treat diastasis recti. Before using surgical procedures, healthcare professionals may advise physical therapy or at-home activities to assist in healing diastasis.
Can weight loss reduce diastasis recti?
Treatment for diastasis recti is not always as simple as decreasing weight. Surgery for a tummy tuck can fix the problem by removing excess skin and strengthening the underlying muscles.
How can I decrease my belly with diastasis recti?
Abdominal compression: Sit up straight, bend your knees to 90 degrees, and stretch your spine. Hold your stomach in your hands and breathe normally. As you take a tiny breath out, try pulling your pelvic floor and abdominal muscles up and into your spine.
Can yoga heal diastasis recti?
There is no proof that yoga can treat or fix diastasis recti on its own. We have chosen and altered traditional yoga postures and developed sequences that support healthy deep-core muscular engagement without placing undue strain on the linea alba.
Is cycling good for diastasis recti?
Maintaining low impact (brisk walking, cycling, or swimming instead of running or jumping) or learning to control the pressure of impact with good breathing and core engagement as you strive to heal your diastasis recti and get stronger are the keys to safe postpartum cardio exercises.
What is the weakness of diastasis recti?
Diastasis recti is a weakening of the anterior abdominal wall that results in a wider space between the rectus abdominis muscles at the midline. The linea alba is weak, thinning, and broadening, and the corresponding abdominal musculature is weak, according to the majority of experts.
What is the recovery time for diastasis recti?
You can typically resume your regular activities and return to work after up to 6 weeks of recovery following rectus diastasis correction. Additionally, you’ll need to wear abdominal compression clothing throughout this time.
Can diastasis recti heal without exercise?
Surgery is occasionally required to repair a diastasis recti, which is unfortunate. However, corrective workouts have a higher chance of healing a diastasis recti. Prior to considering surgery, I advise following a core restoring program for at least a year. This is also something that many doctors advise.
Reference
- Campbell, D., & Campbell, D. (2022, June 8). Diastasis Recti Exercises for Postpartum Ab Separation. What to Expect. https://www.whattoexpect.com/first-year/your-health/diastasis-recti-exercises/
- Diastasis Recti Abdominis. (n.d.). Physiopedia. https://www.physio-pedia.com/Diastasis_Recti_Abdominis
- Professional, C. C. M. (n.d.). Diastasis Recti. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22346-diastasis-recti