Flexor hallucis longus tenosynovitis and Physiotherapy Management
- Flexor hallucis longus tenosynovitis is sometimes referred to as “dancers tendonitis”, reflecting a patient population that is often afflicted by this ailment.
- However, while FHL tendonitis has historically been described within the context of dancers, especially classical ballet dancers, symptoms have also been reported in others.
- At risk individuals include those who require repetitive forefoot push-off and extreme plantar flexion, such as swimmers, ice skaters, long distance runners, and gymnasts.FHL tenosynovitis classically causes pain at the postero-medial ankle, specifically the region of the fibro-osseous tunnel. Pain has also been reported at the knot of Henry and at the level of the sesamoids.
Flexor hallucis longus tenosynovitis Related Anatomy:

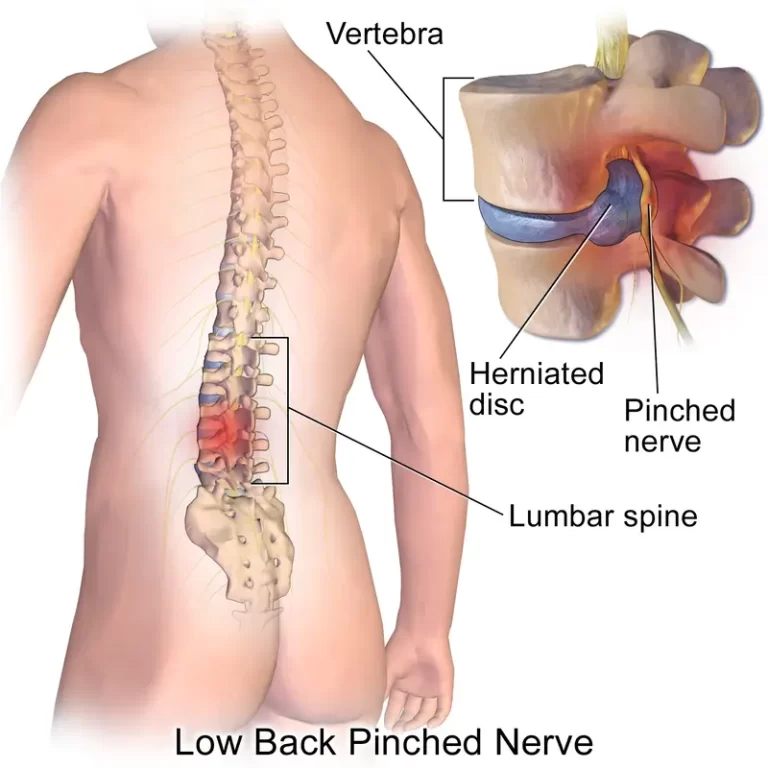
- The FHL originates from the posterior border of the fibula and interosseous membrane of the leg. The FHL passes through the reticular structures at the posteromedial ankle (fibro-osseous tunnel), the plantar midfoot (knot of Henry), and the sesamoids (inter-sesamoid ligament), before inserting at the base of the distal hallucal phalanx.
- At all three of these reticular structures, excessive constriction and abnormal stresses may occur. The FHL is a component of the tarsal tunnel and within the tunnel lies posterior to the neurovascular structures.
- At the level of the knot of Henry, the FHL is dorsal to the medial edge of the plantar fascia. The blood supply to the FHL arises from the posterior tibial and medial plantar arteries, while the tibial nerve provides innervation to the muscle.
Biomechanics
- The primary function of the FHL is to plantar-flex the first metatarsophalangeal (MTP) and interphalangeal joints and to serve as the primary restraint to passive dorsiflexion at the first MTP joint. Moreover, the FHL functions at the ankle-subtalar joint complex, contributing to ankle plantar flexion and subtalar inversion.
- The primary function of the FHL is to plantar-flex the first metatarsophalangeal (MTP) and interphalangeal joints and to serve as the primary restraint to passive dorsiflexion at the first MTP joint. Moreover, the FHL functions at the ankle-subtalar joint complex, contributing to ankle plantar flexion and subtalar inversion.
Flexor hallucis longus tenosynovitis Clinical Presentation
- Patients with FHL tenosynovitis often present with pain at the posterior or posteromedial ankle. However, the site of symptoms can be variable and depends on the anatomic location of the tendon pathology.
- Heel pain, plantar midfoot pain, and first MTP joint pain have all been reported. The proximity of the FHL tendon to more commonly injured structures, such as the posterior tibial tendon (medial ankle), os trigonum (posterior ankle), plantar fascia (plantar midfoot), and first MTP joint (hallux rigidus), may contribute to the delay in diagnosis commonly cited.
- Although pain is the most common presenting symptom, limited MTP joint motion can occur as well. Limited dorsiflexion in the setting of FHL tenosynovitis without first MTP degenerative changes has been coined “pseudo hallux rigidus”.
- Pseudo hallux rigidus is thought to result from nodular tenosynovitis proximal to the fibro-osseous tunnel which limits the excursion of the FHL and thus limits the first MTP joint dorsiflexion. Stenosing tenosynovitis of the FHL at the level of the sesamoids can present as an inability to actively flex the hallux at the IP joint.
Pathogenesis
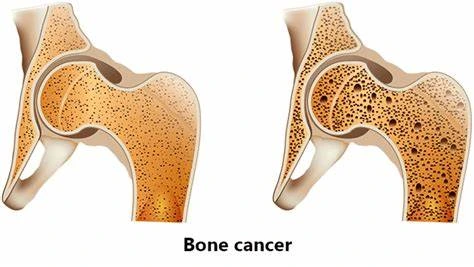
- Pathology includes tenosynovitis, partial longitudinal tears, and nodularity of the FHL due to intra-substance degeneration. While the exact etiology is debated, many authors believe constriction occurs at the fibro-osseous tunnel in the posterior ankle, the knot of Henry in the midfoot, and the inter-sesamoid ligament.
- This pseudo-entrapment induces repetitive microtrauma leading to microscopic and macroscopic tissue damage. Hamilton observed there to be a relative incongruity between the FHL and the fibro-osseous tunnel when the foot is fully plantarflexed, which is postulated to cause abnormal stresses and resultant tenosynovitis.
- Injury at the level of the talus may be due to an abrupt change in direction at this level. Additional etiologies may relate to a low-lying FHL muscle belly or an accessory flexor digitorumlongus.
- Immunohistochemical studies on cadaveric tendons have identified avascular zones where the tendon wraps around the talus and where the tendon traverses the first metatarsal head.
Classification of Flexor hallucis longus tenosynovitis :
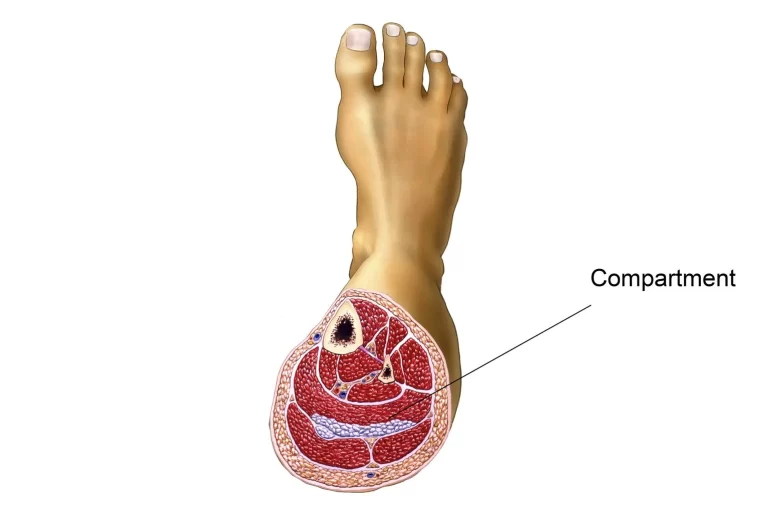
- FHL tenosynovitis can be classified by anatomic zone: zone 1 is posterior to the ankle joint, zone 2 is from the fibro-osseous tunnel underneath the sustentaculum tali to the knot of Henry, and zone 3 is from the knot of Henry to the FHL insertion at the base of the distal hallucal phalanx.
Physical Examination
- The diagnosis of FHL tendonitis can be made primarily by tenderness to direct palpation. Reduced first MTP motion and/or IP motion and triggering of the FHL due to degenerative nodules within the tendon may be present.
- Clinical examination of the FHL includes specific attention to four regions of the foot and ankle: posterior ankle, sustentaculum tali, plantar midfoot, and the level of the sesamoids. During the examination, the ankle and hallux are held in either a neutral or dorsiflexed position to place the FHL under tension.
- Proximally, the muscle belly and the musculotendinous region are palpated just posterior and lateral to the posterior tibial tendon. Medially and inferior to the sustentaculum tali, the FHL can be palpated as it courses through the fibro-osseous tunnel.
- At the medial plantar foot, just plantar to the navicular and medial cuneiform, the FHL can be palpated as it traverses the knot of Henry. Distally, the FHL is palpated as it travels between the sesamoids.
- The FHL stretch test evaluates the influence of the FHL on the first MTP motion; a positive finding is suggestive of “pseudo hallux rigidus”.This test is performed by assessing the first MTP motion in both maximal plantar flexion and moderate dorsiflexion of the ankle.
- To perform the test properly, the first metatarsal (MT) head should be stabilized to prevent compensatory first MT head plantar flexion. A positive test consists of discomfort at the first MTP or a decrease in the first MTP joint motion by 20 degrees with ankle dorsiflexion.
- To assess the effect of the FHL on IP joint motion, place the ankle in a neutral position and stabilize the first MTP joint; limited motion at the IP joint is suggestive of FHL tenosynovitis at the level of the sesamoids.
Imaging related to Flexor hallucis longus tenosynovitis
- Radiographs are obtained to evaluate a bony source of pain. A lateral radiograph can identify an os trigonum.
- Ultrasound can demonstrate fluid within the FHL tendon sheath, swelling of the tendon, and longitudinal split tears. However, ultrasound is less sensitive than MRI, and accurate interpretation requires an experienced user.
- MRI can confirm the diagnosis of FHL tenosynovitis by revealing excess fluid around the FHL at the fibro-osseous tunnel. MRI is a sensitive tool but still may miss pathology such as tendon tears near the knot of Henry.
Conservative Treatment
- Most authors recommend 6 months of non-surgical treatment prior to consideration of surgical intervention. Various treatment protocols have been described and typically involve rest, NSAIDS, immobilization in a neutral position, and gentle stretching.
- The success of non-operative measures has been disappointing with failure ranging from 40-100%.9 One of the more successful non-operative treatment protocols is as follows:
- FHL stretch exercise: The patient stands facing the wall with a book placed under the hallux. While keeping the heel on the ground, the ankle is maximally dorsiflexed by bending the knee. This position is held for 10 seconds and repeated 10 times, with each set of ten being repeated 3 to 4 times daily.
- Immobilization: A walking boot is utilized as a night splint for 6 weeks. If symptoms fail to diminish, a walking boot or short-leg walking cast (extending past the toes) is used full-time (23 hrs/day) for 6 weeks. Both forms of immobilization are used in conjunction with the FHL stretch exercise.
Operative Treatment
- With the failure of non-operative treatment, surgery may be indicated to restore function and minimize pain. Surgical techniques vary depending on the location of the pathology, concomitant injuries, and surgeon preference.
- The goals of all interventions include debridement of the tendon, tenosynovectomy, and treatment of FHL tears. When tendinopathy is located in the posteromedial ankle, the release of the fibrous-osseous tunnel is recommended.
Postero-Medial Ankle
- Medial approach: This surgical approach is advocated by most authors and allows for clear visualization and protection of the neurovascular structures.
- A curvilinear incision is made posterior to the malleolus, following the course of the underlying neurovascular bundle. The neurovascular structures are retracted posteriorly and the fibro-osseous tunnel is then released from proximal to the level of the sustentaculum tali.
- Posterior approach: This approach begins at the lateral edge of the Achilles tendon and proceeds directly anteriorly. The sural nerve is protected and no tendons other than the FHL are manipulated.
- This approach provides excellent exposure to the musculotendinous junction of the FHL, the os trigonum, and the upper aspect of the fibro-osseous tunnel.
- Some authors have expressed concern about a higher risk of tibial nerve injury and increased difficulty decompressing the entirety of the fibro-osseous tunnel.
- Post-op plan: Postoperative treatment for both approaches typically consists of weight-bearing as tolerated in a removable walking boot. Immobilization is discontinued after 2 weeks and activities are increased as tolerated
PHYSIOTHERAPY MANAGEMENT
Pain relieving modalities
- Ultrasound therapy: Ultrasound is a therapeutic modality that generates ultrasound causes deep heat, provides micro-massage to soft tissue, increases flexibility, promotes healing of tissue, and improves localized blood supply to the area. and ultimately pain relief.
- Deep friction massage: Friction is a massage technique used to increase circulation and release areas that are tight; particularly around joints and where there are adhesions within the muscles or tendons. also has a soothing effect that provides pain relief.

- CONTRAST BATH: contrast bath work works on the principle of the combined effect of heat and cold the part alternatively immersed in the hot and cold temperature of hot water ranges from 36c-45c and cold water from 15c -20c.
- treatment begins with hot water and should end with cold water. treatment time varies between 15 to 30 minutes, with immersion in hot water around 3 minutes and in cold water around 1 minute. it relieves the pain.
- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.
FAQ
How do you fix flexor hallucis longus tendonitis?
Take it easy to reduce swelling, and stay away from painful activities. Patients might restrict their foot and ankle motions using crutches, a cast, or a customized boot. To lessen pain and inflammation, use ice and anti-inflammatory drugs such as naproxen or ibuprofen.
How do you treat tenosynovitis of the FHL?
Tenosynovitis of the FHL can be treated by applying ice and non-steroidal anti-inflammatory drugs to the affected region, as well as by resting it. Using techniques like massage, ultrasound, stretching, strengthening, and other techniques, physical therapy can also aid in reducing inflammation.
How long does it take to heal flexor hallucis longus?
Recovery. With rest and conservative therapy for FHL tendonitis, most patients may return to their regular activities in a few weeks. It may take up to three months after surgery to fully recuperate and get back to playing.
How do you treat flexor digitorum longus tenosynovitis?
Pain often subsides after a period of rest for the irritated region. Injections, physical therapy, or surgery may be helpful if the symptoms don’t go away. The tendons and tendon sheaths involved may become inflamed if specific motions or strains are repeatedly performed.
What is hallucis longus tenosynovitis?
Chronic overuse is linked to tenosynovitis of the flexor hallucis longus (FHL) tendon, a disorder that is commonly observed in ballet dancers and occasionally in soccer players. It is regarded as uncommon for this circumstance to have a traumatic cause, such as an ankle sprain.



2 Comments