Gluteus Maximus Enthesopathy
What is Enthesopathy?
The points on bone where tendons or ligaments connect are known as entheses. The word “enthesitis” refers to the inflammation of entheses, although the term “enthesopathy” has a broader definition and can include any clinical conditions connected to these insertions.
Since entheses are areas of high mechanical stress and regularly experience microtrauma, enthesopathy is complex but frequently has a degenerative etiology.
What is Gluteus Maximus Enthesopathy?
Gluteus maximus enthesopathy refers to a condition involving inflammation or damage to the enthesis of the gluteus maximus muscle. It is the attachment site of the muscle’s tendon to the bone, typically around the hip region. Enthesopathy can result from various factors, including overuse, trauma, inflammatory conditions, or degenerative changes. This condition may lead to pain, discomfort, and limited mobility in the affected area, impacting an individual’s daily activities and quality of life.
Proper diagnosis and treatment are crucial to managing gluteus maximus enthesopathy effectively. Medical professionals typically employ a combination of physical examinations, imaging techniques, and potentially conservative measures such as rest, physical therapy, and pain management strategies to alleviate symptoms and promote recovery.
Symptoms of Gluteus Maximus Enthesopathy
Pain, stiffness, and soreness are frequent symptoms of enthesopathy in patients, and activity can make them worse. It typically has a chronic history, can occasionally result in persistent musculoskeletal discomfort, and is linked to localized ossification and calcification.
It might be difficult to accurately diagnose enthesopathy clinically. In order to identify enthesopathy, radiological tests like MRI and ultrasound are quite sensitive.
Degenerative enthesopathy
There are several sources with thorough descriptions of degenerative enthesopathy, in particular:
- Achilles tendon insertion on the calcaneum and supraspinatus insertion on the greater tuberosity of the humerus
- On the lateral epicondyle of the elbow, there is a common extensor origin.
- implantation of the gluteal tendon onto the greater trochanter. This appears as greater trochanteric pain syndrome, also known as trochanteric bursitis, in the hip area.
- There are just a few studies in the literature that examine the CT presentations of gluteus maximus tendinopathy or enthesopathy, which is a rare disorder.
Anatomy
Of the three gluteal muscles, the gluteus maximus is the biggest and most superficial. It helps the thigh to extend and rotate to the side, especially when moving from a flexed to a standing posture (such as when getting up from a chair).
The ilium posterior to the posterior gluteal line, the sacrotuberous ligament, the dorsal aspect of the sacrum, and the coccyx are the sources of the gluteus maximus. Its insertions are completely distinct from those of the gluteus medius and minimus, which attach to the greater trochanter. Maximus muscle fibres have separate tendinous insertions into the gluteal tuberosity of the posterior femur as well as into the iliotibial tract.
The inferior gluteal nerve, which emerges from the sacral plexus, innervates it.
Diagnosis
MRI results in three cases of gluteus maximus enthesopathy with symptoms
The insertion of the gluteus maximus tendon on the posterior femur was thickened and had a noticeable bony spur, according to an MRI. There was no calcification or edoema present. Additionally, neither the other gluteal insertions on the greater trochanter nor the left hip joint underwent any discernible degenerative alteration. After receiving physiotherapy as a conservative approach, the discomfort disappeared.
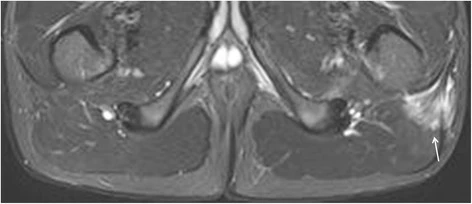
A lucent lesion was seen on plain radiography in the left proximal femur. At first, it was assumed that this was a myeloma metastasis. Body CT and myeloma test, however, came out negative for both diseases. A cortical cyst near the gluteus maximus tendon’s attachment into the posterior femur was discovered on a subsequent MRI, explaining the plain film results. Neither the left hip joint nor the other gluteal insertions on the greater trochanter had any visible signs of degeneration. At the time this article was written, there was no follow-up.
A calcific focus around the proximal femur was seen on plain radiography and was originally mistaken for a chondroid lesion. A further MRI was conducted for additional research. This explained the plain film findings by revealing a thicker, inflamed gluteus maximus tendon with a calcific focus inside it. Neither the left hip joint nor the other gluteal insertions on the greater trochanter had any discernible signs of degeneration. At the time this article was written, there was no follow-up.
Physical therapy
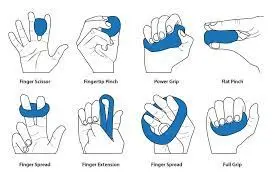
Joint pain and stiffness can be lessened with physical therapy. The majority of physical treatment focuses on increasing flexibility close to the enthesis, strengthening tight muscles, and releasing tension in those muscles. Stretching of the gluteus muscles twice or three times daily, for example, may help persons with hip enthesopathy.
Muscle imbalances, postural issues, and pain exacerbation can be avoided by performing these exercises on both sides, not only the side with enthesopathy. People with enthesopathy can use physical therapy to work around their injuries without making the discomfort worse.
Lifestyle changes
Exercises that put more strain on the joints may need to be avoided by those with enthesopathy. Running and various weight-bearing workouts can aggravate enthesopathy. Non-weight-bearing workouts like riding, swimming, and rowing may be helpful for people who develop enthesopathy. More treatments that could be helpful include:
- Massage the area around the hip joint or the surrounding muscles, using either cold or heat packs on the gluteal region, or alternating the two, to relieve inflammation
- In addition to traditional treatments like acupuncture and corticosteroid injections for inflammatory enthesitis, cool laser therapy (low-level laser therapy) is a type of light therapy that may lessen pain and inflammation.
- It is advised to prevent unpleasant movements as much as possible if at all possible.
Summary
The proximal femur’s lucency and calcification can be seen on plain radiography, which may be mistaken for serious pathology. The gluteus maximus tendon may become thicker, exhibit edoema both within and outside of the tendon, as well as calcification and cortical cysts, according to an MRI.
Gluteus maximus enthesopathy should be taken into consideration as a potential source of symptoms in the thighs and buttocks if the MRI results are favorable, pertinent clinical history exists, and other substantial local pathology is not present.
An uncommon and likely underdiagnosed cause of pain and stiffness in the posterior thigh is gluteus maximus enthesopathy. It could cause the typical thickened gluteus maximus tendon seen on MRIs, either with or without surrounding edema. Additionally, the posterior femur may have cortical erosion or have calcific foci inside the tendon insertion. Although uncommon, it should be taken into account as a potential reason for symptoms in cases of pelvic and thigh discomfort with unknown causes.
FAQs
What is gluteus medius enthesopathy?
Enthesopathy of the gluteal and trochanteric tendons
The gluteus medius tendon experiences additional stress changes as a result of compression. Compression of the distal gluteus medius tendon and adjacent submaximus bursa occurs with hip flexion.
Can enthesopathy be cured?
By treating the source, mild instances brought on by trauma, stress, or overuse can be cured. Your doctor will create a treatment strategy to ease your symptoms if an immune system disorder, such as psoriatic arthritis, is the root cause of your enthesopathy.
Is enthesopathy an arthritis?
Conditions that impair these connecting sites are collectively referred to as enthesopathies. Enthesitis occurs when they become inflamed and uncomfortable as a result of an accident, excessive usage, or illness. Psoriatic arthritis and ankylosing spondylitis are two types of arthritis that frequently cause enthesitis.