Knee Pain around the Kneecap
What is Knee pain around the kneecap?
- Patellofemoral pain syndrome is the term for pain at the front of the knee and around the kneecap. Patellofemoral pain syndrome is also referred to as “runner’s knee.” It is more common in runners and athletes that engage in running and jumping-based sports.
- More often than not, knee discomfort is caused by running, stair climbing, extended sitting, and bending. Simple treatments like ice and deep breathing often help. However, physical therapy may be required for patellofemoral discomfort occasionally.
- Numerous factors could influence patellofemoral development. Overuse from intense sports or training, as well as issues with kneecap alignment, are frequently important causes.
- Conservative measures, such as lowering activity levels or starting a therapeutic exercise program, frequently ease symptoms.
Anatomy of knee pain around the kneecap:
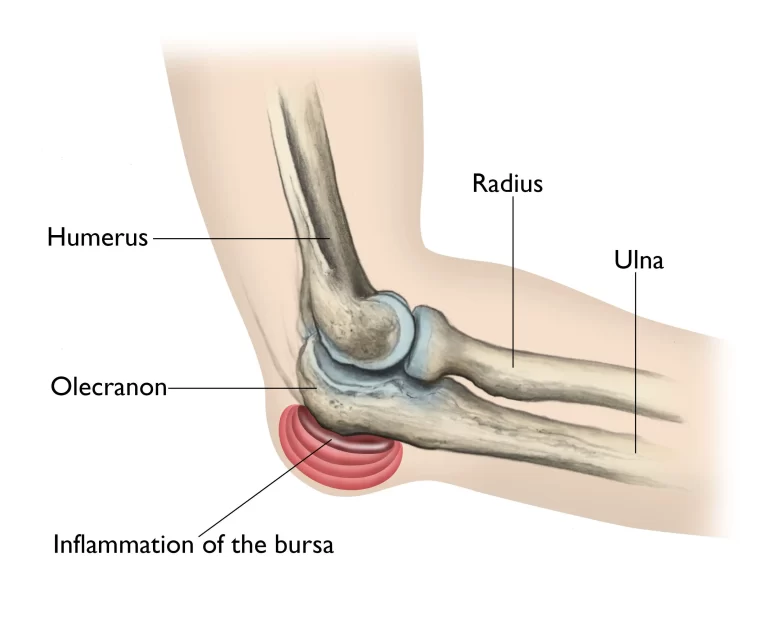
- The largest and most complicated joint in your body is your knee. It is composed of the patella (kneecap), the upper end of the tibia (shinbone), and the lower end of the femur (thighbone).
- The femur is joined to the lower leg bones via tendons and ligaments. The knee’s four major ligaments cling to the bones like sturdy ropes, keeping the bones together.
- Tendons join the muscles to the bones. The muscles on the front of the thigh are connected to the patella by the quadriceps tendon. The patellar retinacula, which are segments of the quadriceps tendon, attach to the tibia and aid in patella stabilization. The patellar tendon extends from your patella to your tibia.
- The knee joint has several components that facilitate movement. For instance, the trochlea, a groove on the top of the femur, is where the patella rests. The patella slides back and forth inside this trochlear groove as you bend or straighten your knee.
- The trochlear groove, the bottom of the patella, and the ends of the femur are covered in a slippery material called articular cartilage. As you move your leg, articular cartilage facilitates the smooth movement of your bones against one another.
- The synovium, a thin layer of tissue covering the joint’s surface, also facilitates movement. A tiny amount of fluid produced by the synovium lubricates the cartilage. Moreover, there is a tiny fat pad directly beneath the kneecap that serves as a shock absorber and cushion.
Symptoms of knee pain around the kneecap:
- Pain at the front of the knee that is dull and painful is the most typical PFPS symptom. This pain can affect one or both knees and typically starts slowly. It is often tied to activities. Additional typical symptoms consist of:
- Pain with physical activity and repetitive knee-bending exercises like running, leaping, climbing stairs, or squatting.
- knee pain in the front that results from extended periods spent sitting with your knees bent.
- Pain resulting from modifications to the playing field, equipment, or degree or intensity of the action.
- Your knee may make popping or crackling noises when you ascend stairs or rise after spending a long time seated.
Causes of knee pain around the kneecap:
There are various reasons for patellofemoral pain syndrome. It has been connected to:
Overuse: Sports involving running or jumping repeatedly strain the knee joint, which can irritate the area beneath the kneecap.
Muscle imbalances or weaknesses: When the muscles surrounding the hip and knee fail to maintain the kneecap’s alignment, patellofemoral discomfort may result. Patellofemoral discomfort has been related to squatting with the knee moved inward.
Injury: Patellofemoral pain syndrome has been related to trauma to the kneecap, such as when the kneecap cracks or becomes misaligned.
Surgery: An increased likelihood of patellofemoral discomfort can result from knee surgery. This is particularly relevant when utilizing a graft of one’s patellar tendon to repair the anterior cruciate ligament.
Patellar Malalignment: An additional possible cause of patellofemoral pain syndrome is aberrant kneecap tracking in the trochlear groove. When the knee is bent in this position, the patella is forced out to one side of the groove. Increased pressure between the trochlea and the rear of the patella due to this anomaly may irritate soft tissues.
The following are some of the factors that result in poor kneecap tracking:
- issues with how the legs should line up between the hips and the ankles. A kneecap that slides excessively to the inside or outside of the leg or that sits too high in the trochlear groove due to alignment issues is referred to as patella alta.
- weakness or imbalance in the muscles, particularly the quadriceps located in front of the thigh. The quadriceps tendon and muscles assist in maintaining the kneecap in the trochlear groove during knee flexion and extension. Inadequate quadriceps strength might lead to inadequate kneecap tracking in the groove.
Risk factors of patellofemoral pain syndrome:
Factors that can increase your risk include:
- Age: Most cases of patellofemoral pain syndrome occur in teenagers and young adults. In elderly adults, knee problems are more frequently the result of arthritis.
- Gender: In women, patellofemoral pain is twice as common as in men. This could be a result of women’s larger pelvises. The angle at which the bones of the knee joint contact is larger in people with broader pelvises.
- Certain sports: Sports involving running and jumping might strain the knees more. This is particularly valid when additional training is added.
Imaging study of knee pain around the kneecap:
- X-rays: Your doctor can typically diagnose PFPS based only on a physical examination. In most circumstances, though, he or she will also request an x-ray to rule out injury to the knee’s skeleton.
- Magnetic resonance imaging (MRI) scans Clear images of the body’s soft tissues, including muscles, ligaments, and tendons, are provided by this kind of research. Your doctor may recommend an MRI if, over some time, your symptoms do not improve with physical therapy and home exercise.
Physical examination of knee pain around the kneecap:
- Your doctor will talk to you about your symptoms and general health during the physical examination. He or she will inquire as to the timing, degree, and type of your knee discomfort (dull vs. sharp). Your physician will also want to know what activities aggravate your pain.
- Your doctor may lightly press and pull on the front of your knees and kneecaps to pinpoint the precise site of the pain. During the examination, he or she can also ask you to lunge, squat, or jump to assess the strength of your knees and core.
- Your doctor may also do certain tests to assist in identifying the source of your discomfort and rule out any additional medical issues.:
- Position of the kneecap and lower leg alignment
- Range of motion of the hips and knees, hip rotation, and knee stability
- The kneecap for any indications of soreness
- The kneecap’s connection to the thigh muscles
- Hip strength, hamstrings, quadriceps, and other front and rear thigh muscles, as well as their flexibility, stiffness, and tone
- flexibility of the feet and the tightness of the heel cord
- Lastly, to assess your gait or the way you walk, your doctor can ask you to walk forward and backward. He or she will search for any issues with your gait that might be causing or aggravating your knee pain.
Treatment of knee pain around the kneecap:
The goals of PFPS medical treatment are to reduce pain and regain strength and range of motion. Patellofemoral discomfort is typically manageable without surgery.
Nonsurgical treatment
Surgical treatment
Nonsurgical treatment:
- Your doctor might suggest the following in addition to activity modifications, the RICE technique, and anti-inflammatory drugs:
- Physical therapy: You can increase your strength, endurance, and range of motion by performing certain workouts. As the primary stabilizer of the kneecap, it is particularly crucial to concentrate on strengthening and stretching your quadriceps. It could also be advised to perform core workouts to strengthen your lower back and abdominal muscles.
- Orthotics: By stabilizing and straightening your foot and ankle, shoe inserts can relieve pressure on your lower leg. Custom orthotics can be manufactured for your foot, or they can be bought “off the shelf.”
Surgical treatment:
- Very seldom is surgery required to address patellofemoral discomfort; it is only done in extreme circumstances where nonsurgical measures fail to relieve the condition. Surgical interventions could involve:
- Arthroscopy: An arthroscope, a tiny camera, is inserted into your knee joint by the surgeon during an arthroscopy. Your surgeon uses the images from the camera to guide tiny surgical instruments on a television screen.
- Debridement: Pain alleviation may occasionally be achieved by excising diseased articular cartilage from the patella’s surface.
- Lateral release: A lateral release operation can be used to repair patellar malalignment if the lateral retinaculum tendon is too tight to pull the patella out of the trochlear groove.
- Tibial tubercle transfer: In certain instances, realigning the kneecap might require repositioning the patellar tendon and a segment of the tibial tubercle, which is the bony protrusion on the tibia (shinbone).
- For this treatment, a standard open surgical incision is needed. To transfer the bone and tendon toward the inside side of the knee, the physician may choose to partially or completely detach the tibial tubercle. After that, screws are used to restore the bone fragment to the tibia. This transfer usually makes it possible for the kneecap to track more accurately in the trochlear groove.
Physiotherapy treatment of patellofemoral pain syndrome:
Strengthening muscles around the knee:
- The muscles that link to the patella and straighten our legs are called quadriceps. The patella may not track correctly when the quadriceps contract if these muscles are not sufficiently strong and coordinated.
- However focusing only on quadriceps strength can put more strain and force on the patella and femur, two components linked to PFPS, thereby aggravating the condition. Mini squats are an exercise that is better for you since they strengthen the quadriceps and other muscles that support your hips and knees. When performing mini squats, it’s important to maintain correct technique and leg alignment; otherwise, the exercise may aggravate knee issues.
Stretching:
- Hamstrings
- Iliopsoas (hip flexors)
- Tensor fascia lata
- Gastrocnemius
Other physiotherapy treatments for patellofemoral pain syndrome:
- foot over-pronation
- generalized joint laxity
- patellar hypermobility
- limb length discrepancy.
Taping:
- K-tape is used to hold the patella in place so it moves in proper alignment with the activity
- enables slightly greater mobility than a brace
- If it lessens symptoms, aids in diagnosis confirmation.
- Several approaches can be used, based on the patient’s preferences or the needs of the activity
Acupuncture:
- Pain modulation
- Help manage tightness in surrounding muscles
Modalities:
Heat, ice, TENS, etc. can all aid in the temporary decrease of pain
Prevention of patellofemoral pain syndrome:
Knee pain can occasionally just appear. However, a few actions could lessen the suffering.
- Build strength: Having strong hip and leg muscles aids in maintaining knee balance during exercise. Steer clear of deep squats when lifting weights.
- Move safely: Consult a physical therapist about proper jumping, running, and turning activities. The muscles surrounding the hips need to be strengthened in particular. This will prevent your knee from buckling inward during squats, leap landings, and step-downs.
- Lose excess pounds: Reducing weight eases knee strain if you are overweight.
- Warm up: Warm up with a little exercise for five minutes or so before running or engaging in any other type of exercise.
- Stretch: Encourage suppleness via mild stretches.
- Build up slowly: Don’t start working out more often all at once.
- Mind your shoes: Put on shoes that are appropriate for the activity and that fit nicely.
Summary
- Patellofemoral pain syndrome is the term for pain at the front of the knee and around the kneecap. Patellofemoral pain syndrome is also referred to as “runner’s knee.” It is more common in runners and athletes that engage in running and jumping-based sports.
- More often than not, knee discomfort is brought on by running, stair climbing, extended sitting, and bending. Simple treatments like ice and deep breathing often help. However, physical therapy may be required for patellofemoral discomfort occasionally.
- Numerous factors could influence patellofemoral development. Overuse from intense sports or training, as well as issues with kneecap alignment, are frequently important causes.
- Conservative measures, such as lowering activity levels or starting a therapeutic exercise program, frequently ease symptoms.
FAQ
Is patellofemoral syndrome likely to disappear?
Up to 90% of patients heal from patellofemoral pain and can return to their pre-painful activities. Most active individuals react well to nonsurgical treatments.
When you have patellofemoral pain syndrome, how do you sit?
Adjust the way you sit, especially the angle at which your knees are bent. offer one knee a rest from its bent position by straightening it out, then switch to offer the other knee the same opportunity to rest. To change positions, you can alternatively slide to the edge of your chair and lower one leg.
How beneficial is walking for patellofemoral syndrome?
By performing stretching and strengthening activities, you can reduce PFPS. He suggests doing five to seven minutes of gentle exercise, such as walking or static cycling, to warm up your muscles first.
How much time does patellofemoral recovery take?
With the right care and rest, patellofemoral syndrome patients can recover totally in as little as 4-6 weeks. But because a runner’s knee is so complex, each person’s primary reason may be different. Developing an individual plan with your physiotherapist might help you heal more quickly.
What is the duration of patellofemoral pain?
Being active may make the pain stronger. Sitting for extended periods might also make it stronger. It might affect one or both of the knees. It may continue for weeks or months.





One Comment