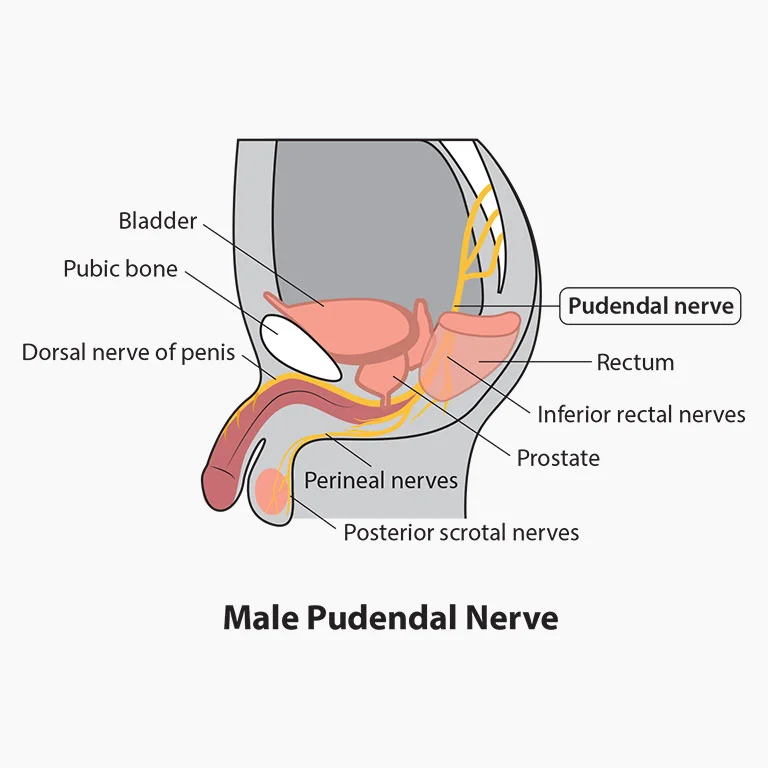
The Pudendal Nerve:
Description
Sacral plexus with Pudendal nerve
The term ‘Pudendal’ comes from the Latin pudenda, meaning “external genitals”, derived from pudendum, meaning “parts to be ashamed of”.
The pudendal nerve is the main nerve of the perineum, pelvic floor muscles & external genitalia. Benjamin Alcock first described it in 1836 while researching the internal pudendal artery’s path & the external genitalia.
The pudendal nerve is a mixed nerve carrying sensory, motor, & autonomic functions. It is one of the primary nerves that arise from the sacral plexus following the sciatic nerve. The nerve is paired, meaning that it is found bilaterally, one on the left & one on the right side of the body.
Course of Pudendal nerve
- This nerve receives input from the primary ventral roots of S2–S4 in the sacral plexus, which connect to form the nerve adjacent to the lateral wall of the pelvic cavity. It then forms one, two, or three trunks before its final branching; variable contributions from S1 & S5.
- Throughout most of its path, the nerve is closely associated with the branches of the internal pudendal artery & vein.
- It then exits the pelvis through the greater sciatic foramen inferior to the piriformis muscle & bends around the posterior aspect of the sacrospinous ligament.
- It runs for a very short distance within the gluteal region where it bends around the sacrospinous ligament to enter the perineum through the lesser sciatic foramen.
- While in the gluteal surface, the pudendal nerve is proximal to the ischial spine where it is the point of a pudendal nerve block.
- Compressive nerve diseases are usually identified at the inter-ligamentous section of its journey, which is when it is dorsal to the sacrospinous ligament & ventral to the sacrotuberous ligament.
- After leaving the lesser sciatic foramen & entering the perineum, the nerve passes through a sheath of connective tissue on the medial wall of the obturator internus muscle called the pudendal (Alcock’s) canal.
- It continues to course through the pudendal canal, giving off three consecutive branches on its path toward the pubic symphysis.
- The pudendal nerve gives rise to the inferior anal nerve immediately after it enters the canal (also called the inferior rectal nerve).
- When it reaches the distal portion of the canal, the nerve bifurcates & gives rise to two more
- branches: the perineal nerve & the dorsal nerve of the penis/clitoris.
- Root value of pudendal nerve
- S2,S3,S4
Branches of Pudendal nerve
There exist three major branches of the pudendal nerve. They are:
Inferior rectal branch
Perineal branch: this is divided into superficial (cutaneous) and deep (muscular) perineal nerve, which further divides into medial and posterolateral scrotal/labial nerve.
Dorsal branch of penis/clitoris
Function of Pudendal nerve
The pudendal nerve consists of 70% somatic fibres (50% is sensory & 20% is motor) & 30% autonomic fibers.
Inferior rectal nerve: carries somatic motor fibers to the external anal sphincter & carries sensations back from the anal canal, inferior to the pectinate line.
Perineal nerve: supplies motor and sensory fibers to the structures in the urogenital triangle, including the external urethral sphincter, the posterior scrotum in males, & the labia minora, vaginal vestibule, lower one-fifth of the vaginal canal & the posterior aspect of the labia majora in females.
Deep (muscular) branch:
In both sexes, it supplies the skeletal muscles of the superficial perineal space (pouch), i.e., the ischiocavernosus, superficial transverse perineal, & bulbospongiosus muscles. Thus, it provides maximal erectile rigidity, ejaculation, & coordinated contractions of all the perineal muscles & pelvic diaphragm.
In either sex, while in the deep perineal space (pouch), the deep perineal nerve innervates the two deep transverse perineal muscles, & more importantly, the external urethral sphincter allowing for the voluntary control of micturition.
In females, the deep perineal nerve also supplies two other skeletal muscles in the deep perineal space: the compressor urethrae & the sphincter urethrovaginalis.
The superficial branch of the perineal nerve carries somatic sensation from most of the skin overlying the urogenital triangle & is called the posterior scrotal or labial nerves.
Dorsal Nerve of the Penis (males) & Dorsal Nerve of the Clitoris (females):
This is uniquely a cutaneous branch of the pudendal nerve & is critical to sexual function since it brings back somatic sensations from the shaft (body) & glans of the penis or clitoris.
This branch is also part of an essential neuropathway in forming erections. Within the lumbosacral spinal cord, the dorsal nerve afferent fibers correspond with the cavernous nerves (carrying parasympathetic axons) which pierce the perineal membrane to supply & encourage the vasodilation of erectile tissue when stimulated.
Clinical relevance
Pudendal nerve block
It is a procedure that comprises injecting a local anesthetic in the proximity of the pudendal nerve. This procedure can help in the diagnosis of pudendal nerve entrapment & can be used for pain relief during obstetric procedures, especially during childbirth in women who are unable to undergo spinal anesthesia.
The block is performed by applying a single injection near to the pudendal nerve to transiently prevent nerve conduction. In these procedures, the ischial spine is used as a landmark to aid in applying the anesthetic in the correct location.
It is also helpful in hemorrhoids, anorectal, vaginal, & perineal surgery, labor, episiotomies, prostate biopsy, prostate brachytherapy, interstitial cystitis, & penile surgery.
Iatrogenic damage to the pudendal nerve
The risk of pudendal nerve injury is of specific importance in obstetrical, perineal, & proctological procedures.
Assessment
History
Common causes of pudendal nerve injury include:
Prolonged sitting (e.g., tailoress, computer operators, judges, concert pianists, locomotive engineers)
Repeated hip flexion (sports activities, exercising, jogging, cycling)
Direct trauma includes falls, motor vehicle accidents, vaginal delivery & pelvic surgeries, especially when using mesh (eg: surgeries for urinary incontinences, total abdominal hysterectomy)
Radiation therapy especially in males treated for prostate cancer & patients treated for rectal & gynecological cancers
Pain Assessment
Patient with pelvic pain (especially perineal & genital) with or without concurrent sexual, bladder, or bowel symptoms
Gradual onset of pain except for acute trauma
Pain is less in the morning & increases with the progression of the day
The type of pain is usually burning pain, but may also experience tingling, aching, stabbing, & shock-like pain
Pain is aggravated while sitting & is relieved when standing, lying down, or seated on a toilet.
Pain distribution may be limited or extensive and may include the vulva, vagina, clitoris, perineum, & rectum in females; glans penis, scrotum, perineum, & rectum in males
Other symptoms associated with PN include urinary frequency, urgency, symptoms mimicking interstitial cystitis, painful ejaculation, dyspareunia, painful nocturnal orgasms, & persistent sexual arousal.
Foreign body sensation
What is pudendal neuralgia?
Introduction
It is a chronic neuropathic pelvic pain that is often misdiagnosed & inappropriately treated by many practitioners. It occurs in both men & women, although studies reveal that about two-thirds of those with the disease are women. The primary symptom is pain in the genitals or the anal-rectal area & the immense discomfort is usually worse when sitting. The pain tends to move around in the pelvic area & can take place on one or both sides of the body. Sufferers describe the pain as burning, knife-like or aching, stabbing, pinching, twisting & even numbness.
Pudendal Conditions- An illustration
Clinically Relevant Anatomy
The pudendal nerve is coupled, meaning there are two nerves, one on the left & one on the right side of the body.
- Nerve roots – S2-S4
Sensory – innervates the external genitalia of both sexes & the skin around the anus, anal canal & perineum
Motor – supplies various pelvic muscles, the external urethral sphincter & the external anal sphincter.
Autonomic – carries sympathetic nerve fibers to the skin of the S2-S4 dermatomal region.
Pudendal nerve entrapment at different levels (ischial spine, sacrospinous, & sacrotuberous ligament, Alcock’s canal) is a cause of disabling, chronic, & intractable pelvic pain that is eminently variable & complex as it is frequently associated with multiple, perplexing functional symptoms.
Pathophysiology
- The exact mechanism of nerve dysfunction & damage is dependent on its diagnosis.
- It can be unilateral or bilateral.
- Causes include compression, stretch, direct trauma, & radiation. Pudendal neuralgia is a functional entrapment where pain happens during a compression or stretch maneuver. The neuropathy worsens due to repetitive micro-trauma leading to persistent pain & dysfunctional complaints. The pudendal nerve is compressed during prolonged sitting & cycling.
- Stretch of the nerve by straining with constipation & childbirth can cause pudendal neuropathy. Fitness exercises, machines, weight lifting with squats, leg presses, or karate with kickboxing & rollerblading are all etiologic factors. Youth sports are a common denominator, possibly related to the bony remodeling of the ischial spine. Driving over uneven roads or farm fields causes vibration trauma. Falls onto the butt can cause pudendal neuralgia
Clinical Presentation
Clinical characteristics include pelvic pain with sitting which increases throughout the day & decreases with standing or lying down, sexual dysfunction & difficulties with urination &/or defecation. To confirm pudendal neuralgia, the Nantes criteria are suggested. The pain sensations are similar to other involvement neuropathies.
In most cases, patients will describe neuropathic pain – a burning, tingling, & numbing pain – that is worse with sitting, & less severe or absent when standing or lying down.
in starting, pain may be present only with sitting, but with time pain becomes more constant & severely aggravated by sitting. Many patients cannot tolerate sitting at all. Interestingly, patients normally report less pain when sitting on a toilet seat, a happening that is believed to be associated with pressure being applied to the ischial tuberosities rather than to the pelvic floor muscles. The pain usually gets progressively worse throughout the day.
What are the diagnostic Procedures for pudendal neuralgia?
Pudendal neuralgia can be very hard to diagnose, as no specific test exists. Therefore, the diagnosis of this condition depends heavily on a proper history & physical examination.
- Diagnostic criteria defined by Robert Nantes are commonly used. Five essential criteria must be present:
- pain limited to the territory of supply of the pudendal nerve
pain predominant during sitting
pain does not waken the patient from sleep
no objective sensory defects
a positive effect of anesthetic infiltration of the pudendal nerve
Objectively these standards determine the baseline function of a patient at the beginning of treatment. Once treatment has begun, the same instrument can be used to determine progress & treatment effectiveness.
- pain limited to the territory of supply of the pudendal nerve
- Professor. Robert Nates Criteria for Diagnosis of Pudendal Neuralgia
- Physical examination focal point on a simple pudendal neurological evaluation. Pinprick sensation is tested at each branch bilaterally: dorsal nerve (clitoris and glans penis), perineal nerve (posterior labia & posterior scrotum), & inferior anal nerve (posterior perianal skin). Hyperalgesia is more common than hypoalgesia. Normal sensation to pinprick might happen even when quantitative sensory testing is abnormal. Pressure is placed on the nerve at the Alcock canal & medial to the ischial spine attempting to reproduce pain, bladder, or rectal symptoms—the Valleix phenomenon.
- MRI helps Pudendal to be classified, based on the involved site:
- Type I, in the sciatic notch
- Type II, the ischial spine & Sacrosciatic ligament
- Type IIIa, the obturator internus muscle
- Type IIIb, the obturator internus muscle & piriformis muscles
- Type IV, the distant branches of the pudendal nerve
result Measures
- Visual Analogue Scale (VAS)
- McGill Pain Questionnaire(MPQ)
- DN4 (which stands for Douleur Neuropathique 4)
- Brief Pain Inventory – Short Form (BPI-SF)
Medical Management
3 main types of drugs are preferred according to symptoms that need to be addressed:
- Muscle Relaxants
- Analgesics
- Anti-convulsants
- Invasive Interventions
- These are performed by experienced practitioners.
Pudendal Nerve Release Surgery. An entrapped pudendal nerve can be requested through 3 different types of surgeries:
- Trans-ischio-rectal (TIR)
- Trans-gluteal (TG)
- Trans-perineal (TP) In some cases, patients may be competent in postoperative pain. In this condition, physical therapy plays a big role in recovery.
- Botox / Botulinum toxin Type A injections
- Pulsed radio-recurrence treatment of the pudendal nerve, sacral nerve roots, or sacroiliac joints
- Cortisone injections
- Activated platelet extract injections (PRP platelet-rich plasma)
- Hyaluronic acid injections
- Neuro-modulation with implantable electrodes
- The selection of applicants for surgery should always include a single diagnostic anesthetic injection of the pudendal nerve, as the fifth of the Nantes basis is an effective predictor of the success of surgery
Clinical treatment depends on the cause of suffering to the nerve. When the cause is not obvious patients are suggested to try the least invasive & least risky therapies initially.
- Non-invasive or Conservative Therapy
- Physiotherapy
- Long term goal is to be pain-free & improves my quality of life.
A physical therapy assessment comprises a movement assessment that will identify poor movement patterns that contribute to the symptoms. frequently, the assessment also comprises a gentle internal assessment of the pelvic muscles. This will provide information about the muscles’ capability to both contract & relax
Treatment includes:
- explanation of pain mechanisms as they related to the patient’s case
- correction of body mechanics, position, or activity moderation
- internal manual therapy to facilitate healthy muscle contraction & relaxation (if applicable)
- Pelvic Floor Relaxation exercises are the most chosen strategy used by physiotherapists, particularly in pelvic floor dysfunction & disorders. A research study, completed by Peter Doran & Michel Coppetiers, two physiotherapists in Australia, reported on a custom for the treatment of the pelvic girdle for pudendal nerve involvement. They had good success with a small group of patients using externally driven techniques to mobilize the sacroiliac joints, decreasing tension on the sacrotuberous & sacrospinous ligaments. This is a non-invasive request that should be considered before more aggressive requests be attempted.
Patient Self-treatment: The patient should use a cushion( Doughnut or C-Shaped) that supports the ischial tuberosities to elevate the pelvic floor off the seat. This support decreases the pressure applied to the pelvic floor muscles & pudendal nerve. dodging of postures or movement which triggers the pain.
Exercises that relax tensed pudendal nerve & will provide temporary relief are:
- Wide leg bridges
- Standing backward leg lifts
- Side-lying hip abduction & extension
- Hip extension in the quadruped position
- Cobra pose
- Arch Backs
Differential Diagnosis
Gender-neutral pathologies: Tarlov cysts, Coccygodynia, Chronic pelvic pain (CPP), Sciatica, Persevering genital activation disorder (PGAD).
In Males: Abacterial chronic prostatitis, prostatodynia, primary proctalgia.
In Females: Vulvodynia, Chronic pelvic pain, Endometriosis, Vaginismus.
Prognosis
The pudendal nerve greatly affects the quality of life but has no effect on life expectancy. Many sufferers report on medical forums & community support groups to have suffered depression & unrelenting discomfort due to the Pudendal nerve which gradually reduced upon the right diagnosis & treatment.
FAQ
What aggravates the pudendal nerve?
Causes of pudendal neuralgia
prolonged sitting, cycling, horse riding, or constipation (usually for months or years) – can cause repeated minor damage to the pelvic area. surgery to the pelvic area. a broken bone in the pelvis. injury to the pudendal nerve during childbirth may be better after a few months.
What might the clinical signs be if the pudendal nerve was damaged?
Pudendal Neuralgiatake place when the pudendal nerve is injured, irritated, or compressed. Symptoms include burning pain (often unilateral), tingling, or numbness in any of the following areas: buttocks, genitals, or perineum (area between the buttocks & genitals).
What can be mistaken for pudendal neuralgia?
Common conditions that could imitate pudendal neuralgia contain coccygodynia, sacroiliac joint dysfunction, piriformis syndrome, ischial bursitis, interstitial cystitis, chronic & non-bacterial prostatitis, prostatodynia, vulvodynia, vulvar vestibulitis, chronic pelvic pain syndrome (CPPS), pelvic floor muscle.
How do you Untrap the pudendal nerve?
Most people with pudendal neuralgia get treatment with a combination of physical therapy, lifestyle changes, & medicines.
Sit up straight & stand more often to help with nerve pain.
Don’t do squats or cycle
Go for physical therapy
Try prescription medication.
How do you decompress a pudendal nerve?
Pudendal nerve decompression surgery is an option that is usually checked out after more conservative therapies fail. These therapies contain such measures as lifestyle changes, pelvic floor physical therapy, medications & nerve blocks.
What functions will be lost with injury to the pudendal nerve?
injury to this branch of the pudendal nerve can result in sexual dysfunction & urinary incontinence. In females, the deep perineal nerve also innervates two other skeletal muscles in the deep perineal space: the compressor urethrae & the sphincter urethrovaginalis.
How serious is pudendal nerve entrapment?
Pudendal neuralgia due to pudendal nerve involvement is a rare neuropathic condition. It causes significant impairment in quality of life, & the pain can become disabling. It often is not correctly diagnosed in starting, so most patients get treated for other conditions, which are normally unsuccessful.
Can pudendal nerve damage cause bowel problems?
The pudendal nerve & pelvic splanchnic nerves are vital to the normal function of the bladder & bowel. Trauma to these nerves can impair communication between the brain & bowel & vice versa, which in turn affects the ability to control feces & urine.


2 Comments