Labral Injury and Physiotherapy Management
- A SLAP tear is an injury to the Labrum of the shoulder, which is the ring of cartilage that surrounds the socket of the shoulder joint.
Anatomy related to Labral Injury
- the Shoulder is a ball-and-socket joint made up of three bones: humerus, scapula, and clavicle.
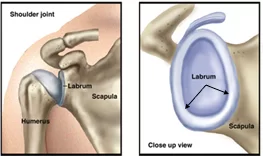
- The head of the humerus bone fits into a rounded socket in the glenoid cavity of the scapula. Surrounding the outside edge of the glenoid is a rim of strong, fibrous tissue called the labrum.
- The glenoid labrum (glenoid ligament) is a fibro-cartilaginous structure (not a fibro-cartilage as previously thought) rim attached around the margin of the glenoid cavity of the scapula. The shoulder joint is considered a ball and socket joint.
- The labrum helps to deepen the socket and stabilize the shoulder joint. It also serves as an attachment point for many of the ligaments of the shoulder, as well as one of the tendons from the biceps muscle in the arm.
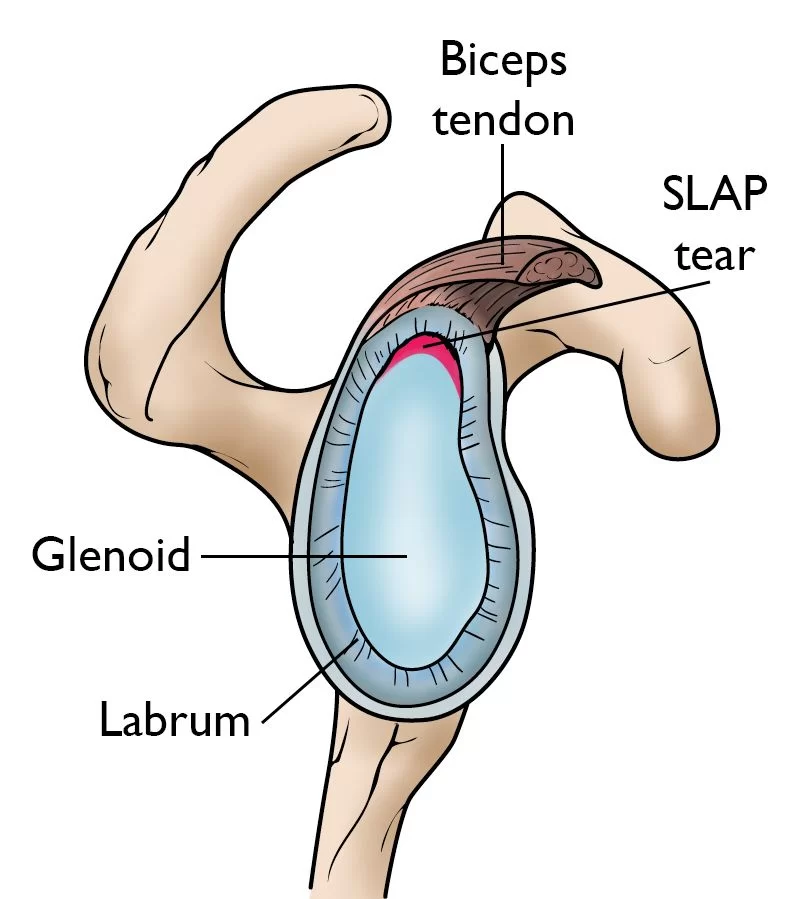
The SLAP lesion
- The term SLAP stands for Superior Labrum Anterior and Posterior. In a SLAP injury, the superior part of the labrum is injured. This top area is also where the biceps tendon attaches to the labrum. A SLAP tear occurs both in the front anterior and posterior of this attachment point. The biceps tendon can be involved in the injury, as well.
Causes of Labral Injury
- Injuries to the superior labrum can be caused by acute trauma or by repetitive shoulder motion. An acute SLAP injury may result from:
- A motor vehicle accident
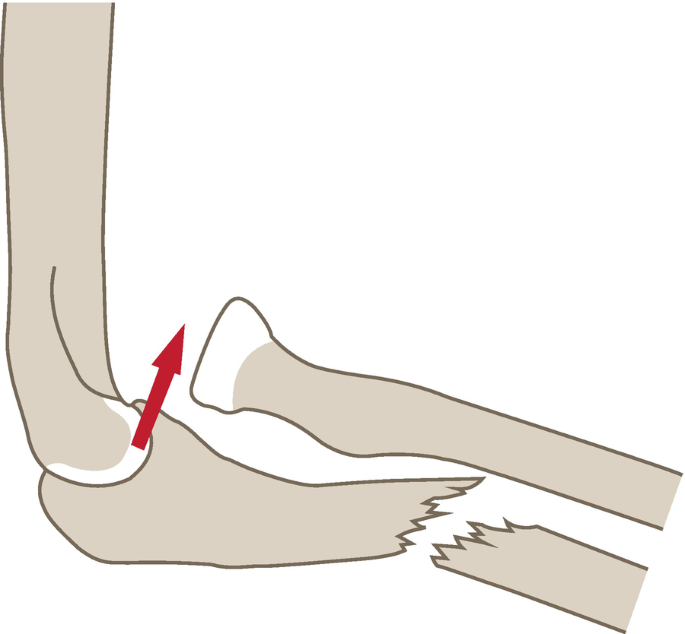
- A fall onto an outstretched hand in the abduction
- repeated overhead activities
- lifting heavy objects
- repeated eccentric biceps contraction
- sudden violent biceps contraction
- Forceful pulling on the arm, such as when trying to catch a heavy object
- Rapid or forceful movement of the arm when it is above the level of the shoulder
- Shoulder dislocation
- the tight posterior shoulder capsule
Symptoms of Labral Injury
- The common symptoms of a SLAP tear include:
- Dull, throbbing, ache in the joint which can be brought on by very strenuous exertion or simple household activity.
- Difficulty in sleeping due to shoulder discomfort. The SLAP lesion decreases the stability of the joint which, when combined with lying in bed, causes the shoulder to drop.
- For an athlete involved in a throwing sport such as baseball, pain and a catching feeling are prevalent. Throwing athletes may also complain of a loss of strength or significantly decreased velocity in throwing.
- Any applied force overhead or pushing directly into the shoulder can result in impingement and catching sensations.
- A sensation of locking, popping, catching, or grinding
- Pain with movement of the shoulder or withholding the shoulder in specific positions
- Pain with lifting objects, especially overhead
- The decrease in shoulder strength
- A feeling that the shoulder is going to “pop out of joint”
- Decreased range of motion
- Pitchers may notice a decrease in their throw velocity or the feeling of having a “dead arm” after pitching.
Diagnosis of Labral Injury
- SLAP lesions are often seen in combination with other shoulder problems and this makes it difficult to diagnose. A SLAP lesion is mostly combined with a lesion of the proximal head of the biceps because it attaches to the superior part of the glenoid labrum. It is associated with pain and instability and an inability of the patient to perform overhead movements.
- biceps tears, and other problems, such as bursitis and rotator cuff tears, are often identified. In combination with SLAP lesions.
- SLAP lesions are difficult to diagnose as they are very similar to those of instability and rotator cuff disorders.
- At first, the clinician can test the tenderness to palpation at the rotator interval which can be helpful in the diagnostic procedure. The rotator interval is an anatomic space between the Supraspinatus tendon, the Subscapularis tendon, and the processus coracoids.
- This rotator interval has a triangular shape in which the supraspinatus is superiorly located, the subscapularis inferiorly, and the processus coracoids medially.
- It contains the coracohumeral and the superior glenohumeral ligament, the biceps tendon and the anterior joint capsule. If you know where these structures are situated, you can try to palpate the rotator interval.
- This can be followed by these tests that are positive when there is a presence of a SLAP lesion: positive anterior drawer, positive apprehension at 90° of abduction and maximal external rotation , and positive relocation test.
- In addition, several special tests can be used to help identify the presence of a SLAP lesion including the Clunk test, the crank test, O’ Briens, Anterior Slide test, Biceps Load I and II test, and the Active Compression test.
- Another very important diagnostic element is the use of clear radiological and arthroscopic images of the labrum, which can help clinicians to distinguish the pathology from normal variation and make the correct diagnosis.
- MRI is the most common imaging tool used to diagnose labral lesions, although it may not show a SLAP lesion. Therefore an MR arthrogram, where a contrast material gets injected into the shoulder, is also used. This is able to detect a SLAP tear better than a normal MRI scan.
- Thus, MRI is more useful than conventional MRI and CT arthrography and is a helpful technique in the diagnosis of SLAP tears. However, there is a great chance of false-positive results due to a superior labral recess or sulcus, which is a normal variant but can make the diagnosis more difficult.
Treatment of Labral Injury
Nonsurgical Treatment
- In most cases, the initial treatment for a SLAP injury is nonsurgical.
- Medical Management
- Nonsteroidal anti-inflammatory medication (NSAIDs). Drugs like ibuprofen and naproxen reduce pain and swelling.
Surgical Treatment
- A doctor may recommend surgery if your pain does not improve with nonsurgical methods.
- The surgical intervention depends on the type of labral lesion, but an advanced arthroscopic technique is most commonly used. Studies of surgical labral repairs show that they are generally good to excellent to allow the patient to return to a pre-injury level of function. Knowing the type of SLAP lesion is important for post-operative rehabilitation.
- Type I: are treated with debridement. Straightforward arthroscopic shaving, without damaging the biceps anchor, is enough for the surgical treatment of this type of lesion.
- Type II: can be treated with arthroscopic fixation of the superior labrum to establish biceps anchor stability.
- The detachment of the superior labrum from the glenoid is recognized as a problematic injury in throwing athletes and others who engage in repetitive overhead activities.
- SLAP lesions are repaired by the use of portals. There are different portals: a posterior portal, an anteroinferior portal, and a mid-glenoid portal. More recently, Nord et al. described the use of the Neviaser portal, a superior medial portal, as the working portal in SLAP repairs. There is no specific portal used for each type a SLAP lesion. The use of a certain portal is determined by a combination of location and the surgeon’s preference.
- Arthroscopy. The surgical technique most commonly used for treating a SLAP injury is arthroscopy. During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your shoulder joint. The camera displays pictures on a video monitor, and your surgeon uses these images to guide miniature surgical instruments.
Physiotherapy Management of Labral Injury
- physiotherapy is the most effective treatment in a SLAP tear, it will provide pain relief in the acute stage while helping to achieve maximum functional mobility with shoulder joint stability.
Goals of physiotherapy
In the acute phase, Physiotherapy treatment will be focused on
- to prevent further damage to tissue
- to relieve pain
- to relieve inflammation
- to maintain an available range of motion
- to maintain muscle strength and endurance
In restoring phase Physiotherapy will be focused on
- to increase the range of motion
- to improve the strength and endurance of muscle
- to gain maximum stability at the shoulder
- to prevent further occurrence
pain-relieving modalities
- SWD: Short wave diathermy produces heat in deeply located soft tissue.it will increase the blood supply to the area and removes the waste product which is one of the reasons for pain. short wave diathermy will reduce pain by sedative effects and it will relax the muscle.
- Ultrasound: Ultrasound is therapeutic modalities that generate ultrasound causes deep heat, provides micro-massage to soft tissue, increases flexibility, promotes healing of tissue as well improves localized blood supply to the area. and ultimately pain relief.
- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.
- LASER: Low-level laser therapy is a form of medicine that applies low-level lasers or light-emitting diodes to the surface of the body. it decreases nerve sensitivity by decreasing bradykinin; a pain eliciting chemical. It normalizes ion channels [cellular gatekeepers] and releases endorphins [body’s natural pain reliever] and enkephalins [related to endorphins] that produce an analgesic effect. It also has a pain-blocking effect on certain nerve fibers.
Physiotherapy inpatient treated conservatively
- patients should avoid any aggravating activities in order to provide relief to the pain and inflammation. If necessary, NSAID’s and intra-articular corticosteroid injections can be applied to help diminish complaints. physical treatment can be started sooner. Strength, stability, and motion are the components of shoulder function that will be focused on during rehabilitation.
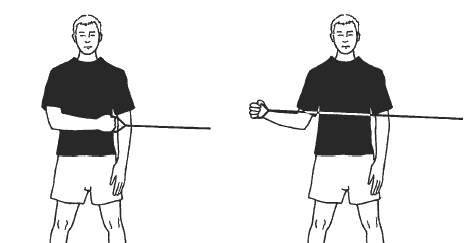
- This course of treatment will focus on restoring the strength of the rotator cuff, shoulder girdle, trunk, core, and scapular musculature, restoring normal shoulder motion, and training to improve dynamic joint stability
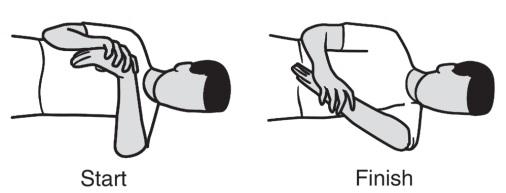
- Regaining GIRD is a crucial aspect of the rehabilitation of SLAP lesions. By the use of posterior capsule stretching exercises, such as sleeper stretch and cross-body adduction stretches, and exercises for scapula stabilization, redevelopment of the internal rotation can be accomplished.
- By stretching the posterior capsule and restoring internal rotation, through posterior capsule stretching exercises, such as sleeper stretch and cross-body adduction stretches, and exercises for scapula stabilization, pathologic contact between the supraspinatus tendon and the posterosuperior labrum.
- can be prevented. The patient is eventually advanced to a strengthening phase, which includes trunk, core, rotator cuff, and scapular musculature. In athletes, a progressive program that is directed toward the patients’ specific sport and position can be initiated after 3 months.
Physiotherapy after surgery
When conservative treatment fails, a surgical approach is in order.
- After surgery, for 3 to 4 weeks, the shoulder of the patient is placed in a sling, which immobilizes the shoulder in internal rotation and leads to a general loss of motion and stiffness. Postoperative rehabilitation is determined by the type of SLAP lesion, the chosen surgical procedure, and other concomitant pathologies and procedures performed.
- Generally, pendulum and elbow range-of-motion exercises are allowed during the period of immobilization. External rotation must absolutely be avoided and abduction limited to 60°. Assisted and passive techniques are used at 4 weeks post-operative to increase shoulder mobility.
- Between weeks 4 and 8, internal and external rotation ROM is progressively increased to 90° of shoulder abduction. Resistance exercises can be initiated at approximately 8 weeks post-operative, in which scapular strengthening should be emphasized. Since the metabolism of cartilage depends partly on its mechanical environment, resistance training can contribute to gaining mobility.
- However, the achievement of adequate shoulder mobility is an important condition to begin resistance training. At month 4 to 6, dependent on the type of sport practiced, patients should be able to start sport-specific training and gradually return to their former level of activity






2 Comments