Stress Fracture on Lower Back
What is a Stress Fracture on the Lower Back?
Stress fractures in the lower back, also known as spondylolysis, represent a specific type of injury that occurs in the vertebrae, the building blocks of the spine. Unlike acute fractures resulting from a single traumatic event, stress fractures develop gradually due to repetitive strain or overuse, often affecting athletes, dancers, or individuals engaged in activities that place repetitive stress on the spine.
- One kind of overuse injury that can happen to young athletes who engage in a lot of repetitive, monotonous exercise is a stress fracture. It differs from a «normal» fracture, which splits the bone in half.
- The phrase refers to a weak part or region of the bone structure where bone tissue degrades more quickly than it can regrow. Early detection of the injury is crucial to avoid a total fracture.
It is believed that 5-8% of the population suffers from this kind of injury. - Men are also three times more likely than women to have it. A stress fracture in the lower back affects up to 50% of young individuals with back pain.
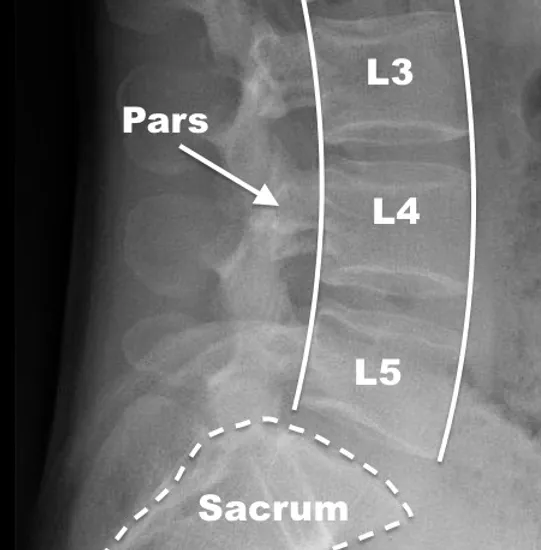
- A spinal deformity or fracture of the pars interarticularis, a bone structure that joins the spine’s facet joints, is known as spondylolysis. Sometimes the illness is referred to by the abbreviations “pars defect” or “pars fracture.”
- The rings of bone that make up the middle and posterior (rear) portions of the spinal column shield the spinal cord. The pars interarticularis, also called the “pars” for short, joins the pedicle and lamina, two other ring components, on either side of the vertebra within each of these rings.
- Instead of being the result of an acute injury, spondylolysis typically develops during childhood or adolescence as a result of repeated stress. Stated differently, it is typically a stress fracture as opposed to an abrupt break.
- Adolescent athletes who perform high-impact stretching and arching landings, like gymnasts, are more susceptible to stress fractures in their backs. For children and teenagers, the most common cause of structural back pain is spondylolysis.
- A prevalent ailment among kids and teenagers participating in organized sports is spondylolysis. Spondylolysis can cause symptoms in active children and teenagers, but it can also go undiagnosed until later in adulthood in some cases.
- The long-held assumption that the illness was inherited or congenital—present from birth—has been abandoned. As was already established, repetitive and monotonous loading of the back is most likely the cause of stress fractures.
- Growing children are especially vulnerable to this kind of injury since their bones have not fully matured. Sports like wrestling, dancing, gymnastics, tennis, rowing, weightlifting, diving, and javelin are the ones where the injury occurs most frequently.
- These sports need a lot of spinal rotation and backward and forward bending. In addition, a stress fracture may develop on the side opposite the primary action. A right-handed tennis player, for instance, could sustain a stress fracture on their left side.
Anatomy
- The 24 little, rectangular-shaped bones that make up your spine are piled on top of one another and are known as vertebrae. A canal formed by the connections between these bones shields the spinal cord.
- The lumbar spine is made up of the five lower back vertebrae.
- The spinal cord and nerves are additional components of your spine: These “electrical cables” transfer messages from your brain to your muscles via the spinal canal: From the spinal cord, nerve roots emerge through the vertebrae’s holes.
- Facet joints: Little joints between and behind neighboring vertebrae help to stabilize the spine and regulate its mobility. The facet joints, which run in pairs down each side of the spine, function similarly to hinges.
- Disks between vertebrae: In between Flexible intervertebral disks make up the vertebrae. These disks have a half-inch thickness and are spherical, flat, and smooth. When you walk or run, intervertebral disks absorb trauma and cushion the vertebrae.
Signs and symptoms
- back pain that gets worse when an athlete is exercising, particularly when they are stretching and rotating their back. Sometimes the discomfort travels down into the buttocks, but it may sometimes be localized to one side. It may sound unusual, but even in the absence of pain or suffering, a stress fracture can occur.
- A pars defect sufferer may have lower back discomfort and stiffness that gets worse with movement and gets better with rest. Because it overloads the pars fracture, hyperextension, or improper stretching, of the lower back typically aggravates the region.
- Nerve symptoms are sometimes possible. These could consist of a leg that feels like it has “pins and needles,” either with or without numbness or weakness
- discomfort in the shoulders, thighs, legs, back, or neck
- weakness or spasms of muscles
- Back tingling, numbness, and/or stiffness
Causes
- Young people who play activities like gymnastics, football, and weightlifting that frequently demand overstretching (hyperextension) of the lumbar spine are more likely to develop spondylolysis or spondylolisthesis. This repetitive motion can eventually weaken the pars interarticularis, resulting in a vertebral fracture or slippage.
- Genetics: All children, adolescents, and adults who walk upright are at risk of developing stress weakness in their lower lumbar spine at the site of a spondylolysis. According to medical professionals, certain individuals may have thinner spinal bones from birth, which could make them more prone to fractures.
Diagnosis
Physical Examination
- The doctor seeing your child will start by obtaining a medical history and inquiring about the overall health and symptoms of your child. They’ll inquire as to whether your child plays sports. Kids who play sports that put a lot of strain on their lower backs are more likely to be diagnosed with spondylolisthesis or spondylolysis.t
- Tender spots
- Restricted range of motion
- Tense muscles
- Weakened muscles
- The posture and gait (the way your child walks) will also be observed by the doctor. Sometimes a patient with tight hamstrings would stand awkwardly or walk with stiff legs.
- A clinical examination alone is not a reliable way for a physician or physiotherapist to diagnose a stress fracture. An X-ray may not reveal the changes in the bone tissue if the pain has just recently started.
- An additional imaging diagnostic technique, such as an MRI, should be utilized to confirm the diagnosis if an injury is still suspected despite the normal X-ray. Any low back pain experienced by a young athlete should raise suspicions about this illness.
- A physical examination, a review of the patient’s medical history, and X-rays—which can identify a pars fracture—are all part of the evaluation process for this illness.
- While an MRI may be helpful to examine the surrounding tissue and disc quality, a CT scan can be used to analyze a pars defect and visualize fixing bone.
- Spondylolisthesis is indicated if the vertebra has moved forward and the fracture gap at the pars interarticularis has enlarged. Your physician will be able to assess the amount of forward slippage with the aid of a side-view X-ray.
- SPECT scans, or single photon emission computed tomography: A tiny quantity of radioactive material is used by a SPECT scan to pinpoint regions with elevated bone activity. A SPECT scan can detect a spondylolysis in situations where CT scans are not accessible. However, there isn’t much purpose for this test anymore.
Treatment
Non-Surgical Treatment
- The majority of people with low-grade spondylolisthesis and spondylolysis will have improvements in their symptoms, including back discomfort, with nonsurgical treatment.
- Among the nonsurgical treatments are:
- Rest: Skipping sports and other activities that strain the lower back for a while can frequently help with symptoms of back pain and other issues.
- NSAIDs, or nonsteroidal anti-inflammatory drugs: NSAIDs that lower swelling and improve back pain include ibuprofen and naproxen.
- Physical therapy: Certain exercises can help strengthen the back and abdominal muscles, increase flexibility, and loosen up tense hamstring muscles.
- Bracing: To restrict spinal movement and give a recent pars fracture time to heal, some patients may need to wear a back brace for a while. Even so, athletes with abrupt Patients who experience sudden or severe pain are eligible for brace treatment; those who have chronic pain are not. Even after wearing a brace for several months, there is little possibility that the stress fracture in these patients will heal.
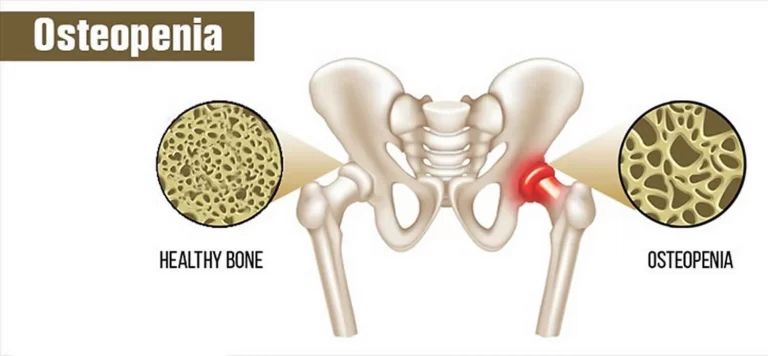
- Blood tests should occasionally be performed on the athlete to check for any nutritional deficiencies. Low calcium and vitamin D levels have an impact on bone density and can raise the chance of stress fractures.
- The athlete’s diet should be modified to guarantee that nutritional requirements are satisfied. This could entail taking supplements.
Surgery
- Adolescents with lumbar spondylolysis may benefit from surgery if non-surgical therapy is ineffective. A sturdy titanium screw can be used to fix the fracture. It’s not a fusion of the spine. A 2- to 3-inch incision is made in the middle of the lower back to perform this procedure.
- By fastening the two sides of the fracture together, the screw applies some compression to the affected area. The repair could then be further supported by the use of a bone graft, which is a portion of bone taken from another part of the body.
- Two hours are spent on the procedure, and then you spend a day in the hospital recovering. For recuperation at home, the majority of teenagers will require one to two weeks away from school. After surgery, there are no exercises for three months. This procedure has a great success rate in curing spondylolysis-related back pain. Most people can resume their prior level of physical activity and sports without experiencing any pain.
- Your child’s physician will take X-rays regularly during treatment to see if the vertebra is moving.
- In essence, spinal fusion is a welding procedure. The main goal is to fuse the damaged vertebrae so that they grow into a single, strong bone. Fusion reduces spinal flexibility and removes mobility between the injured vertebrae. The idea is that a sore spine segment shouldn’t hurt if it is immobile.
- The lumbar spine’s vertebrae will initially be realigned by the doctor during the process. The holes between the vertebrae that need to be fused are then filled with tiny bits of bone, known as bone grafts. The way that a broken bone heals is akin to how the bones grow together over time.
- Your doctor may use metal screws and rods to stabilize the spine better and increase the likelihood of successful bone grafting before implantation
Physiotherapy Treatment
Patients who experience high-grade slippage may also experience compression of the spinal nerve roots. If so, your doctor might first undertake a treatment to release pressure from the nerves and free up the spinal canal, to prepare the spine for spinal fusion.
- Even if the pain goes away during this time, the athlete should refrain from engaging in the activity that resulted in the injury for at least 12 weeks. It takes time for the bone tissue to mend. The athlete can continue to be in shape in the interim by engaging in different, pain-free workouts. Cycling, swimming, and general strength training are a few examples.
- It might be a good idea for some sportsmen to modify their style of play. understand that monotonous and repetitive loading may result in harm. Technique modifications can change the load and lower the risk of damage. Though it normally gets harder as one gets older, young athletes are especially open to modifying their technique.
- Bracing and activity restriction are the first treatments for these kinds of stress fractures, which are then followed by physical therapy.
- Depending on the injuries, age, and the demands of the sport, each patient receives customized care. Every several months, a series of X-rays can be used to evaluate the fracture. Surgery might be necessary if the patient still experiences pain after receiving nonsurgical treatment.
What are the risk factors for spondylolysis?
- Basic human anatomy and upright gait constitute the most fundamental risk factor for spondylolysis. The pars interarticularis is under stress due to the lower back’s inherent inward curvature. Spondylolysis may be more likely in sports where backward bending is required frequently or excessively.
- Football, soccer, and gymnastics are a few examples. Spondylolysis can occasionally occur in young athletes due to overuse and hyperextension of the lower back. For some people, genetics may also be a risk factor.
Summary
- Repetitive stress is most likely to impact this area. Approximately one in every twenty individuals has this illness, making it extremely common.
- Most people with spondylolisthesis and spondylolysis experience no pain or other symptoms, sometimes in a matter of weeks or months. With few consequences or recurrences, the patient can usually gradually resume sports and other activities.
- The doctor might advise your child to perform particular exercises to strengthen and stretch their back and abdominal muscles to help prevent further injuries. Your youngster will also require routine examinations to make sure that issues do not arise.
FAQ
How does a stress fracture in the lower back feel?
back pain that gets worse when an athlete is exercising, particularly when they are stretching and rotating their back. Sometimes the discomfort travels down into the buttocks, but it may sometimes be localized to one side. It may sound odd, but even in the absence of pain or suffering, a stress fracture can occur.
How much time does it take for a back stress fracture to heal?
The bone is still brittle there and may shatter once again as long as you are experiencing pain. A stress fracture typically takes six to eight weeks to heal. While you’re recuperating, cease the activities that resulted in the stress fracture.
How may a lower back stress fracture be treated?
Bracing and activity restriction are the first treatments for these kinds of stress fractures, which are then followed by physical therapy. Depending on the injuries, age, and the demands of the sport, each patient receives customized care. Every several months, a series of X-rays can be used to evaluate the fracture.
Is walking beneficial for stress fractures in the back?
Walking is not an exercise but rather an everyday pastime. Complete rest may be necessary until the pain subsides if it is more severe and interferes with everyday activities. Bracing is rarely necessary or appropriate unless excruciating pain is present.
References
- Spondylolysis (Pars Stress Fracture of the Spine) | HSS. (n.d.). Hospital for Special Surgery. https://www.hss.edu/condition-list_spondylolysis-pars-fracture.asp
- Spondylolysis. (2022, November 18). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/spondylolysis
- Spondylolysis and Spondylolisthesis – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/spondylolysis-and-spondylolisthesis/



One Comment