Intervertebral disc
Definition/Description
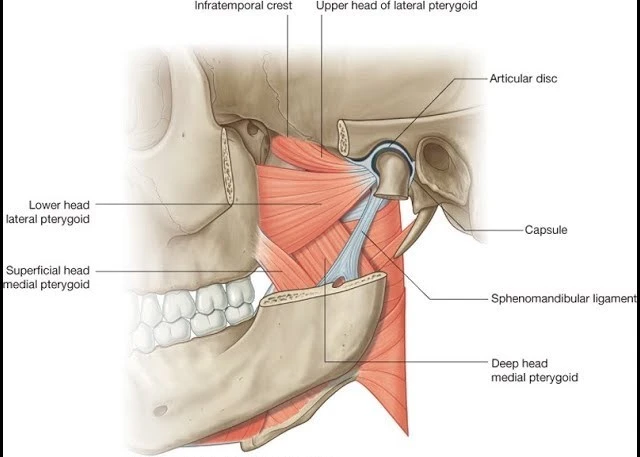
The intervertebral disc (IVD) is important in the usual or typical functioning of the spine or vertebrae. It is a cushion of fibrocartilage and the main joint between two vertebrae in the spinal column. There are 23 discs in the human spine: 6 in the cervical region (neck), 12 in the thoracic region (middle back), & 5 in the lumbar region (lower back).
the intervertebral disc allows the spine to be flexible without offering a great deal of strength. They also provide a shock-absorbing effect within the spine & prevent the vertebrae from grinding together. They consist of three major components: the inner, nucleus pulposus the outer, annulus & the cartilaginous endplates that anchor the discs to adjacent vertebrae.
Anatomy of intervertebral disc
The IVD consists of three distinct components
- A central nucleus pulposus
- A peripheral annulus fibrosus
- Two vertebral endplate
Nucleus Pulposus
- A gel-like structure that sits at the center of the intervertebral disc & accounts for much of the strength & flexibility of the spine. It is made of 66% to 86% water with the difference consisting of primarily type II collagen (it may also contain type VI, IX, & XI) & proteoglycans. The proteoglycans include the larger aggrecan & versican that bind to hyaluronic acid, as well as various small leucine-rich proteoglycans. Aggrecan is largely responsible for maintaining water within the Nucleus pulposus. This structure also comprises a low density of cells. While scattered, these cells produce the extracellular matrix (ECM) products (aggrecan, type II collagen, etc.) & maintain the integrity of the Nucleus pulposus.
Annulus Fibrosus Collagen
- contain “lamellae” & concentric layers of collagen fibers. The fiber orientation of each layer of lamellae alternate & therefore allows effective resistance of multidirectional movements. The Annulus fibrosus consists of an inner & an outer portion. They differ primarily in their collagen composition. While both are primarily collagen, the outer annulus contains mostly type I collagen, while the inner has mainly type II. The inner annulus also contains more proteoglycans than the inner.NB collagen Type I: skin, tendon, vasculature, organs, bone (the main component of the organic part of the bone) Type II: cartilage (the main collagenous constituent of cartilage & is more flexible)
- Vertebral Endplate
- An upper & a lower cartilaginous endplate (each about 0.6–1 mm thick) cover the superior & inferior aspects of the disc. The endplate allows diffusion & gives the main source of nutrition for the disc. The hyaline endplate is also the end part of the disc to wear through during severe disc degeneration.
- Plates of cartilage that bind the disc to their particular vertebral bodies.
- Each endplate covers almost the whole surface of the adjacent vertebral body; only a narrow rim of bone, called the ring apophysis, around the perimeter of the vertebral body is left exposed by cartilage.
- The portion of the vertebral body to which the cartilaginous endplate is applicable is referred to as the vertebral endplate.
- The endplate covers the nucleus pulposus in its whole; peripherally it fails to cover the entire extent of the annulus fibrosus.
- The collagen fibrils of the inner lamellae of the annulus enter the endplate & merge with it, resulting in all aspects of the nucleus being circumscribed by a fibrous capsule.
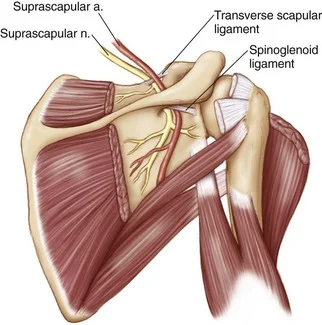
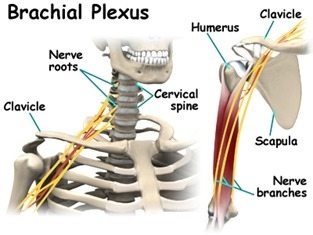
Innervation
The disc is supplied in the outer few millimeters of the annulus fibrosus
- Only the outer third of the AF is vascular & supplied in a non-pathologic state. In aging & states of inflammation, both nerve growth & granulation tissue growth are stimulated. Additionally, the granulation tissue produces inflammatory cytokines, which further increase sensitivity to pain sensations
Vascular Supply
- The Intervertebral disc is largely avascular, with no major arterial branches to the disc The outer annular layers are supplied by small branches from metaphysical arteries. Only the outer annulus is vascularized. Blood vessels near the disc-bone junction of the vertebral body as well as those in the outer annulus supply the Nucleus pulposus & inner annulus. Glucose, oxygen & other nutrients reach the avascular area by diffusion. The same process removes metabolites.
Vital functions
Restricted IV joint motion.
Contribution to stability.
Resistance to axial, rotational, & bending load.
Preservation of anatomic relationship.
It gives cushioning for the vertebrae & reduces the stress caused by impact.
They work as shock absorbers for the spine.
They help protect the nerves that run down the spine & between the vertebrae.
Biomechanics
Weight-bearing: The disc is subjected to various loads, including compressive, tensile & shear stresses. During compressive loading, hydrostatic pressure develops within the NP, which thereby disperses the forces toward the endplates as well as the Annulus fibrous. This mechanism slows the rate applied loads are conveyed to the adjacent vertebra, giving the disc its shock-absorbing capabilities.
Movement: The disc is also involved in allowing movements between vertebral bodies, which include:
Axial compression/distraction;
Flexion/extension;
Axial rotation;
Lateral flexion.
Nuclear migration: Asymmetric compressive loading disc can cause the Nucleus pulposus to move in a direction opposite to the compression. For example, during forward bending (or flexion) of the lumbar spine, the Nucleus pulposus moves posteriorly or backward. opposite, during backward bending (or extension), the nucleus is compressed anteriorly or forwards. This impression is known as the dynamic disc model. Although Nucleus pulposus migration has been shown to behave predictably in asymptomatic discs, a variable pattern of migration occurs in people with symptomatic &/or degenerative Intervertebral discs.
Physiologic Variants
Disc thickness generally increases from anterior to caudal. The thickness of the discs as related to the size of the vertebral bodies is highest in the cervical & lumbar area. This return to the increased range of motion found in those regions.
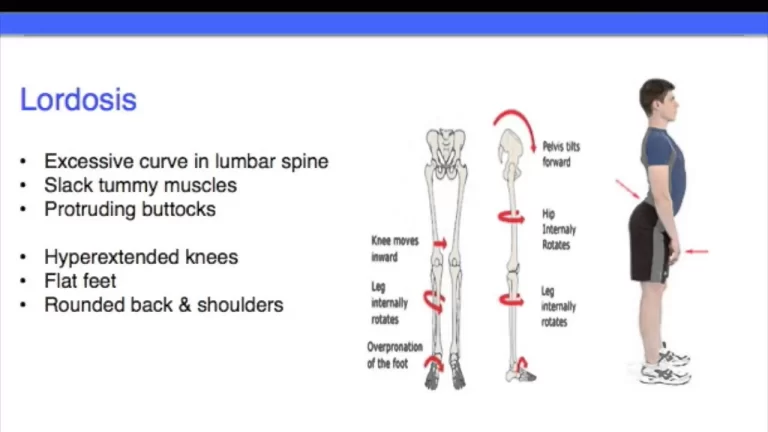
In the cervical & lumbar area, the intervertebral discs are thicker anteriorly. This creates the secondary curvature of the spine – the cervical & lumbar lordoses.
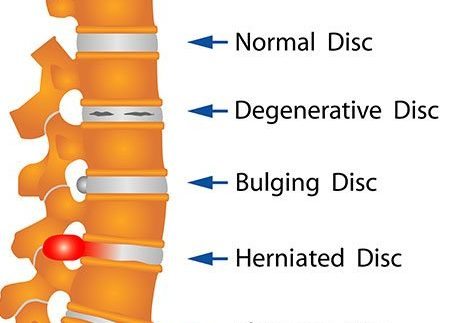
Pathology of Intervertebral disc
There are several terms to express disc pathologies
- Disc bulge – slip disc i.e the circumference of the disc extends behind the vertebral bodies.
- Disc herniation involves the Nucleus pulposus. Disc herniation is significant in that it might compress an adjacent spinal nerve. A herniated disc impinges upon the nerve related to the inferior vertebrae (e.g., L4/L5 herniation affects the L5 nerve root). The most common site of disc herniation is at L5-S1, which may be due to the thinning of the posterior longitudinal ligament towards its inferior end
There are three subtypes of herniations:
- Disc protrusion is described by the width of the base of the protrusion being wider than the diameter of the disc material that is herniated.
- In disc extrusion, the AF is damaged, allowing the Nucleus pulposus to herniate behind the normal bounds of the disc. In this case, the herniated material constructs a mushroom-like dome that is wider than the neck linked to the body of the Nucleus pulposus. The herniation might extend superior or inferiorly relative to the disc level.
- In disc sequestration, the herniated material separated from the body of the Nucleus pulposus.
Disc desiccation is common in aging. It is brought about by the death of the cells that produce and maintain the ECM, including proteoglycans, like aggrecan. The Nucleus pulposus shrinks as the gelatinous form is replaced with fibrotic tissue, reducing its functionality, & leaves the Annulus fibrosus supporting additional weight. This increased stress leads the Annulus fibrous to compensate by increasing in size. The resulting flattened disc decreases mobility & might impinge on spinal nerves leading to pain & weakness. It is thought to be due to proteoglycan breakdown, which decreases the water-maintaining properties of the Nucleus pulposus
Symptoms of disc problems
The symptoms of a provoked disc can vary according to its location & severity. Back scans are frequently unhelpful
for deciding whether a person’s back pain starts from a disc issue, as discs change with aging & with
use. However, symptoms may include:
- back pain
- increased back pain when repetitively forward bending or with prolonged sitting
- increased back pain with coughing, sneezing, laughing, or straining
- pain, numbness, or pins-& needles radiating into an arm or leg if a disc has caused irritation of a nearby nerve.
Risk factors for disc problems
Some people are more susceptible to disc troubles than others. Risk factors include:
elevated body mass index (e.g. obesity)
- elevated body mass index (e.g. obesity)
- lack of fitness
- lack of regular exercise
- cigarette smoking
- older age
- poor posture
- diabetes
- lifting heavy loads.
- frequently, however, disc changes develop without a recognizable risk factor.
Types of Intervertebral disc problems
Common disc-related problems include:
disc strains & sprains
degenerative disc disease (which can also be present in people who do not have any symptoms)
protruded discs (also known as ‘herniated’, ‘prolapsed’, ‘extruded’, or ‘slipped’ discs). For some people, protruding
discs can cause nearby nerve irritation & result in sciatica (nerve pain spreading into the lower limbs).
Disc strain
Disc strain happens like any strains or sprains in other areas of the body. Applying sustained or excessive load to
any soft tissues of the body (like ligaments, tendons, or muscles) can cause pain. If the force & load is more
than the soft tissue can manage with it, it may cause irritation & inflammation. This might not show on x-rays or
scans.
The discs of a young child are plump & moist (fluid-filled & well-hydrated). But the water content of discs
decreases with age until they are comparatively thin & hard. This normal aging process is thought to increase
friction between the bones, resulting in growth around the discs. These are called bone spurs.
recurrent these age-related changes do not cause problems, but some people can experience pain. These changes
are also called ‘degenerative disc disease. The most general symptom is back pain which can be aggravated by
activity or prolonged sitting. It’s recurrent thought to be the most general cause of back pain in older people.
Disc protrusion
- A ‘slipped disc’ is an incorrect term still sometimes used to describe a disc protrusion. It proposes a disc that has
- evacuated out of position, but this is not the case. Discs are held strongly in place by ligaments, muscles & the vertebrae themselves.
- Terms like ‘protruded’, ‘herniated’, ‘extruded’, ‘bulged’, and ‘prolapsed’ better describe the situation. The
- problem is not that the entire disc ‘slips’ out of place but that a small area in the resilient outer disc shell weakens.
- This permits the soft jelly-like contents to exude. When this ‘jelly’ comes into adjoining with other structures,
- especially nearby spinal nerves, it can cause:
- referred nerve pain (pain radiates to the lower limbs)
- altered nerve function (numbness & pins-&-needles).
- The most common site for disc protrusion is in the lower back, & lower backache can be a symptom. As we
- get older, we are at low risk of disc protrusion. This is because the discs dry out & the contents are less able
- to exude through any impaired areas in the outer disc shell.
Sciatica
Sciatica is nerve pain caused by provoke of the sciatic nerve. The pain radiates from the spine & down into
the buttock, back of the thigh, leg, and sole of the foot. Sciatica is frequently associated with altered nerve function. It might cause an altered sensation in the affected lower limb, such as pins-& needles or numbness.
Disc protrusion is a common cause of sciatica. The spinal nerves normally have room to slide up & down
inside the spinal column whenever the body moves. However, a disc bulge can cause mentioned lower limb pain by
protruding into the spinal column & compressing against spinal nerves. This hampers their movement. If the
bulging disc leaks some of its contents around the nerves, which can cause local chemical irritation or
inflammation.
Diagnosis of Intervertebral disc problems
The diagnosis of disc problems involves:
taking a medical history to:
determine predisposing risk factors & conditions
identify any associated spinal nerve involvement
doing a physical examination.
Investigations are carried out if:
• symptoms preserve for more than six weeks despite remaining active, or
• there is anxiety the disc is affecting a spinal nerve.
Treatment for Intervertebral disc problems
Most disc problems will settle with time, regardless of treatment, just like soft tissue sprains in other parts of the body. Short-term bed rest for a few days might help in the starting management of severe sciatica. However, most people can stop active, with some restrictions, according to their level of pain. Appropriate pain relief & allowing the person to stop active within their pain limits is normally the best approach.
- Some treatments used for pain relief include:
- heat treatment (for example heat wraps or hot packs can help to relieve the pain)
- gradually increasing activity levels within pain limits
- an exercise program planned to improve strength, flexibility & fitness
- a short-term (less than 12 weeks) trial of massage, spinal mobilization, or manual therapy
- non-steroidal anti-inflammatory drugs (NSAIDs) or steroids
- pain-relieving medications, like paracetamol.
- Sciatica pain might be treated with an injection of anti-inflammatory steroids into the area of the affected spinal nerve. In severe cases of sciatica caused by a large disc protrusion, the pain might be relieved by surgery to cut the protruding disc. This might be done to relieve pressure on the affected spinal nerve.
- In severe cases of degenerative disc disease, surgery might be considered to remove the disc & fuse together the two vertebrae on either side. However, severe cases of both sciatica & degenerative disc disease are rare. Remember, most disc problems settle without specific treatment.
Self-help for disc problems
With time, most disc protrusions heal themselves & decrease in size. Ongoing self-management strategies might help decrease the future risk of further disc problems. Be guided by the doctor or health professional, but general suggestions include:
- try to avoid a sedentary lifestyle
- avoid lifting objects that are too heavy for you
- remember that movements such as bending & twisting (especially at the same time) can increase pressure & load on discs
- if you find that certain postures bring on the pain, you may need to address issues related to posture while sitting, standing & walking
- to try to maintain good overall physical fitness. This means staying physically active & maintaining good levels of muscle strength in the arms, legs & trunk. Regular exercise to improve flexibility can improve mobility & help decrease muscle tension & back pain
- do a program of back-strengthening exercises
- doing Pilates, walking regularly, or doing tai chi or yoga might help improve strength & flexibility in people with back problems. So, find an exercise that you enjoy & can do regularly which can help to improve your strength.
Other reasons for back pain include:
- muscular pain – this is common, & normally does not spread into the legs. It is very likely to solve out on its own without the need for specific treatment
- fracture-take place more commonly in older people
- people with osteoporosis– people taking medications that cause bone loss (like steroids, anti-seizure, or epilepsy medications).
- Fractures can also take place after direct injury or trauma to the back (for example, due to a motor vehicle accident or road traffic accident )
- cancer – some cancers can lead to back pain.
- strong pain
- persistent pain
- night pain
- unexpected weight & appetite loss
- a history of a cancer diagnosis in another part of the body
- any other symptoms that concern you
- infection – can take place after invasive procedures (such as surgery or dental work). It might also arise in people who are immune suppressed or inject improper drugs. Symptoms that should be rapidly assessed by a doctor include:
- strong pain
- night pain
- fevers
- sweats
- fatigue
Ankylosing spondylitis – causes a gradual onset of persistent back pain & stiffness that is worse in the morning. It normally affects young men more than women. Pain is typically relieved by movement & activity, not rest. It frequently causes overnight pain & sleeps disturbance. If you have this pattern of back pain, visit the doctor for a referral to a rheumatologist
- for scoliosis –which is the increased curvature of the spine. Children & adolescents with scoliosis should visit their doctor for a referral to see a spinal surgeon experienced in assessing & managing scoliosis (particularly if it is getting worse). These specialists generally work in children’s hospitals.
- Scoliosis may:
- be present from birth
- occur due to a person having increased soft tissue elasticity (‘hypermobility’)
- develop with increasing age.
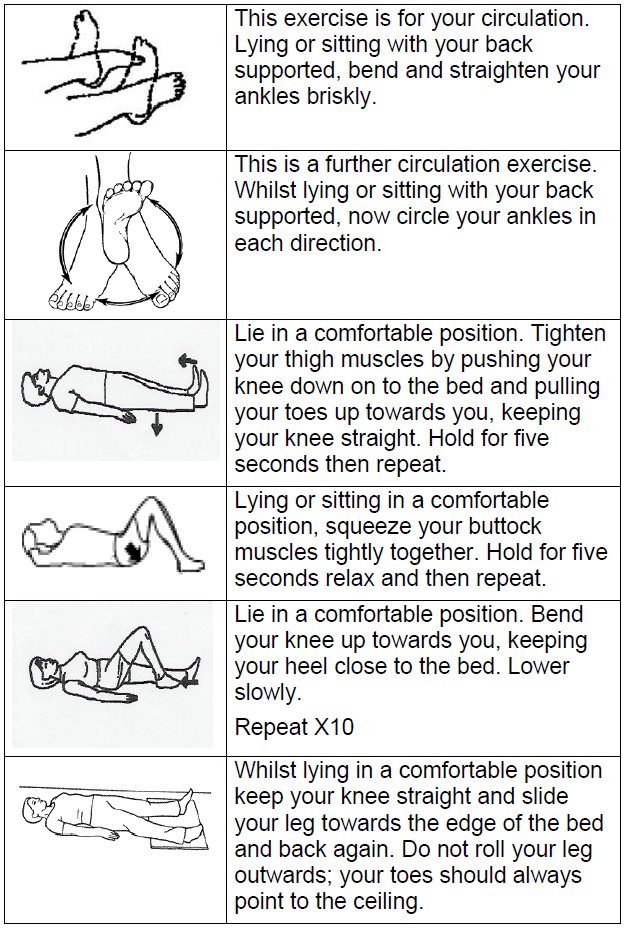
Physiotherapy treatment
- Passive Physical Treatments for Herniated Discs
- Deep Tissue Massage: a deep tissue massage is an ideal option if you have a herniated disc because it uses a great deal of pressure to relieve deep muscle tension & spasms, which develop to prevent muscle motion in the affected area.
- Hot & Cold Therapy: Both hot & cold therapies offer their own set of benefits, & the physical therapist might alternate between them to get the best results. Your physical therapist might use heat to increase blood flow to the target area. Blood helps heal the area by distributing extra oxygen & nutrients. Blood also removes waste products from muscle spasms.
- Conversely, cold therapy (also called cryotherapy) slows circulation. This reduces inflammation, muscle spasms & pain. the physical therapist might place an ice pack on the target area, give you an ice massage, & even use a spray known as fluoromethane to cool inflamed tissues.
- Hydrotherapy– As the name suggests, hydrotherapy involves water. As a passive treatment, hydrotherapy might involve simply sitting in a whirlpool bath or warm shower. Hydrotherapy delicately relieves pain & relaxes muscles.
Transcutaneous electrical nerve stimulation (TENS)
- A TENS machine uses an electrical current to stimulate the muscles. It sounds sharp, but it really isn’t painful. Electrodes taped to the skin send a small electrical current to key points on the nerve pathway. TENS decreases muscle spasms & is generally believed to trigger the release of endorphins, which are the body’s natural painkillers.
Traction:
- The goal of traction is to decrease the effects of gravity on the spine. By gently pulling aside the bones, the purpose is to decrease disc herniation. The analogy is much like a flat fatigue” disappearing” when you put a jack under the car and take pressure off the fatigue. It can be done in the cervical or lumbar spine.
Active Treatments You might Try in Physical Therapy
Active treatments assist address flexibility, posture, strength, core stability, & joint movement. An exercise program might also be prescribed to achieve maximal results. This will not only check recurrent pain but will also benefit overall health. the physical therapist will work with you to develop a program based on the specific diagnosis & check the health history.
Core stability: Many people don’t perceive how important a strong core is to their spinal health. the core (abdominal) muscles assist the back muscles to support the spine. When the core muscles are weak, it puts extra pressure on the back muscles. the physical therapist might teach you to do core stabilizing exercises to strengthen the back.
Flexibility: Learning proper stretching & flexibility techniques will prepare you for aerobic & strengthening exercises. Flexibility helps the body move easier by warding off stiffness.
Hydrotherapy: In contrast to simply sitting in a hot tub or bath like its passive counterpart, active hydrotherapy might involve water aerobics to help condition the body without unnecessary stress.
Muscle strengthening:
- Strong muscles are a great support system for the spine & better handle pain. the physical therapist will teach you ways to condition & strengthen the back to help prevent future pain. You may learn self-care principles so you understand how to best treat the symptoms. The eventual goal is for you to expand your knowledge to maintain a pain-free lifestyle.
- It’s essential that you learn how to exercise & condition the back after the formal physical therapy ends. If you don’t instrument the lessons you learned during physical therapy, you won’t enjoy its long-term results. By taking care of the back on your own, you may prevent further herniated disc pain.
FAQ
What are the 3 purposes of the intervertebral discs?
It gives cushioning for the vertebrae & decreases the stress caused by impact. They work as shock absorbers for the spine. intervertebral dis help protect the nerves that run down the spine & between the vertebrae
What is the 2 constituent of an intervertebral disc?
Movement at a single disc level is limited, but all of the vertebrae & discs combined to allow for a significant range of motion. The intervertebral disc is made up of two components: the annulus fibrosus & the nucleus pulposus.
What happens if the intervertebral disc is damaged?
Sometimes the exterior of these rubbery disks can tear, & the soft inside slips out. This results in a herniated disk, also known as a slipped disk & ruptured disk. This disk injury can provoke nearby nerves causing pain, numbness, or weakness in an arm or a leg.
What holds spinal discs in place?
Endplates. The top (superior) & bottom (inferior) of each vertebral body is covered with an endplate. Endplates are complex structures that blend into the intervertebral disc & help hold the disc in place.
What happens to the intervertebral disc as we get aged?
As people age, however, the discs undergo changes. They might dry out, thin, or crack. The soft cartilage core might bulge or herniate out through the fibrous outer area of the disc. Degenerative disc disease is an umbrella term that expresses these age-related processes.
How do intervertebral discs get nutrients?
Intervertebral disk cells need glucose for sustainability & oxygen to synthesize matrix components. Nutrients enter the disk via 2 vascular supply routes: capillary beds of end plates & the peripheral annulus fibrosus
Do intervertebral discs lubricate?
The nucleus pulposus is the gel-like center of the disc designed to absorb shock & give lubrication. It’s mostly made of water. As we get aged, it can dry up a bit, making the discs thinner & less shock absorbent.
What is the major purpose of the intervertebral discs?
The intervertebral disc serves primarily to allow movement between adjacent vertebral bodies, to absorb shock, & to distribute loads through the vertebral column.


8 Comments