Tibial Nerve
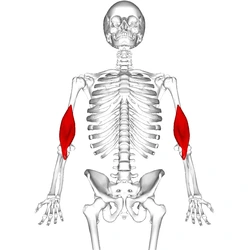
The tibial nerve is a major peripheral nerve of the lower limb. It has several cutaneous and motor functions in the leg and foot.
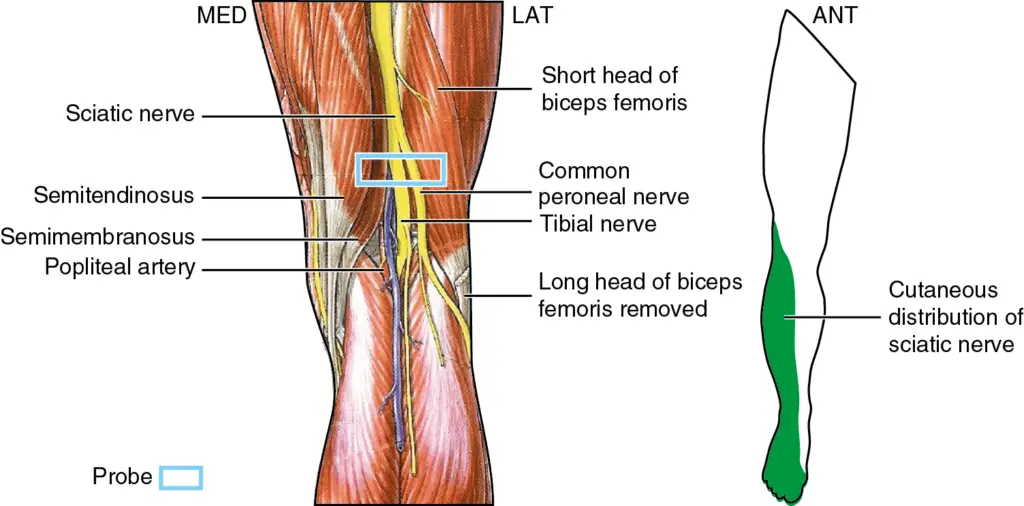
The tibial nerve is a branch of the sciatic nerve. The tibial nerve passes through the popliteal fossa to pass below the arch of the soleus.
Description of Tibial Nerve:
The Tibial Nerve is one of the two main muscular branches of the Sciatic Nerve.
The tibial nerve is the larger terminal branch with root values of L4, L5, S1, S2, and S3.
The Tibial Nerve provides innervation to the muscles of the lower leg and foot.
Specifically: Triceps Surae ( the two-headed Gastrocnemius and Soleus); Plantaris, Popliteus; Tibialis Posterior; Flexor Digitorum Longus; and Flexor Hallucis Longus muscles.
It also has articular and cutaneous branches.
Anatomical Course of Tibial Nerve:
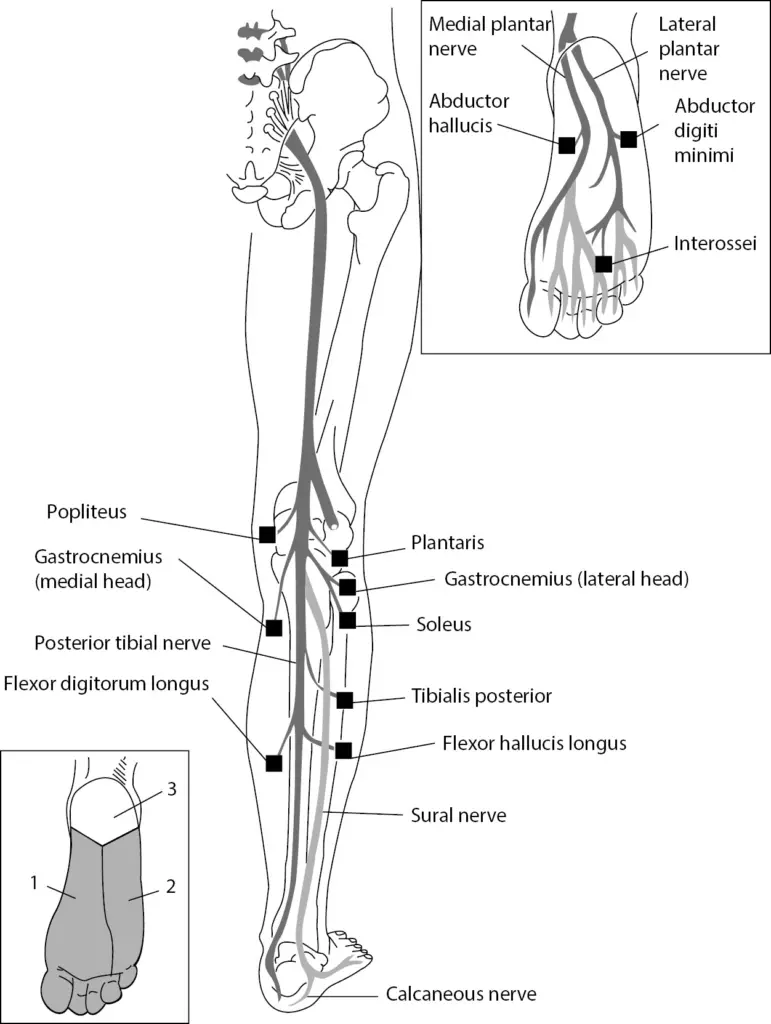
The tibial nerve is a branch of the sciatic nerve and arises at the apex of the popliteal fossa.
It travels through the popliteal fossa, giving off branches to muscles in the superficial posterior compartment of the leg.
The tibial nerve also gives rise to branches that contribute towards the sural nerve, which innervates the posterolateral aspect of the leg.
The tibial nerve continues its course down the leg, posterior to the tibia. During its descent, it supplies the deep muscles of the posterior leg.
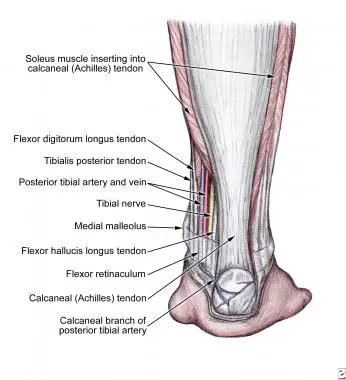
At the foot, the nerve passes posteriorly and inferiorly to the medial malleolus, through a structure known as the tarsal tunnel.
This tunnel is covered superiorly by the flexor retinaculum. Within this tunnel, branches arise from the tibial nerve to supply cutaneous innervation to the heel.
Immediately distal to the tarsal tunnel, the tibial nerve terminates by dividing into sensory branches, which innervate the sole of the foot.
Nerve roots:
L4-S3
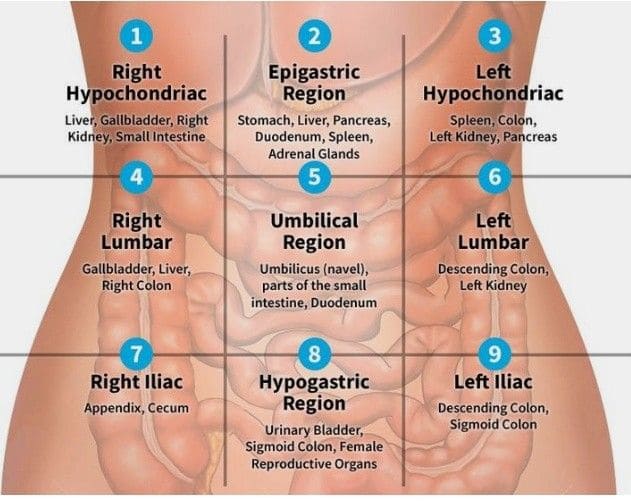
Sensory: Innervates the skin of the posterolateral side of the leg, the lateral side of the foot, and the sole of the foot.
Motor: Innervates the posterior compartment of the leg and the majority of the intrinsic foot muscles.
Structure of Tibial Nerve:
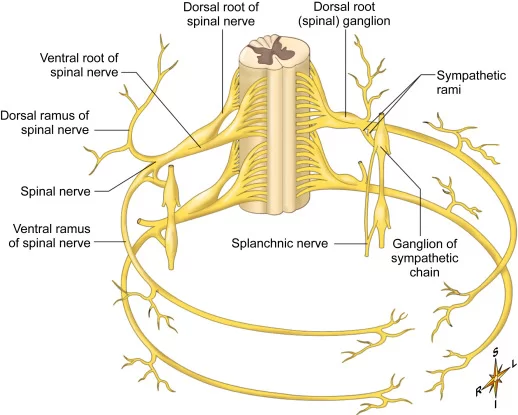
Popliteal fossa :
- Tibia nerve is the larger terminal branch of the sciatic nerve with root values of L4, L5, S1, S2, and S3.
- It lies superficial (or posterior) to the popliteal vessels, extending from the superior angle to the inferior angle of the popliteal fossa, crossing the popliteal vessels from lateral to medial side.
It gives off branches:
Muscular branches:
- Muscular branches arise from the distal part of the popliteal fossa.
- It supplies the medial and lateral heads of the gastrocnemius, soleus, plantaris, and popliteus muscles.
- The nerve to the popliteus crosses the popliteus muscle, runs downwards, and laterally, winds around the lower border of the popliteus to supply the deep (or anterior) surface of the popliteus.
- This nerve also supplies the tibialis posterior muscle, superior tibiofibular joint, tibia bone, interosseous membrane of the leg, and the inferior tibiofibular joint.
Cutaneous branches:
- The tibial nerve also gives off a cutaneous nerve called the medial sural nerve from the middle of the popliteal fossa and exits at the inferior angle.
- It supplies the skin of the lower half of the back of the leg and the lateral border of the foot until the tip of the little toe.
Articular branches:
- There are three articular branches that arise from the upper part of the fossa: Superior medial genicular nerve (located on the surface of the medial condyle of the femur.
- Middle genicular nerve (pierces the posterior capsule of the knee joint to supply the structures located in the intercondylar notch of the femur.
- Inferior genicular nerve (runs along the upper border of the popliteus to reach the medial condyle of the tibia).
Back of the leg:
- At the inferior angle of the popliteal fossa, the tibial nerve passes deep to the tendinous arch of the soleus to enter the back of the leg.
- In the leg, it runs downwards and medially to reach the posteromedial side of the ankle, midway between the medial malleolus and medial tubercle of the calcaneum.
- It terminates deep into the flexor retinaculum at the origin of the abductor hallucis by dividing into medial and lateral plantar nerves to supply the foot.
The tibial nerve gives off several branches to supply the back of the leg
Muscular branches:
- Supplies tibialis posterior, flexor digitorum longus, flexor hallucis longus, and deep part of soleus.
Cutaneous branches:
- The medial calcaneal nerve pierces the flexor retinaculum to supply the skin of the back and the lower surface of the heel.
Articular branches:
- Supplies the ankle joint
Foot:
In the foot, the nerve terminates by dividing into medial and lateral plantar branches.
Medial plantar nerve:
- It is the larger terminal branch of the tibial nerve. It passes between the abductor hallucis and flexor digitorum brevis to divide further into branches.
- Its distribution resembles that of the distribution of the median nerve in the hand.
- Its muscular branches supply the abductor hallucis, the flexor digitorum brevis, the flexor hallucis brevis, and the first lumbrical.
- Cutaneous distribution of the medial plantar nerve supplies the medial sole and medial three-and-one-half toes through four digital branches.
- Each digital branch gives off a dorsal branch to supply the nail beds on the dorsum.
- This nerve also gives off articular branches to supply the bones of the tarsus and metatarsus.
Lateral plantar nerve:
- It is the smaller terminal branch of the tibial nerve. It courses laterally and forward until the base of the fifth metatarsal bone, where it divides into superficial and deep branches.
- Its distribution resembles the distribution of the ulnar nerve in the hand. The main trunk of the nerve supplies two muscles: flexor digitorum accessorius and abductor digiti minimi.
- This nerve also supplies the skin of the sole.
- The superficial branch is divided into medial and lateral branches.
- The lateral branch supplies three muscles: flexor digiti minimi, 3rd and 4th interossei, and the skin over the lateral side of the toe.
- The medial branch communicates with the medial plantar nerve and supplies the skin over the fourth interdigital cleft.
- The deep branch supplies the 2nd, 3rd, and 4th lumbricals, first and second plantar interossei, and adductor hallucis.
Motor Functions :
The tibial nerve innervates all the muscles in the posterior compartment of the leg.
They are divided into deep and superficial compartment:
Deep:
- Popliteus – Laterally rotates the femur on the tibia to unlock the knee.
- Flexor hallucis longus – Flexes the big toe and plantar flexes the ankle.
- Flexor digitorum Longus – Flexes the other digits and plantar flexes the ankle.
- Tibialis posterior – Inverts the foot and plantar flexes the ankle.
Superficial:
- Plantaris – Plantar flexes the ankle.
- Soleus – Plantar flexes the ankle.
- Gastrocnemius – Plantar flexes the ankle and flexes the knee.
Sensory Functions:
- In the popliteal fossa, the tibial nerve gives off cutaneous branches. These combine with branches from the common fibular nerve to form the sural nerve.
- This sensory nerve innervates the skin of the posterolateral side of the leg and the lateral side of the foot.
The tibial nerve also supplies all the sole of the foot via three branches:
- Medial calcaneal branches: These arise within the tarsal tunnel, and innervate the skin over the heel.
- Medial plantar nerve: Innervates the plantar surface of the medial three and a half digits, and the associated sole area.
- Lateral plantar nerve: Innervates the plantar surface of the lateral one and a half digits, and the associated sole area.
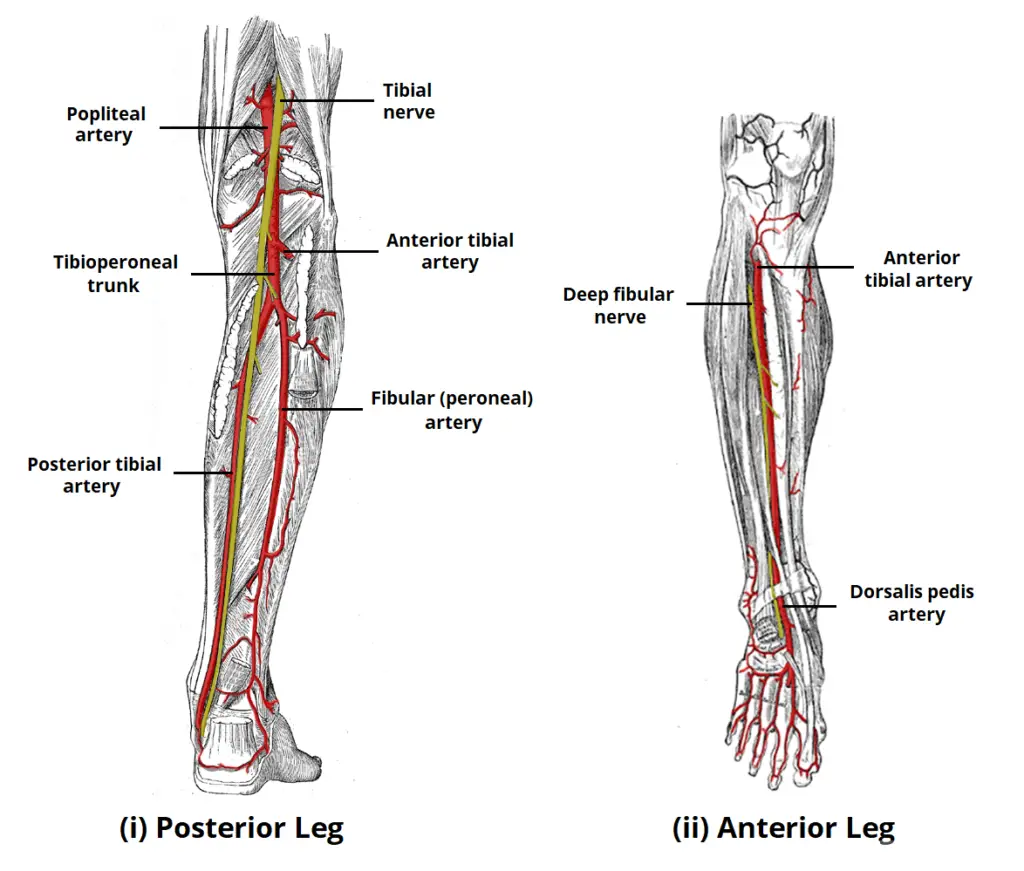
Blood Supply
The popliteal artery supplies the majority of the blood supply to the tibial nerve structures. The femoral artery, a sizable artery that passes beneath the inferior border of the inguinal ligament before entering the lower extremities through the femoral sheath, is continued by the popliteal artery.
Clinical Relevance:
Tarsal Tunnel Syndrome:
This is a condition where the tibial nerve is compressed within the tarsal tunnel (posterior to the medial malleolus). There are varying causes, of which the main three are:
- Osteoarthritis
- Rheumatoid arthritis
- Post-trauma ankle deformities
- Patients complain of paraesthesia in the ankle and sole of the foot, which can radiate up the leg slightly. It is aggravated by activity and relieved by rest.
- Tarsal tunnel symptoms can be treated conservatively by anti-inflammatory drugs and changes in footwear. If these interventions are not successful, the flexor retinaculum can be cut surgically, which releases the pressure.
Damage to the Tibial Nerve :
- Damage to the tibial nerve is rare and is often a result of direct trauma, entrapment through narrow space, or compression for a long period of time.
- Damage results in loss of plantar flexion, loss of flexion of toes, and weakened inversion (The tibialis anterior can still invert the foot).
The fascial membranes wrap a multitude of muscle groups seen in the human extremities. Four fascial envelopes or compartments—the anterior, lateral, superficial posterior, and deep posterior—are found in the leg. An abrupt or persistent rise in pressure inside a fascial compartment that compromises the blood flow to the compartment’s tissues is known as compartment syndrome.
While all four compartments may be affected, anterior compartment syndrome is the most prevalent. The most common cause of compartment syndromes is increasing limb swelling after trauma, which raises the pressure inside the compartment and eventually causes tissue ischemia and venous hypertension.
Tibial nerve ischemia resulting from untreated compartment syndrome of the deep posterior compartment can cause motor and sensory impairments in the foot and ankle. Plantar foot paresthesias as well as weakness in the toe and plantar flexion are among the deficiencies. For symptomatic individuals, the mainstay of treatment is fasciotomy, which involves cutting an incision in the surrounding fascia to lower the pressure inside the compartment. Decompression must occur right away in acute cases in order to prevent irreparable tissue necrosis.



18 Comments