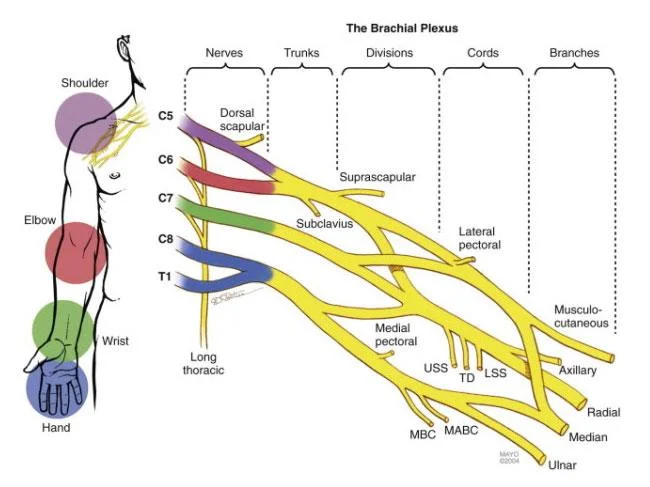
Brachial Plexus
What is the Brachial Plexus?
The brachial plexus is a network of nerves that originates from the spinal cord in the neck region and supplies the upper limb, including the shoulder, arm, forearm, and hand. It comes from nerve roots in the spinal cord’s cervical and upper trunk regions (C5-T1).
Anatomy of Brachial Plexus:
The skin and musculature of the upper limb are supplied by the brachial plexus, a network of nerve fibers. It starts at the neck’s base, travels through the axilla, and continues all the way down the upper extremities.
The first thoracic spinal neuron, T1, and the anterior rami (divisions) of cervical spinal nerves C5, C6, C7, and C8 together make up the plexus.
The roots, trunks, divisions, cables, and branches make up the brachial plexus. These divisions serve just to clarify the brachial plexus; there are no functional distinctions between them.
Structure and function:
The upper extremities, including the scapular area, receives somatic motor and sensory innervation from the brachial plexus. The brachial plexus has a number of designated sections depending on how the plexus was created as it passes through the posterior triangle of the neck into the axilla, arm, forearm, and hand. The superior, inferior, and intermediate trunks are created when the ventral rami from the brachial plexus’s roots, the spinal nerves C5 through T1, come together.
The C5 and C6 roots create the superior trunk, the C8 and T1 roots the inferior trunk, and the C7 root the middle trunk as they proceed from the posterior triangle into the axilla.
The divisions are bundles that extend from the trunks. To create the lateral, posterior, and medial cords, each brachial plexus trunk continues as an anterior and posterior division.
The anterior and posterior divisions combine to produce the three cords (posterior, medial, and lateral), which are so named because of how closely they resemble the anterior and posterior divisions of the axillary artery. The anterior division from the middle trunk and the anterior division from the superior trunk combine to produce the lateral cord, while the three posterior divisions converge to form the posterior cord. The medial cord is still produced by the anterior division of the inferior trunk. This “mixing” of nerve fibers causes the lateral cord to have C5, C6, and C7 components, the medial cord to include C8 and T1 contributions, and the posterior cord to include fibers from all levels of the brachial plexus (C5 to T1).
The C5–T1 spinal levels contribute in various ways to the brachial plexus’s ultimate subdivision, which consists of five terminal branches.
The section Nerves and Muscles below goes into further detail on the brachial plexus’s terminal and non-terminal branches.
Embryology:
From cells in the spinal cord’s basal plate during development, motor nerve fibers similar to those seen in the brachial plexus emerge to the ventral nerve root. Neural crest cells give rise to the sensory nerve fibers in the dorsal nerve root. The dorsal and ventral nerve roots will ultimately converge to create a spinal nerve as they move in the same direction. The dorsal and ventral principal rami of the spinal nerves will separate. Nerves will lengthen and extend into the limb in dermatomal and myotomal distributions as the limb bud matures.
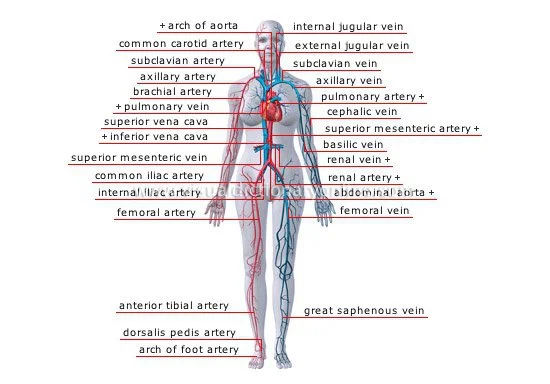
Blood Supply and Lymphatics:
The majority of the blood supply to the brachial plexus is provided by the subclavian artery and its branches. The ascending and deep cervical arteries’ muscular branches, as well as occasionally the subclavian’s muscular branches, supply the trunks. The subclavian, axillary, and subscapular arteries deliver blood to the cords.
Roots of Brachial Plexus:
The “roots” are the anterior rami of the spinal nerves that make up the brachial plexus. These are the anterior rami of the spinal nerves C5, C6, C7, C8, and T1.
A pair of spinal nerves emerge from each level of the vertebra. The intervertebral foramina of the vertebral column are where they exit the spinal cord.
Then, each spinal nerve splits into a front and a back ramus. The anterior rami of spinal nerves C5–T1—whose posterior divisions innervate the skin and musculature of the intrinsic back muscles—form the roots of the brachial plexus.
These nerves enter the base of the neck after forming between the anterior and medial scalene muscles.
Trunks of Brachial Plexus
The brachial plexus has three trunks that merge at the base of the neck. The names of these structures reflect their approximate anatomical locations:
There are three trunks of brachial plexus:
- Superior trunk
- Middle trunk
- Inferior trunk
Superior trunk: a root system with C5 and C6 combined.
Middle trunk: C7 is continued.
Inferior trunk: a mixture of T1 and C8 roots.
The trunks pass the posterior triangle of the neck as they move laterally.
Divisions of Brachial Plexus:
In the neck’s posterior triangle, each trunk splits into two branches. Both divisions migrate in opposite directions—one towards the front of the body and the other towards the back. They are referred to as the anterior and posterior divisions as a result.
We now have three nerve fibers in the anterior and posterior. The axilla is where these divisions enter after leaving the posterior triangle. They merge back together to form the brachial plexus cables.
Cords of Brachial Plexus:
The three cords are identified by their positions in relation to the axillary artery once the anterior and posterior divisions have reached the axilla.
There are three cords of the brachial plexus
- Lateral cord
- Posterior cord
- Medial cord
Lateral cord:
The lateral cord is formed by:
- the superior trunk’s anterior division
- a portion of the middle trunk’s anterior division
Posterior cord:
The posterior cord is formed by:
- the superior trunk’s posterior division
- The middle trunk’s rear section
- the inferior trunk’s posterior division
Medial cord:
The medial cord is formed by:
- the inferior trunk’s anterior division.
- The cords give birth to the brachial plexus’ main branches.
Branches of Brachial Plexus:
The three cords give birth to five primary branches that are located in the axilla and the proximal part of the upper limb. These nerves continue up the upper limb, innervating the skin and muscles there.
Supraclavicular branches:
Dorsal scapular nerve:
Most frequently, the dorsal scapular nerve develops straight from the root of the C5 spinal nerve. On rare occasions, it may come from the brachial plexus’s superior trunk. The levator scapulae, rhomboid major, and rhomboid minor muscles all receive motor innervation from the dorsal scapular nerve.
Suprascapular nerve:
The superior trunk gives way to the suprascapular nerve, which transmits C5 and C6 nerve fibers. The glenohumeral and acromioclavicular joints get sensory innervation from the suprascapular nerve, while the supraspinatus and infraspinatus muscles receive motor innervation.
Long thoracic nerve:
The roots of C5, C6, and C7 combine to form the long thoracic nerve. The serratus anterior muscle receives motor innervation from this nerve.
Subclavian nerve:
The C5 and C6 spinal nerve fibers are found in this nerve, which arises from the superior trunk of the brachial plexus. The motor innervation for the subclavius muscle comes from the subclavian nerve.
Branches of the lateral cord:
The lateral pectoral nerve and the lateral root of the median nerve are two preterminal branches that arise from the lateral cord. The musculocutaneous nerve, one of the brachial plexus’ terminal branches, is also produced by it.
Lateral pectoral nerves:
The lateral cord of the brachial plexus gives birth to the lateral pectoral nerves, which transport C5, C6, and C7 spinal nerve fibers. The lateral nerves contribute to the innervation of the pectoralis minor muscle by anastomoses with the medial pectoral nerves.
The lateral root of the median nerve:
One of the two roots of the median nerve is this small branch. The medial root is a branch of the medial cord, and it combines fast to produce the median nerve.
Musculocutaneous nerve:
Roots: C5, C6, C7.
Motor Functions: nourishes the biceps brachii, coracobrachialis, and brachialis muscles.
Sensory Functions: emits the lateral cutaneous branch of the forearm, which innervates a tiny lateral area of the posterior forearm as well as the lateral part of the anterior forearm.
Branches of medial cord:
The medial cord also creates the medial pectoral nerve, medial brachial cutaneous nerve, medial antebrachial cutaneous nerve, and the medial root of the median nerve in addition to the ulnar nerve.
Medial pectoral nerves:
The medial cord of the brachial plexus, which contains C8 and T1 spinal nerve fibers, is where the medial pectoral nerves emerge. The lower sternocostal region of the pectoralis major muscle and the pectoralis minor muscle both receive motor innervation from this nerve.
Medial brachial cutaneous nerve:
The medial cord, which carries C8 and T1 spinal nerve fibers, gives rise to the medial brachial cutaneous nerve, also known as the medial cutaneous nerve of the arm. The inferior section of the medial side of the arm’s skin is sensory innervated by this nerve.
Medial antebrachial cutaneous nerve:
The medial cord transporting T1 spinal nerve fibers gives rise to the medial antebrachial cutaneous nerve, commonly known as the medial cutaneous nerve of the forearm. This nerve innervates the skin of the medial side of the forearm and the skin of the arm covering the biceps brachii with sensory information.
The medial root of the median nerve:
The second source of the median nerve is the medial root of the nerve. The median nerve’s trunk is formed when it combines with the lateral root previously stated.
Ulnar nerve:
Roots: C8 and T1.
Motor Functions: innervates the flexor carpi ulnaris and medial half of the flexor digitorum profundus, as well as the hand’s other muscles (apart from the thenar and two lateral lumbricals).
Sensory Functions: innervates the associated region of the palm as well as the medial first and second finger’s anterior and posterior surfaces.
Motor supply:
the remaining forearm muscles (medial half of the flexor digitorum profundus, flexor carpi ulnaris muscle) that are not supplied by the median nerve.
Except for the lateral two lumbricals, opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis muscles, all intrinsic hand muscles.
Sensory supply:
The medial one-half of the palm’s anterior and posterior surfaces are covered with skin.
The medial one-and-a-half fingers’ anterior and posterior surfaces are covered with skin.
The ulnar nerve supplies the hand muscles:
Hypothenar muscles
Interossei muscles (dorsal and palmar interossei)
Medial two Lumbricals
Adductor pollicis
Branches of posterior cord:
The subscapular, thoracodorsal, and axillary nerves, as well as the radial nerve, are all derived from the posterior cord of the brachial plexus.
Subscapular nerves:
These nerves, the superior and inferior subscapular nerves, are often present in pairs. The fibers of the C5 spinal nerve are carried by both of these nerves when they emerge from the posterior cord. The inferior subscapular nerve innervates the remainder of the subscapularis muscle as well as the teres major muscle, while the superior subscapular nerve only affects the superior part of the subscapularis muscle.
Thoracodorsal nerve:
The C7 and C8 fibers are carried by the thoracodorsal nerve, which emerges from the brachial plexus’ posterior chord. The latissimus dorsi muscle receives motor innervation from this nerve.
Axillary nerve:
Roots: C5 and C6.
Motor Functions: innervates the deltoid and teres minor muscles.
Sensory Functions: emits the arm’s superior lateral cutaneous nerve, which innervates the deltoid’s inferior area.
Radial nerve:
Roots: C5 – T1.
Motor Functions: predominantly, but not only, extensors of the wrist and fingers, the triceps brachii, and the muscles in the posterior compartment of the forearm are also innervated.
Sensory Functions: innervates the posterolateral side of the hand as well as the posterior arm and forearm.
Motor supply:
The triceps brachii muscle, together with the rest of the arm’s posterior compartment muscles.
The muscles of the posterior compartment of the forearm include the brachioradialis, anconeus, supinator, extensor carpi radialis longus and brevis, extensor carpi ulnaris, extensor digitorum, extensor pollicis longus and brevis, extensor indicis, extensor digiti minimi, and abductor pollicis longus.
Sensory supply:
The skin covers the back of the arm.
The skin on the forearm’s middle, posterior surface.
The skin on the hand’s dorsum’s lateral surface.
The skin on the lateral two-and-a-half fingers’ backside.
Median nerve:
Two roots from the lateral and medial cords of the brachial plexus combine to generate the median nerve:
the terminal branch of the lateral cord known as the lateral root of the median nerve.
the terminal branch of the medial cord’s median nerve’s medial root.
The median nerve divides into its terminal branches in the hand after traveling the length of the entire upper limb. Multiple areas of the forearm and hand get both motor and sensory innervation from this mixed nerve.
The following receive motor supply from the median nerve:
Except for the flexor carpi ulnaris and the medial half of the flexor digitorum profundus, all of the flexor muscles are in the forearm’s flexor compartment.
save for the adductor pollicis and all the thenar muscles.
lateral lumbrical muscles on both sides.
The following get sensory input from the median nerve:
The skin on the palm’s lateral half.
the skin on the lateral three-and-a-half fingers’ anterior side.
The skin on the lateral two-and-a-half fingers’ backside.
The following mnemonic can be used to quickly recall the median nerve’s role in the motor supply of the hand.
The hand muscles are supplied by the median nerve:
- Lateral two lumbricals
- Opponens pollicis
- Abductor pollicis brevis
- Flexor pollicis brevis
Physiologic Variants:
Contributions from C4 and T2 are one of the most prevalent variations of the brachial plexus. These levels of the spinal cord can contribute in different ways. A branch from C4 could be little whereas a branch from T2 might be huge, for instance. The levels present in a particular nerve might differ, even with the normal amounts involved in the creation of the brachial plexus. This may result in changes to the dermatomal distribution or the muscles’ primary innervation.
Clinical Significance
Brachial Plexus Injury
A brachial plexus injury refers to damage or trauma to the brachial plexus, which is a complex network of nerves that controls movement and sensation in the shoulder, arm, forearm, and hand. These injuries typically occur due to high-impact accidents or during childbirth, but they can also result from sports injuries, falls, or other trauma to the upper body.
Brachial plexus injuries can vary in severity, ranging from mild stretching of the nerves (neuropraxia) to partial tearing (axonotmesis) or complete severing (neurotmesis) of the nerves. The extent of the injury determines the symptoms and the potential for recovery.
These injuries can be categorized into different types based on their location and severity:
- Avulsion injuries often result from significant trauma, such as motor vehicle accidents or falls, and may lead to complete loss of function in the affected limb.
- Rupture: A rupture occurs when the nerve is torn, but the nerve roots remain attached to the spinal cord. This type of injury can also cause severe functional impairment and may require surgical intervention for repair.
- Neuroma: In some cases, when the nerve is stretched or injured, scar tissue may form, resulting in the formation of a neuroma. A neuroma can interfere with nerve signal transmission and lead to pain or abnormal sensations.
- Neuropraxia: Neuropraxia refers to a temporary and mild form of brachial plexus injury where the nerves are stretched but not torn. It typically causes temporary weakness, numbness, or tingling sensations in the affected limb but often resolves on its own with time and conservative treatment.
The symptoms of a brachial plexus injury can vary depending on the location and severity of the damage. Common symptoms include:
- Weakness or paralysis in the affected arm, shoulder, or hand
- Numbness or loss of sensation in the affected limb
- Tingling or burning sensations
- Lack of muscle control or coordination
- Muscle atrophy (wasting) over time
The treatment of brachial plexus injuries depends on several factors, including the type and severity of the injury, the age and overall health of the individual, and the time since the injury occurred. Treatment options may include physical therapy to improve muscle strength and range of motion, pain management techniques, assistive devices, and in some cases, surgical intervention to repair or reconstruct the damaged nerves.
Early diagnosis and appropriate treatment can greatly improve the chances of functional recovery in individuals with brachial plexus injuries. Therefore, prompt medical attention is crucial if a brachial plexus injury is suspected.
Summary:
The brachial plexus is a network of nerves that links to the nerves in the arm. It comes from nerve roots in the spinal cord’s cervical and upper trunk regions (C5-T1).
FAQ:
What is the brachial plexus’s biggest branch?
The C5 and C6 spinal nerve fibers are found in the subclavian nerve, which arises from the superior trunk of the brachial plexus.
Are there two brachial veins?
The brachial veins are usually two in number and they are located on either side of the brachial artery. Near the level of the elbow, the radial and ulnar venae comitantes often join to form them.
What is the nerve plexus anatomy?
Introduction. The nerve plexuses are proximal portions of peripheral nerves that emerge from the spinal foramina with nerves from various levels of the spine interacting and tangling to generate distinct nerves farther distally. The brachial and lumbosacral plexuses are the two main nerve plexuses.
What is the brachial plexus’s blood supply?
Results: The brachial plexus is supplied by branches of the subclavian-axillary axis, and these branches anastomose each other. According to the distribution feature, the blood supply of the brachial plexus could be divided into three zones.



8 Comments