Gout and Physiotherapy Treatment
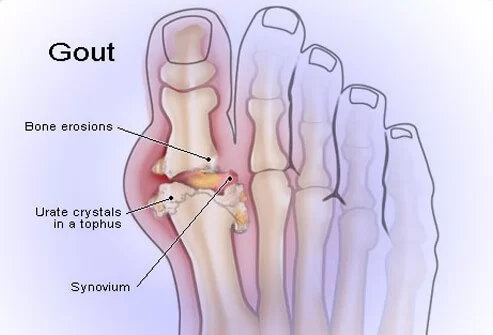
Gout is a form of arthritis characterized by severe pain, redness, swelling, and tenderness in the joints, most commonly affecting the base of the big toe. It occurs due to the accumulation of uric acid crystals in the tissues around the joints. Gout is considered a chronic condition and is part of a group of diseases called crystal arthropathies.
Uric acid is a natural waste product that is produced when the body breaks down purines, substances found in certain foods and beverages Usual uric acid excretion from the body occurs through the kidneys after dissolving in the blood. However, in some cases, either the body produces too much uric acid or the kidneys are unable to eliminate it effectively, leading to its accumulation in the form of crystals.
When uric acid crystals accumulate in a joint, they can trigger an immune response, resulting in inflammation and intense pain. Gout attacks often occur suddenly and typically affect one joint at a time, with the big toe being the most commonly affected site. However, gout can also affect other joints, such as the ankles, knees, elbows, wrists, and fingers.
- Gout is a type of arthritis that causes inflammation, usually in one joint, that begins suddenly. Gouty arthritis is caused by the deposition of needle-like crystals of uric acid in a joint.
Pathophysiology of Gout

- Gout is caused by too much uric acid in the bloodstream and the accumulation of urate crystals in tissues of the body. Uric acid is normally found in the body as a byproduct of the way the body breaks down certain proteins called purines. Normally, uric acid dissolves in blood and passes through the kidneys into the urine.
- But sometimes either body produces too much uric acid or the kidneys excrete too little uric acid. When this happens, uric acid can build up, forming sharp, needle-like urate crystals in a joint or surrounding tissue that cause pain, inflammation, and swelling. It mainly affects the joints.it is commonly seen in the big toe(1st metatarsophalangeal joint) in men.
- there may be the formation of osteophytes and in late stages reduction in joint space. during the acute stage involved, the joint has signs and symptoms of acute inflammation with hard and tender nodules.
Risk factors for Gout
Factors that increase the uric acid level in your body include:
- Diet– Eating a diet rich in meat and seafood and drinking beverages sweetened with fruit sugar (fructose) increases levels of uric acid, which increases your risk of gout. Alcohol consumption, especially of beer, also increases the risk of gout.
- Obesity– If you’re overweight, your body produces more uric acid and your kidneys have a more difficult time eliminating uric acid.Medical conditions. Certain diseases and conditions increase your risk of gout. These include untreated high blood pressure and chronic conditions such as diabetes, metabolic syndrome, and heart and kidney diseases.
- Certain medications- The use of thiazide diuretics — commonly used to treat hypertension — and low-dose aspirin also can increase uric acid levels. So can the use of anti-rejection drugs prescribed for people who have undergone an organ transplant.
- Family history of gout-– If other members of your family have had gout, you’re more likely to develop the disease.
- Age and sex– Gout occurs more often in men, primarily because women tend to have lower uric acid levels. After menopause, however, women’s uric acid levels approach those of men. Men are also more likely to develop gout earlier — usually between the ages of 30 and 50 — whereas women generally develop signs and symptoms after menopause.
- Recent surgery or trauma– Experiencing recent surgery or trauma has been associated with an increased risk of developing a gout attack.
Symptoms of Gout
- Intense joint pain. Gout usually affects the large joint of the big toe, but it can occur in any joint. Other commonly affected joints include the ankles, knees, elbows, wrists, and fingers. The pain is likely to be most severe within the first four to 12 hours after it begins.
- Lingering discomfort. After the most severe pain subsides, some joint discomfort may last from a few days to a few weeks. Later attacks are likely to last longer and affect more joints.
- Inflammation and redness. The affected joint or joints become swollen, tender, warm, and red.
- Limited range of motion
Differential Diagnosis
When diagnosing gout, healthcare professionals consider a range of possible conditions that may present with similar symptoms. It’s important to differentiate gout from other conditions to ensure appropriate treatment. Here are some of the main conditions that can be considered in the differential diagnosis of gout:
- Pseudogout: Pseudogout, also known as calcium pyrophosphate deposition disease (CPPD), is a condition that resembles gout but is caused by the deposition of calcium pyrophosphate crystals in the joints. Symptoms, such as joint pain, swelling, and inflammation, can be similar to those of gout. Aspirating joint fluid and examining it under a microscope can help distinguish between gout (uric acid crystals) and pseudogout (calcium pyrophosphate crystals).
- Septic arthritis: Septic arthritis is a bacterial or fungal infection of a joint, which can cause joint inflammation, pain, and swelling. It can be challenging to differentiate septic arthritis from gout solely based on symptoms, so joint fluid analysis and blood tests are crucial in making an accurate diagnosis.
- Rheumatoid arthritis: Rheumatoid arthritis (RA) is an autoimmune disease that primarily affects the joints, leading to chronic inflammation, pain, and joint deformity. While gout typically affects one joint at a time, RA often involves multiple joints symmetrically. Blood tests, such as rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibody tests, can help differentiate RA from gout.
- Osteoarthritis: Osteoarthritis is a degenerative joint disease characterized by the breakdown of joint cartilage. It can cause joint pain, stiffness, and swelling, which may resemble gout symptoms. X-rays or other imaging tests can help identify joint damage and distinguish between osteoarthritis and gout.
- Cellulitis: Cellulitis is a bacterial skin infection that can lead to redness, swelling, warmth, and pain in the affected area. Cellulitis can sometimes occur in the same regions as gout flares, such as the lower leg or foot. The presence of fever, skin changes, and spreading redness can help differentiate cellulitis from gout.
- Tendonitis: Tendonitis is the inflammation of a tendon, which can cause pain, swelling, and difficulty moving the affected joint. Although it primarily affects tendons rather than the joint itself, tendonitis can be mistaken for gout due to similar symptoms. Physical examination and imaging studies can help distinguish between the two conditions.
- Psoriatic arthritis: Psoriatic arthritis is an inflammatory arthritis associated with the skin condition psoriasis. It can cause joint pain, stiffness, and swelling, similar to gout. The presence of psoriasis skin lesions and characteristic patterns of joint involvement can help differentiate psoriatic arthritis from gout.
Diagnosis of Gout

- Joint fluid test- Your doctor may use a needle to draw fluid from your affected joint. Urate crystals may be visible when the fluid is examined under a microscope.
- Blood test- Your doctor may recommend a blood test to measure the levels of uric acid and creatinine in your blood. Blood test results can be misleading, though. Some people have high uric acid levels but never experience gout. Some people have signs and symptoms of gout but don’t have unusual levels of uric acid in their blood.
- X-ray imaging- Joint X-rays can be helpful to rule out other causes of joint inflammation.
- Ultrasound-Musculoskeletal ultrasound can detect urate crystals in a joint or in a tophus. This technique is more widely used in Europe than in the United States.
- Dual-energy CT scan-This type of imaging can detect the presence of urate crystals in a joint, even when it is not acutely inflamed. This test is not used routinely in clinical practice due to the expense and is not widely available.
Treatment of Gout
Treatment for gout usually involves a combination of lifestyle changes, medications, and managing underlying health conditions. Lifestyle modifications may include adopting a low-purine diet, losing weight if necessary, limiting alcohol consumption, and staying hydrated. Medications can help alleviate pain during gout attacks and reduce uric acid levels to prevent future flare-ups.
Medications to treat gout attacks
Drugs used to treat acute attacks and prevent future attacks include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs).-NSAIDs include over-the-counter options such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve), as well as more-powerful prescription NSAIDs such as indomethacin (Indocin) or celecoxib (Celebrex).
- Colchicine- colchicine (Colcrys, Mitigare), is a type of pain reliever that effectively reduces gout pain.
- Corticosteroids.-Corticosteroid medications, such as the drug prednisone, may control gout inflammation and pain. Corticosteroids may be in pill form, or they can be injected into the joint.
- Corticosteroids are generally used only in people with gout who can’t take either NSAIDs or colchicine.
Physiotherapy Treatment of Gout
Physiotherapy treatment depends on the affected joint
main goals of the physiotherapy will be
1. to relieve pain
2. to relieve inflammation
3. to maintain Rom and strength

- Cryotherapy to alleviate the pain associated with acute bouts of gout may be effective. in the form of a crushed ice pack will provide pain relief as well as relieve inflammation.
- Range of motion exercise will be beneficial for maintaining the normal functions of joints.
- Strengthening exercises: Strengthening exercises for the surrounding muscles can help support and stabilize the affected joint(s). Strengthening exercises may include resistance training using weights, resistance bands, or bodyweight exercises.
- Manual therapy: Manual therapy techniques, such as joint mobilization and soft tissue mobilization, can be used to improve joint mobility, reduce stiffness, and alleviate pain.
- Assistive devices: In some cases, assistive devices such as braces, splints, or crutches may be recommended to provide support, reduce stress on the affected joint, and promote proper alignment and gait.
- Exercise and weight management: Physiotherapists may prescribe specific exercises and help individuals develop an exercise program tailored to their abilities and needs. Regular exercise can aid in weight management, improve overall cardiovascular health, and promote joint flexibility and strength. Physiotherapists will also help to lose weight.
Low Purine Diet: Best Foods to Eat & What to Avoid in Gout
A low-purine diet is often recommended for individuals with gout to help manage their condition and reduce the risk of gout flares. Purines are natural compounds found in certain foods that break down into uric acid during digestion. By limiting the intake of high-purine foods, uric acid levels can be lowered in the body. Here are some general dietary guidelines for a low-purine diet:
- Limit high-purine foods: Avoid or minimize consumption of foods high in purines. Examples of high-purine foods include organ meats (liver, kidney, sweetbreads), red meat (beef, lamb), certain seafood (anchovies, sardines, mussels, scallops), and some types of poultry (turkey, goose). Limiting or avoiding these foods can help reduce uric acid production.
- Choose low-purine protein sources: Opt for low-purine protein sources such as lean meats (chicken, turkey), low-fat dairy products (milk, yogurt, cheese), eggs, and plant-based proteins like legumes (beans, lentils), tofu, and tempeh.
- Increase complex carbohydrates: Incorporate more complex carbohydrates in your diet, including whole grains (such as brown rice, quinoa, whole wheat bread), fruits, and vegetables. These foods are generally low in purines and provide essential nutrients and fiber.
- Moderate your intake of certain vegetables: While most vegetables are considered low in purines, some contain moderate amounts. Examples include asparagus, spinach, cauliflower, mushrooms, and peas. While these vegetables can still be included in a low-purine diet, it is advised to consume them in moderation.
- Stay hydrated: Drinking an adequate amount of water helps to dilute uric acid and promote its excretion through the kidneys. Aim to drink plenty of water throughout the day.
- Limit alcohol consumption: Alcohol, especially beer, can increase uric acid levels and trigger gout flares. It is best to limit or avoid alcohol altogether. If you do choose to drink, do so in moderation and opt for low-purine alcoholic beverages like wine or spirits.
- Minimize sugary drinks: Sugary beverages, such as sodas and fruit juices, have been associated with an increased risk of gout. Opt for water or unsweetened beverages instead.
How to Prevent Gout?
Preventing gout involves adopting certain lifestyle modifications and managing underlying risk factors. Here are some key strategies to help prevent gout:
- Maintain a healthy weight: Excess weight increases the risk of developing gout. Losing weight, if necessary, can help reduce uric acid levels and decrease the likelihood of gout attacks. However, avoid crash diets or rapid weight loss, as they may temporarily increase uric acid levels and trigger gout flares.
- Follow a balanced diet: Limit foods that are high in purines, as they can increase uric acid levels in the body. Foods to moderate or avoid include red meat, organ meats (liver, kidney), seafood (particularly shellfish), sugary drinks, and alcoholic beverages (especially beer). Instead, focus on a diet rich in low-fat dairy products, vegetables, whole grains, and fruits. Cherries and cherry juice have also been associated with a lower risk of gout attacks.
- Stay hydrated: Drinking an adequate amount of water helps promote the excretion of uric acid through the kidneys. Aim for at least 8-10 glasses of water per day to maintain proper hydration.
- Limit alcohol consumption: Alcohol, especially beer, has been linked to an increased risk of gout. Limit your alcohol intake or avoid it altogether, particularly during gout flares.
- Exercise regularly: Engaging in regular physical activity helps maintain a healthy weight, improve overall cardiovascular health, and enhance joint function. Choose activities that are low-impact and joint-friendly, such as walking, swimming, cycling, or yoga.
- Manage underlying health conditions: Conditions like high blood pressure, diabetes, and metabolic syndrome can increase the risk of developing gout. It is important to manage these conditions through proper medical care, medication, and lifestyle modifications as advised by your healthcare provider.
- Avoid dehydration and limit sugary drinks: Dehydration can increase uric acid concentration in the body, so it’s important to stay well-hydrated. Additionally, excessive consumption of sugary drinks has been associated with a higher risk of gout.
- Take prescribed medications: If you have been prescribed medications to manage gout, such as urate-lowering drugs (e.g., allopurinol, febuxostat), take them as directed by your healthcare provider. These medications help lower uric acid levels and prevent gout flares.
- Monitor and manage stress: High levels of stress can potentially trigger gout attacks. Practice stress management techniques such as relaxation exercises, mindfulness, and engaging in activities you enjoy.







21 Comments