Knee injuries
Knee injuries are a prevalent and often debilitating health concern that can affect individuals of all ages and activity levels. The knee joint is a complex structure, comprising bones, ligaments, tendons, and cartilage, all working together to provide stability and facilitate various movements.
Unfortunately, the knee is susceptible to a wide range of injuries, stemming from traumatic incidents, overuse, or degenerative conditions.
These injuries can have a significant impact on an individual’s daily life, limiting mobility and causing pain. Athletes, in particular, are prone to knee injuries due to the repetitive stress placed on the joint during sports activities. Additionally, aging and certain medical conditions can contribute to the deterioration of the knee over time.
Self-care techniques are effective in treating many forms of mild knee discomfort. Other options for pain relief include physical therapy and knee braces. However, there are instances in which knee surgery is required.
Introduction
Injuries to the knee joint result from damage to one or more of the tissues that comprise it, including the muscles, tendons, cartilage, bones, and ligaments. These injuries can be caused by falling, violently twisting the knee, high impact from a car accident, or other forces. Common knee injuries involve fractures, dislocations, tears, and sprains.
Knees allow the legs to bend and straighten while providing the body with stable support. Since the knee is the largest joint in the body, injuries are common. Tendons, cartilage, ligaments, and bones are the four primary tissue types that make up the knee. An injury can cause damage to any of these significant tissue types.
Meniscus tears and anterior cruciate ligament (ACL) tears are two of the most frequent sports-related knee injuries. Although less frequent in sports, patella (kneecap) fractures can happen as a result of high-impact trauma. The majority of knee injuries need to be treated right away, and some might even need surgery.
Due to its complexity and multitude of parts, the knee is susceptible to a wide range of injuries. Sprains, ligament rips, fractures, and dislocations are a few of the most typical knee injuries.
Simple interventions like bracing and rehabilitation exercises effectively treat many knee injuries. Surgery might be necessary to repair other injuries.
Knees allow the legs to bend and straighten yet provide the body with secure support.
Since the knee is the largest joint in the body, injuries are common. The four basic tissue types in the knee are cartilage, tendons, ligaments, and bones. Any of these vital tissue kinds is susceptible to harm.
Common knee injuries involve:
- Sprain, which is an excessive tearing of the knee ligaments.
- Tear in a ligament, such as the ACL or PCL in the anterior cruciate ligament.
- Strains or excessive muscular and tendon stretching.
- Injury to the knee’s lining cartilage.
- Meniscus tear (the cartilage that separates the thighbone and shinbone).
- Discomfort at the area of the kneecap.
Less common injuries to the knee involve:
- Fractures (typically brought on by a direct hit, twisting, or falling onto the knee).
- Kneecap dislocations.
- Knee dislocations (rare because it takes a lot of force).
Anatomy
The largest and most easily injured joint in the body is the knee. It consists of four main structural components: ligaments, tendons, cartilage, and bones.
- Bones: Your knee joint is formed in the femur (thighbone), tibia (shinbone), and patella (kneecap). For minor protection, the patella rests in front of the joint.
- Articular cartilage: Articular cartilage lines the rear of the patella, the femur, and the tibia. The smooth material in question facilitates the seamless movement of your knee bones when you extend or contract your leg.Meniscus.Shock absorbers between your femur and tibia are two wedge-shaped pieces of meniscal cartilage. The meniscus, which helps stabilize and cushion the joint, is tougher and more rubbery than articular cartilage. Usually, when someone mentions a torn meniscus, they mean a torn piece of cartilage in the knee.
- Ligaments: Ligaments attach a bone to another bone. Your knee’s four major ligaments work as sturdy ropes to keep your knee stable and the bones together.
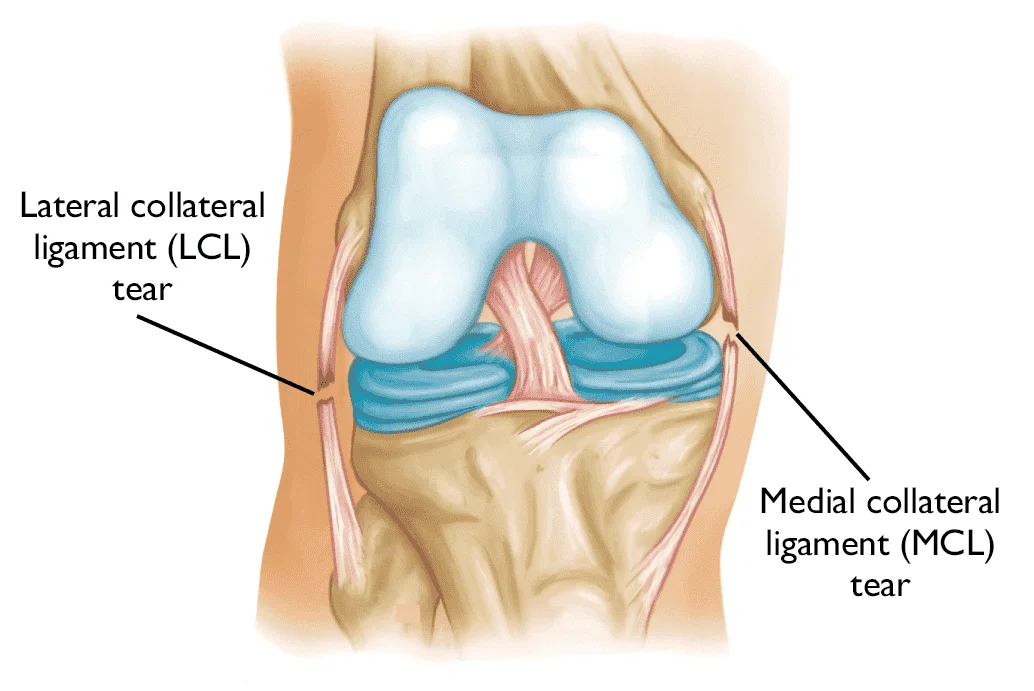
- Collateral ligaments: On either side of your knee are these. Your knee’s lateral collateral ligament is located on the outside, and the medial collateral ligament is located inside. They regulate your knee’s side-to-side movement.
- Cruciate ligaments: Within the knee joint is where they are located. The anterior cruciate ligament is in front and the posterior cruciate ligament is behind, forming an X with them crossing each other. Your knee’s front and back motions are governed by the cruciate ligaments.
- Tendons: Tendons help connect muscles to bones. The muscles in the front of the thigh are connected to the patella by the quadriceps tendon. The patellar tendon, on the other hand, connects the patella to the tibia.
Mechanism of injury
Numerous studies have tried to clarify the extrinsic and intrinsic factors that contribute to knee injuries because of the potentially serious acute and chronic morbidity of these injuries.
Intrinsic factors include ligamentous laxity, decreased muscle flexibility, muscle weakness, and foot shape; extrinsic factors include shoe wear, training surface conditions, and training regimen.
Athletes who play American football and soccer have been the focus of most studies on acute knee injuries. Shoe type is one extrinsic factor that has been researched in American football players. High school football players who wore “soccer style” shoes in the 1970s reported fewer knee and ankle injuries.
These players’ shoes had more cleats, which were shorter and wider than those worn traditionally. These results led to the measurement of torque forces, which was followed by the implementation of cleat size and length regulations by the National High School Athletic Federation and the National Collegiate Athletic Association.
In a study conducted by the National Football League between artificial turf and natural grass during the 1980–1989 season, it was discovered that artificial turf was responsible for 36 more knee injuries; nonetheless, only 11% of injuries required surgery due to anterior cruciate ligament (ACL) injuries.
Running shoes that are too small or too large for a runner’s foot type can cause overuse injuries, as can neglecting to replace an old shoe’s midsole when it starts to lose its ability to absorb impact. Training on hard surfaces, running on uneven terrain like hills or sand, or running on the same banked edge of a road or track can all lead to chronic injuries.
Within the first few weeks of beginning or drastically escalating the intensity of a training regimen, overuse injuries typically manifest. Athletes who move from high school to a collegiate level and whose training intensifies may also sustain injuries. It is important to advise athletes to gradually increase the volume and intensity of their training.
Numerous overuse injuries, including patellofemoral pain syndrome, have been linked to benign hypermobility syndrome and the generalized ligamentous laxity that it causes. On the other hand, numerous investigations have demonstrated that there is no connection between the frequency of knee ligament injuries or football players’ ligamentous laxity and benign hypermobility syndrome.
An instability that may require more knee recruitment and loading can be caused by weakness of the core (abdominal, paraspinal, and buttock) muscles. Acute knee effusions can also result in quadriceps weakness, which is commonly linked to overuse injuries to the knee.
Reduced knee load and the potential for overuse injury can result from weaker hamstrings, ITBs, calf muscles, and hip flexors. Athletes who have pes planus, pes cavus, or an abnormal foot shape may be more vulnerable to knee injuries.
Common Knee Injuries
Sprains and tears of soft tissues (such as ligaments, and meniscus), fractures, and dislocations are the most frequent injuries to the knee. Many times, injuries affect more than one knee structure.
The most typical symptoms of a knee injury are pain and swelling. The knee might also lock or catch. Instability, or the sensation that your knee is giving way, can be brought on by certain types of knee injuries, including ACL tears.
The knee joint is complex. People can sit, squat, jump, and run with it since it moves like a door hinge, bending and straightening their legs.
There are four parts to the knee:
- Bones.
- Cartilage.
- Ligaments.
- Tendons.
At the apex of the knee joint is the femur, also referred to as the thighbone. The base of the knee joint is composed of the tibia or shinbone.
The joint of the femur and tibia is covered by the patella, often known as the kneecap.
The tissue that cushions the knee joint’s bones is called cartilage. It also helps ligaments glide over the bones and shields them from impact.
For stability and to hold the bones together, the knee’s four ligaments function like ropes. Tendons attach to the bones in the upper and lower legs the muscles that support the knee joint.
Knee injuries come in a variety of forms. Here are ten of the most typical knee injuries.
Knee Ligament Injury
To support and regulate movement, tough bands of connective tissue called ligaments envelop a joint. Ligament injuries, also referred to as knee sprains, frequently occur as a result of a sports injury that makes the knee joint unstable. They also severely restrict how you can move your knee.
Four major ligaments, which join the thigh and shin bones, stabilize the knee:
- An anterior cruciate ligament (ACL) – the knee ligament located in the middle that regulates the shin bone’s rotation and forward motion. An ACL injury is a rip or sprain of the ACL brought on by abrupt stops, direction changes, jumping, and landings. In sports like football, basketball, and downhill skiing, it is typical.
- A posterior cruciate ligament (PCL) – the ligament in the middle of the knee that regulates the shin bone’s backward movement. The strongest ligament in your knee, the PCL, can sustain damage if it is strained or torn by a strong, sharp blow, most commonly during a football tackle or other similar activity.
- Lateral collateral ligament (LCL) – The ligament in charge of stabilizing the inner knee. Activities involving twisting, bending, or abrupt direction changes can cause injuries to the LCL. One instance would be being struck on the inside of the knee while playing football.
- Medial collateral ligament (MCL) – The outer knee ligament, which provides stability. A direct hit to the outside of the knee, such as during a game of hockey or football, can result in this injury, which is also known as an MCL sprain.
The knee displays instability in the direction that the injured ligament stabilizes when any one of these four is damaged. The Anterior Dawer Test (for ACL), the Posterior Dawer Test (for PCL), the Valgus Stress Test (MCL), and the Varus Stress Test (LCL) are the four specific tests used to assess injuries.
Symptoms Of Knee Ligament Injury
- At the moment of injury, there was a loud pop or snap.
- Abrupt, excruciating pain that occasionally keeps you from engaging in your sport.
- Discoloration around the knee, black and blue.
- Knee instability.
- swelling that occurs in the first 24 hours following an injury.
- A sensation of looseness in the joint.
- Inability to bear weight on the injured joint because of discomfort.
- bending the knee inward toward the exterior.
The doctor does a physical examination first to diagnose ligament damage. They’ll check the knee for soreness and swelling. Due to the various knee movements used to evaluate your range of motion and the external pressure applied to your knees, the procedure may cause discomfort.
Even though ligament injuries occur frequently, the severity of the injury can vary:
- Grade I: Ligament spraining occurs when the fibers in a Grade I injury have been slightly overstretched. There won’t be much, if any, swelling and very little bruises. A sprained MCL is an illustration of this kind of injury.
- Grade II: This occurs when there is partial tearing of the ligament fibers, but not complete tearing. There will be more bruising and swelling as well as greater pain and joint restriction compared to Grade I.
- Grade III: When the ligament is totally torn, it results in a Grade III injury, which initially causes excruciating pain. There will be severe swelling and bruises around the knee. An LCL tear is an illustration of this kind of injury.
A grading system is used to classify the extent of damage into three categories: Grade I (mild), Grade II (moderate), and Grade III (severe). The length of time a knee sprain lasts varies depending on the kind of sprain, the severity of the injury, your rehabilitation plan, and the kind of sport you play.
Small to moderate wounds frequently mend on their own. Surgery is typically not necessary for the majority of collateral ligament tears (MCL and LCL). Reconstructive injury, however, will be the sole choice in cases where the cruciate ligaments (PCL or ACL) have been torn and stretched to an extreme degree. If you receive the right care and participate in a quality physical therapy program, you should be able to recover completely.
Anterior Cruciate Ligament (ACL) Injuries
Anterior cruciate ligament injuries are a common consequence of participating in sports. Athletes who play cutting and pivoting sports like basketball, football, and soccer are more susceptible to ACL injuries.
Roughly changing direction quickly or landing from a jump improperly can cause an ACL tear. Damage to other knee structures, such as articular cartilage, the meniscus, or other ligaments, coexists with approximately half of all anterior cruciate ligament injuries.
The anterior cruciate ligament (ACL), which runs diagonally down the front of the knee, is essential for maintaining joint stability. ACL injuries can be rather serious and necessitate surgery.
ACL injuries are assigned a number between one and three. An ACL tear is referred to as a grade 3 sprain, whereas a grade 1 sprain is considered a minor injury.
Athletes who participate in contact sports like football or soccer frequently sustain ACL injuries. Sports involving contact, nevertheless, are not the main reason for this ailment.
An ACL tear may result from abruptly changing the direction of motion or from improperly landing from a jump.
Posterior Cruciate Ligament (PCL) Injuries
A blow to the front of the knee while the knee is bent frequently injures the posterior cruciate ligament. This frequently happens in car accidents and collisions involving sports. Most posterior cruciate ligament tears are partial tears that may mend on their own.
At the rear of the knee is where the posterior cruciate ligament is found. One of the several ligaments that joins the thighbone with the shinbone is this one. The shinbone can’t go rearward too much because of this ligament.
When the knee is bent, a posterior cruciate injury demands strong force. This degree of stress usually occurs in cases of severe falls onto a bent knee or injuries sustained in an event that affects the bent knee.
Collateral Ligament Injuries
A force that pushes the knee sideways is typically the cause of collateral ligament injuries. These are frequently injuries from contact.
A direct blow to the outside of the knee is typically the cause of MCL injuries, which are frequently related to sports.
The lateral collateral ligament can be injured by blows to the inside of the knee that cause the knee to bend outward (LCL). Less often than other knee injuries, lateral collateral ligament tears occur.
Collateral ligaments are what join the shinbone and thighbone. Athletes, especially those engaged in contact sports, frequently suffer injuries to these ligaments.
Tears to the collateral ligaments are a common consequence of direct collisions or impacts with other people or objects.
Patellofemoral Pain Syndrome
The condition known as patellofemoral pain syndrome, or “runner’s knee,” is characterized by pain near the patella, the kneecap, and is brought on by imbalances and misalignments in the surrounding muscles and structures. It is typical among athletes who engage in repetitive knee flexion activities like cycling, jumping, and running.
Symptoms Of Patellofemoral Pain Syndrome
- Sharp, dull pain in the anterior region of the knee.
- Discomfort that gets worse when you squat, climb stairs , or sit for extended periods.
- Sporadically buckling or giving way to the knee.
Treatment options include using orthotics or shoe inserts to support the feet and lessen stress on the knee joint, as well as physical therapy to strengthen the muscles surrounding the knee, improve flexibility, and correct imbalances.
Meniscal Tears
Sports-related meniscal tears are common. Meniscus tears can happen during twisting, cutting, pivoting, or being tackled.
Meniscal tears can also result from aging or arthritis. If the menisci have weakened with age, even a simple awkward twist while rising from a chair could result in a tear.
A meniscal tear is most likely what people mean when they talk about torn cartilage in the knee.
The two stretchy cartilage wedges that sit between the thighbone and shinbone are called menisci. During sports, these cartilage fragments may rupture unexpectedly. As they age, they might also tear more slowly.
The term “degenerative meniscus tear” describes a meniscus tear that results from aging naturally.
There can be a pop in the knee from an abrupt meniscus tear. The following few days following the first injury may see an increase in discomfort, edema, and tightness.
The meniscus is a shock-absorbing cartilage pad in the knee that has a crescent shape. Meniscal tears are a common type of knee injury that can be caused by a sudden twist or a significant trauma, particularly in sports environments.
The injury may happen on its own or in conjunction with ligament damage. Moreover, it can vary in severity from mild to severe based on the degree of damage.
Symptoms Of Meniscal Injury
- Localized discomfort on the knee’s medial or lateral surfaces.
- Sounds of locking and clicking.
- intermittent swelling that is delayed.
A complete history and physical examination are the foundation for diagnosing a torn meniscus. Imaging tests like an MRI, X-ray, or arthroscopy may also need to be performed to confirm a diagnosis.
Meniscal injuries should be treated right away using the RICER method (rest, ice, compression, elevation, and referral). For quick medical attention and pain relief, this protocol must be followed within 48–72 hours. Furthermore, the No HARM protocol needs to be followed, which prohibits the use of heat, alcohol, running, and massage. It lessens the injured knee’s edema and bleeding.
Stability and support for your knee joints can be increased by strengthening the muscles in your legs and around your knees through physical therapy. Even a knee brace made especially to support a meniscus injury might be required for the patient to wear. The doctor might suggest surgery, though, if the pain doesn’t go away and your knee locks up despite treatment.
Following a meniscal tear, a favorable prognosis is achievable. Patients can either have surgery or receive conservative care to accomplish this. Athletes can go back to their original sports and compete. It is also true that cartilage cannot be restored to its pre-damage state after it has occurred. For this reason, everyone has to look for preventative measures (like strengthening the surrounding muscles, maintaining a healthy weight, or using appropriate body mechanics) to avoid a torn meniscus.
Bursitis
Little fluid-filled sacs called bursae cushion the knee joints and make it easier for tendons and ligaments to glide over them.
When these sacs are overworked or repeatedly compressed when kneeling, they can enlarge and become inflammatory. We refer to this as bursitis.
Self-care can be used to treat bursitis in most situations, which are not significant. However, in certain cases, antibiotics may be necessary, as well as aspiration—a needle-assisted operation used to remove extra fluid.
Located close to your knee joint, the knee bursae are sacs filled with liquid. When functioning properly, they aid in smooth joint guidance and prevent muscles, ligaments, and tendons from rubbing against the bones.
When one or more bursae become damaged, irritated, or inflammatory, knee bursitis results. Chronic pressure, forceful hits, and repetitive activities (like running) can create grating friction that can result in bursitis. If the joint is kept in one position for an extended period, this gets worse.
Symptoms Of Knee Bursitis
- A dull, aching pain that follows a first sharp or stabbing pain.
- Swelling and redness in the knee’s anterior region.
- Warmth in the vicinity of the joint.
- Discomfort when knelt.
- Heightened discomfort following extended immobilization of the joint.
- Inability to bend or straighten the knee.
Some conditions like arthritis, stress fractures, and tendinitis can occasionally be confused with bursitis. The physical therapist or orthopedic physician will perform a comprehensive examination and order specialized tests (such as an MRI, ultrasound, or X-ray) to accurately diagnose the issue.
Knee bursitis usually goes away on its own with little to no medical intervention. An intervention is intended to relieve symptoms, but in certain circumstances, medical attention may be necessary. This includes simple therapies like lifestyle adjustments, over-the-counter medications, and home cures. Other options for long-lasting symptoms include surgery, aspiration, and corticosteroid injections.
Tendonitis
Patellar tendinitis is the term for knee tendinitis or inflammation. This is damage to the tendon that joins the shinbone and kneecap.
To extend the knee and enable running, jumping, and other physical activity, the patellar tendon cooperates with the front of the thigh.
Tendonitis, also known as “jumper’s knee,” is a common condition among sportsmen who jump a lot. All physically active individuals, however, run the risk of tendinitis.
Overstressed knees are a defining feature of patellar tendinitis, also known as “jumper’s knee” or patellar tendinopathy. In sports like basketball, volleyball, and long jump, where athletes frequently jump or land hard, they frequently sustain this kind of injury. It also happens if you suddenly increase the amount of exercise you do or train on hard surfaces like concrete. Tiny tears caused by the increased strain on the tendon cause the muscle to become inflamed.
The typical course of patellar tendinitis pain is gradual. It was even possible for athletes to train and compete with mild to moderate symptoms. When first injured, the wound might not cause any issues and would frequently heal fast. If it happens frequently, though, the tears might appear before the body can heal. There will eventually be more damage, which will cause pain and dysfunction.
Symptoms Of Patellar Tendonitis
- Pain and tenderness below the kneecap.
- discomfort that is exacerbated by prolonged sitting, running, jumping, and landing.
- Weakness in the knee.
Your doctor will examine and feel different parts of your knee to identify painful spots to diagnose the issue. This will be at the front of your knee, directly below the kneecap, if you have patellar tendonitis.
Doctors will also perform imaging tests, such as MRIs, ultrasounds, and X-rays, to get a more definitive diagnosis.
Physiotherapy and possibly extended rehabilitation are other medical interventions for this injury. You can return to the court, track, or field as soon as possible with the right injury care and rehabilitation.
Tendon Tears
It is possible to tear and stretch the patellar tendons and quadriceps. While tears are more common in middle-aged individuals who participate in sports involving running or jumping, injuries to these tendons can occur to anyone. Common causes of injuries to the knee tendon include falls, direct force applied to the front of the knee, and awkward landings from jumps.
The soft tissues called tendons connect the muscles to the bones. Patellar tendon injuries occur often in the knee. An athletic or middle-aged individual who engages in physical activity frequently tears or overstretches their tendons. The tendon may also tear as a result of direct impact from a fall or hit.
Iliotibial band syndrome
Among long-distance runners, iliotibial band syndrome is widespread. The iliotibial band, which is situated outside the knee, rubbing on the exterior of the knee joint is what causes it.
Usually, the discomfort begins as a slight annoyance. Eventually, it might get so bad that a runner needs to stop running in order to give their iliotibial band time to heal.
The thick band of fascia that runs the entire length of your thigh and ends at the top of your shin is known as the iliotibial band (ITB) or iliotibial tract. The dense fibrous connective tissue that starts at the iliac crest and inserts at the knee makes up this structure. The ITB and the muscles that it contracts are responsible for the hip’s lateral rotation, abduction, and extension.
Iliotibial Band Syndrome is thought to be a non-traumatic overuse injury linked to underlying hip abductor muscle weakness. Knee pain on the outside of the knee, typically experienced by runners and cyclists, is a result of overuse caused by repetitive knee flexion and extension. It is also linked to sports like basketball, swimming, hockey, cycling, and hiking.
Symptoms Of Iliotibial Band Syndrome
- Palpable pain and/or tenderness on the outside of the knee.
- Pain that lingers after working out.
- Clicking sensation.
- Sensitivity in the lower back.
- The skin around the knee is red and warm.
With the help of your medical history, which describes your current symptoms and problems, a diagnosis can be made. A physical examination and a comprehensive evaluation of the strength and range of motion of your knees will also be part of this. Your doctor can differentiate meniscal tears and osteoarthritis from iliotibial band syndrome and other possible causes of your knee pain with specific tests. An MRI or X-ray would need to be performed to make a conclusive diagnosis.
The majority of people react well to cold compresses, stretching, strengthening, and anti-inflammatory drugs. To minimize discomfort, stop additional injury, and give the knee time to heal completely, it is also essential to temporarily restrict one’s activities. Sometimes recommended methods of reducing tension include electrotherapy and ultrasound. Some may even need surgery to treat the injury in the interim.
The majority of iliotibial band syndrome patients recover, but it typically takes weeks or months for them to resume their normal activities pain-free.
Fractures
The patella is the bone that is most frequently broken near the knee. It is also possible for the ends of the femur and tibia to break where they join to form the knee joint. High-energy trauma, such as falls from considerable heights and car crashes, is the primary cause of many fractures around the knee.
It is possible for any of the bones in or near the knee to break. The patella, or kneecap, is the most often broken bone in the joint. Most knee fractures result from high-impact trauma, such as falls or auto accidents. Even a small misstep or trip can result in a knee fracture in someone with underlying osteoporosis.
Serious knee injuries that can cause significant impairment are patellar fractures. This happens when you land on your kneecap directly, when you overuse your knee, or when you receive a direct blow or trauma. A fracture may occur if the stress exceeds the bone’s capacity to withstand. The location, severity, and kind of these injuries can all change.
Symptoms Of Patellar Fracture
- The front of the knee is suddenly very painful and sharp.
- Swelling.
- A noticeable imperfection in the kneecap.
- Foot not being able to be lifted.
- Obvious deformity (in severe cases).
A physical examination, radiological results, and an assessment of the injury’s mechanism of acquisition are used to make a diagnosis. Repositioning, surgery, or the use of protective and functional equipment (such as crutches, plaster casts, or knee braces) may be necessary as part of the treatment. Rehabilitating athletes can be accomplished through safe and efficient gradual patellar conditioning.
When treated appropriately, patients who suffer from patellar fractures typically recover completely. With the careful supervision of their physiotherapist or other specialist, they can return to sports in a matter of weeks or months. Osteomalacia, patellofemoral pain syndrome, and post-traumatic arthritis are a few disorders that may arise from this kind of fracture if rehabilitation is not adequate.
Osgood-Schlatter Disease
A common overuse injury known as Osgood-Schlatter Disease causes pain and inflammation to the growth plate at the tibial tuberosity. It is more common in adolescents who play sports that require sprinting, jumping, and sudden direction changes, and it mainly affects them during growth spurts.
Symptoms Of Osgood-Schlatter Disease
- Patellar tendon swelling and tibial tuberosity.
- Tibial tuberosity, the bony protrusion below the kneecap, is the site of pain, swelling, and tenderness.
- Discomfort that is worse when squatting, running, or jumping.
- Temporary pain alleviation while resting.
In addition to anti-inflammatory drugs and physical therapy to strengthen the surrounding muscles, treatment usually consists of rest, ice, compression, and elevation (RICE). The growth plate closing usually takes care of the condition on its own.
Dislocation
When the knee’s bones are partially or totally out of alignment, it results in a dislocation. The patella may slip out of place, For instance, or the tibia and femur may be forced out of alignment.
An anomaly in the knee’s structure may result in dislocations. The most common cause of dislocations in individuals with normal knee structure is high-energy trauma, which includes collisions in cars, sports, and falls.
When the knee’s bones are misaligned or out of alignment, the knee can become dislocated.
One or more bones may come out of position in a dislocated knee. A knee dislocation may result from trauma or structural problems, such as those sustained in falls, auto accidents, or contact sports.
There are two types of knee dislocations: high-velocity and low-velocity. The most common cause of high-velocity knee dislocations is a violent force, like an automobile accident. On the other hand, low-velocity knee dislocations frequently happen in athletic environments.
When an athlete plants their foot on the ground and quickly changes direction, they risk dislocating their knee. There is a twisting movement. In sports like soccer, cycling, skiing, gymnastics, and long jumping, this is typical.
Symptoms Of Knee Dislocation
- Sudden, severe swelling.
- Severe pain and tenderness.
- “Sloppy” kneecap (hypermobile patella).
- An obvious knee deformity.
- Weakness or lack of pulse below the knee.
The doctor will first check distal pulses to rule out injury, particularly on the foot since vascular damage is frequently associated with knee dislocation. To assess the level of bone damage, they might also prescribe an X-ray. In certain situations, an ultrasound may be used to evaluate arterial blood flow, while an arteriogram—an X-ray of the artery—may be performed on patients to look for arterial damage.
Relocation (putting the lower leg back into place through a procedure known as reduction), surgery (which includes knee reconstruction and vascular repair to preserve blood flow), and immobilization are all part of the treatment.
A dislocation is regarded as a serious injury. Even though recovery is possible, the injured knee typically loses its ability to withstand stress. Physicians frequently recommend the use of bracing wraps or other devices to protect the knee and keep it from experiencing excessive strain.
Quadriceps & Hamstring Strains
There are two main groups of muscles in your thigh: the quadriceps and the hamstrings. The semitendinosus, semimembranosus, and biceps femoris are the three muscles that make up the hamstring. They run along the back of your leg from your thigh to your knee.
Together, these muscles allow for hip extension and knee flexion. On the anterior portion of your thigh, in the space between your hip and knee, are the quadriceps muscles. They are connected to your hip bones, patella (kneecaps), femur (thigh bones), and pelvis by their corresponding tendons.
Common muscle injuries that result from overstretching of the muscle fibers that tear are quadriceps and hamstring strains. Sports involving sprinting, jumping, or abrupt direction changes are prone to these injuries.
Symptoms Of Quadriceps And Hamstring Strains
- Sharp pain that suddenly appears in the hamstrings or quadriceps of the thigh.
- Swelling and bruising.
- walking or bearing weight with the afflicted leg being difficult.
To reduce pain and swelling, treatment for these injuries usually consists of rest, ice, compression, and elevation, or RICE. It might also be required to undergo physical therapy to help the injured muscles regain their strength and flexibility.
Which knee injuries are likely to happen after a fall?
These eight knee injuries are the most frequent ones that can happen after a fall, ranging in severity from minor to severe.
Abrasion
A scrape is also known as an abrasion. When the skin comes into contact with a rough surface, like cement or asphalt, this happens.
A minor abrasion only removes the epidermis, or outer layer of skin, and can be treated at home. Serious abrasions involving multiple layers of skin and bleeding might require medical care.
Laceration
A laceration is a wound from a cut or puncture that tears or punctures the skin.
A laceration may result from falling and landing on something sharp, such as a nail. Similar to abrasions, lacerations can range in severity from very shallow, requiring medical attention, to minor, with little to no bleeding.
You could also get tetanus from cuts brought on by rusty objects, like a nail. If this happens, get medical attention as soon as possible.
Contusion
A common injury from falling on a hard surface is a bruise or contusion to the knee.
The impact may result in blood leaking from a blood vessel or capillary in the skin or muscle beneath into the surrounding area, giving rise to the characteristic black and blue bruise.
Usually, at-home care for a bruised knee consists of rest, ice, elevation, and, if necessary, over-the-counter anti-inflammatory drugs like ibuprofen.
Sprain
One or more of the knee’s ligaments becoming overextended can result in a sprain.
A ligament is a type of structure that joins two bones together. A knee sprain could happen if you take a hard fall or are struck by something heavy or strong, like a football tackle.
You can typically recuperate at home and take care of your sprain. Consult a physician if:
- There’s a lot of swelling.
- Severe pain.
- Your knee moves very difficultly for you.
Torn meniscus
Located between the femur and tibia, the meniscus is a rubbery piece of cartilage that serves to support and cushion the two bones.
Meniscus tears typically happen during a hard fall, but they can also happen during a sharp turn in sports like football or basketball.
While some meniscus tears can be treated conservatively (i.e., without surgery), persistent pain and/or swelling could indicate that your torn meniscus needs to be repaired surgically.
Tendon tear
In the knee, there are two primary tendons:
- Quadriceps tendon: The tendon that attaches the quadriceps muscle in the front of the thigh to the patella (kneecap) is called the quadriceps tendon.
- Patellar tendon: The tibia (shinbone) and the base of the patella are joined by the patellar tendon. Both injuries can be caused by a fall onto the front of the knee or by missing a step and landing awkwardly. Patellar tendon tears are more common.
Torn ligament
The tibia and femur, or thighbone, are joined by four major ligaments in the knee, which enable side-to-side rotation, forward and backward motion:
- An anterior cruciate ligament (ACL).
- Posterior cruciate ligament (PCL).
- Medial collateral ligament (MCL).
- Lateral collateral ligament (LCL).
One or more of these ligaments may tear as a result of a high-impact injury like a fall or blow to the side of the knee.
A torn ligament is frequently repaired with surgery. A torn ligament can cause persistent pain and disability in the injured knee if left untreated.
Knee dislocation
Though they are rare, dislocated knees are extremely serious injuries that need to be treated right away.
Low-energy injuries can also cause a dislocated knee by pushing the thighbone out of alignment with the shinbone. High-energy injuries, such as those sustained in auto accidents or falls from significant heights, are the most common cause of dislocated knees.
Following a dislocated knee, complications like blood vessel and nerve damage are common and necessitate prompt medical attention.
Symptoms
The source of the problem may affect the knee pain’s location and intensity. Signs and symptoms that sometimes accompany knee pain involve:
- Swelling and stiffness.
- Touch-sensitive redness and warmth.
- Weakness or instability.
- Sounds of popping or crunching.
- Not being able to extend the knee to its fullest.
Causes
Injuries, mechanical issues, various forms of arthritis, and other conditions can all result in knee pain.
A knee injury may affect the bones, cartilage, ligaments, and tendons that form the knee joint as well as the fluid-filled sacs (bursae) that surround the joint. Among the more typical knee injuries are:
- ACL injury: As one of the four ligaments connecting your shinbone to your thighbone, the anterior cruciate ligament (ACL) can tear and result in an ACL injury. People playing basketball, soccer, or other sports involving quick direction changes are likelier to suffer an ACL injury.
- Fractures: Accidents involving falls or cars can break the bones in the knee, including the patella, or kneecap. Additionally, osteoporosis patients may occasionally suffer a knee fracture from simply taking the wrong step.
- Torn meniscus: Your shinbone and thighbone are separated by a tough, rubbery cartilage called the meniscus, which serves as a shock absorber. Knee tears can occur if you twist it suddenly while bearing weight on it.
- Knee bursitis: Inflammation in the bursae, which are tiny fluid-filled sacs that cushion the outside of your knee joint and allow ligaments and tendons to glide over it smoothly, is a common side effect of acute knee injuries.
- Patellar tendinitis: One or more tendons—the thick, fibrous tissues that connect muscles to bones—can become inflamed and irritated when someone has tendinitis. The patellar tendon, which extends from the kneecap (patella) to the shinbone and permits jumping, running, and kicks, can become inflamed. Patellar tendinitis can affect runners, skiers, cyclists, and participants in jumping sports and activities.
- Dislocated kneecap: This suggests that your kneecap sliding out of place is the source of your knee pain and swelling. Your physician might refer to this as a “patellar dislocation.”
- Patellofemoral pain syndrome: Muscle imbalances, tightness, and problems with leg alignment are the usual causes of this illness. It causes knee pain and intermittent “buckling,” or your knee’s incapacity to bear your weight. There’s no wound to blame. Women are impacted more frequently than males are.
- IT (iliotibial) band syndrome: Tough tissue that extends from your hip to the outside of your knee is called the iliotibial (IT) band. Overindulgence in activity has the potential to worsen over time. The outside of the knee hurts as a result. It’s a typical occurrence for runners traveling downhill.
- Meniscal tear: Sometimes, a knee injury will cause cartilage to tear. These sharp edges have the potential to become lodged in the joint, resulting in discomfort and inflammation. People frequently experience a “catching” feeling in their joints as they are moving.
- Osgood-Schlatter disease: In youth, when bones and other knee components are still developing, this problem occurs. Where a tendon from the kneecap attaches to the shin below the knee, it may result in an excruciating lump. Excessive exercise and irritation at the tibial tubercle, a point on the underside of the knee, are common causes of pain in this region. The pain might come and disappear in due course. It is particularly prevalent among teenage girls and boys.
- Osteoarthritis: This kind of arthritis is known as “wear and tear.” For people over 50, it’s the leading cause of knee discomfort. When you exercise, this disease makes your knee joint hurt or bulge. Osteoarthritis-affected joints may also be stiff in the morning.
Mechanical problems
The following are a few instances of mechanical issues that can result in knee pain:
- Loose body: Occasionally, a fragment of bone or cartilage may break off and float in the joint space due to damage or degeneration. Unless the loose body restricts the movement of the knee joint, this might not cause any issues. In that case, the situation would resemble a pencil stuck in a door hinge.
- Iliotibial band syndrome: This happens when your iliotibial band, a strong band of tissue that runs from the outside of your hip to the outside of your knee, gets so tight that it causes friction against the outside of your thighbone. Particularly vulnerable to iliotibial band syndrome are cyclists and distance runners.
- Dislocated kneecap: This happens when the patella, the triangular bone covering the front of the knee, slips out of position, usually to the outside of the knee. There are situations where the kneecap may remain dislocated and visible.
- Hip or foot discomfort: If you experience foot or hip discomfort, you can modify your gait to spare your hurting joint. However, this changed gait may put additional strain on your knee, leading to knee pain.
Types of arthritis
There are over a hundred varieties of arthritis. The following types are most likely to impact the knee:
- Osteoarthritis: Osteoarthritis, the most prevalent kind of arthritis, is also referred to as degenerative arthritis. It’s a wear-and-tear ailment brought on by the deterioration of knee cartilage with age and use.
- Rheumatoid arthritis: Rheumatoid arthritis, the most crippling type of arthritis, is an autoimmune disease that can affect practically any joint in the body, including the knees. Rheumatoid arthritis is a chronic condition, but its severity can vary and it may even come and go.
- Gout: Uric acid crystals accumulate in the joint and cause this kind of arthritis. Although it typically affects the big toe, gout can also occur in the knee.
- Pseudogout: Crystals containing calcium that form in the joint fluid are the cause of pseudogout, which is frequently confused with gout. The most common joint to experience pseudogout symptoms is the knee.
- Septic arthritis: An infection in your knee joint can occasionally cause swelling, pain, and redness. Fever is a common symptom of septic arthritis, and pain rarely appears before trauma. Deep damage to the knee cartilage can occur rapidly from septic arthritis. If you have knee pain along with any of the septic arthritis symptoms, Visit your physician immediately.
Other problems
Pain between the kneecap and the underlying thighbone is commonly referred to as patellofemoral pain syndrome. This condition is frequently observed in athletes, young adults, particularly those whose kneecap is malaligned in its groove, and older adults, who typically have kneecap arthritis as the underlying cause.
Risk factors
Several factors can raise your risk of developing knee issues, such as:
- Excess weight: Even during routine activities like walking or stair climbing, being overweight or obese puts more strain on your knee joints. Due to the acceleration of joint cartilage degradation, it also raises your risk of developing osteoarthritis.
- Occupations: Repetitive motions at work, such as squatting or kneeling, may increase your risk of developing knee conditions, just like playing sports.
- Lack of muscle flexibility or strength: Knee injuries may be more likely in people who lack strength and flexibility. Robust muscles support and shield your joints, while supple muscles enable you to move through your entire range of motion.
- Falling or Trauma: Individuals who trip and fall or are in auto accidents may sustain fractures and dislocations to their knees. These injuries can occasionally be avoided. However, you might be able to reduce your risk of knee trauma if you take the right safety precautions.
- Certain sports or occupations: More sports-related strain is placed on the knees than in other sports. Your risk of knee injury is increased by basketball jumps and pivots, alpine skiing with its stiff ski boots and potential for falls, and running or jogging, which repeatedly pounds your knees. Your risk may also be increased by jobs like farming or construction that involve repetitive strain on the knees.
- Previous injury: The likelihood of suffering another knee injury increases if you have had one in the past.
- Genetics & Family History: Some people are more likely to develop diseases like osteoarthritis, which increases the risk of injury to the knee. Furthermore, some people have extra joint space from birth, which makes the knee less stable.
Complications
Not every knee ache is severe. On the other hand, if left untreated, certain knee injuries and illnesses, like osteoarthritis, can worsen pain, damage to the joint, and disability. Further, even a small-scale knee injury increases your risk of future injuries of a similar nature.
Diagnosis
In the course of the physical examination, your physician may:
- Examine your knee for signs of visible bruising, warmth, tenderness, pain, and swelling.
- Measure your lower leg’s range of motion in various directions.
- To assess the stability of the structures in your knee, apply pressure or tension to the joint.
Imaging tests
In certain situations, your physician may recommend tests like:
- X-ray: To identify bone fractures and degenerative joint disease, your doctor might first advise getting an X-ray.
- Computerized tomography (CT) scan: CT scanners produce cross-sectional images of your interior body by combining X-rays from various angles. CT scans help identify minor bone problems and fractures. Even in cases where there is no inflammation in the joint, gout can be correctly diagnosed using a specific type of CT scan.
- Ultrasound: This technology creates real-time images of the soft tissue structures in and around your knee using sound waves. During the ultrasound, your doctor might want to adjust the position of your knee to look for certain issues.
- Magnetic resonance imaging (MRI): An MRI generates three-dimensional images of the inside of your knee using radio waves and a strong magnet. When it comes to identifying damage to soft tissues like ligaments, tendons, cartilage, and muscles, this test is especially helpful.
Lab tests
Blood tests and occasionally an arthrocentesis procedure—which involves using a needle to remove a small amount of fluid from inside your knee joint and sending it to a lab for analysis—will likely be performed if your doctor suspects an infection or inflammation.
When to see your doctor
Someone should see a doctor if their knee discomfort gets severe, chronic, or lasts more than a week. If there’s a decrease in joint range of motion or if bending the knee becomes challenging, it’s critical to consult a physician.
A doctor should be consulted right away following an injury in cases of trauma or blunt force.
You ought to contact a doctor about medicine if:
- I have excruciating knee pain.
- You were hurt or involved in an accident recently.
- One cannot kneel and walk.
- The knee seems unsteady, as though it would buckle or give way.
- Your knee cannot be fully bent or straightened.
- The knee appears malformed.
An injury to the knee, such as a bruise, can hurt. However, unless there is uncontrollable bleeding, this type of injury usually does not require medical attention.
Other signs that point to the urgent need for medical intervention include:
- Experiencing a “pop” sound during your fall, as this is frequently linked to a ruptured ligament.
- Another common symptom of a torn ligament is the sensation that the knee is unstable, buckles, or gives way.
- An injury or ripped ligament may be indicated by knee swelling.
- Inflammation resulting from a torn tendon or muscle may be the cause of your knee feeling warm to the touch following a fall. Infections or bursitis can also be indicated by heat.
- Your knee may have structural damage if you are unable to bear weight on it.
- If bleeding from a cut or scrape continues for more than a few minutes, you should get help.
- An infection may be indicated by the area surrounding a cut or scrape becoming red, swollen, or seeping pus sometime after the injury.
Treatment of Knee Injuries
The RICE protocol can expedite your healing when you are first hurt:
- Rest — Give the damaged joint no use for at least two days.
- Ice: Apply cold packs multiple times a day, for 20 minutes at a time. Avoid putting ice right on your skin.
- Compression: Apply a thin bandage or ace wrap to the injured area.
- Elevation: Raise the injury above your heart while you’re at rest to help with swelling.
Make sure you get help as soon as you can, particularly if you:
- Feel your knee give out at the moment of injury and hear a popping sound.
- Experience excruciating pain.
- Unable to move the knee.
- Start to limp.
- Have edema where the wound was sustained.
The recommended course of treatment by your physician will vary depending on several factors, including the extent of your injury, your age, overall health, and level of activity.
You can take painkillers as prescribed by your physician or chemist. Applying heat or massage to a knee injury is not recommended. While the wound is healing, stay off alcohol and don’t run.
Your physician might prescribe an MRI, CT, or x-ray. For knee injuries, these imaging examinations aren’t always advised. Frequently, discussing the incident and having a physical assessment by a physician will be equally beneficial.
The majority of patients with knee injuries require both guided rehabilitation and physiotherapy.
For more severe knee injuries, several therapies could be needed:
- ACL rupture: Almost always, surgery is required for ACL ruptures, and recovery can take up to a year.
- PCL rupture: A long hinged knee brace will likely immobilise the knee. A six- to ten-week period of rehabilitation is required.
- Other ligament injuries: A hinged knee brace is used during treatment, and six to twelve weeks of rehabilitation are thereafter required.
- Meniscal tear: Rest and physical treatment are typically advised. An arthroscopy may be required occasionally.
- Dislocated kneecap or fracture: To prevent future dislocation, the knee joint will be immobilized, and arthroscopy and physiotherapy may be required.
See your physician once more if:
- After a few days, the soreness or swelling doesn’t go down.
- The signs and symptoms worsen.
- You get a fever or your knee becomes red.
Furthermore, the knee can be harmed by underlying medical conditions like systemic lupus erythematosus, rheumatoid arthritis, and osteoarthritis.
Treatment options will change based on the precise cause of your knee pain.
Nonsurgical Treatment
Numerous knee injuries are manageable with basic techniques like:
- Immobilization: To keep your knee from moving, your doctor might advise getting a brace. A cast or brace may help hold your fractured bones in place while they heal. Your knee may be further protected by crutches, which prevent you from bearing weight on your leg.
- Physical therapy: You can strengthen the leg muscles that support your knee and get it back to working order with certain exercises.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Ibuprofen and naproxen, two anti-inflammatory medications, lessen pain and swelling.
Medications
If your knee pain is being caused by a medical condition like gout or rheumatoid arthritis, your doctor may prescribe medication to help relieve the pain.
Injections
Your doctor might advise injecting drugs or other materials straight into your joint in specific circumstances.
Examples involve:
- Corticosteroids: A corticosteroid medication injected into your knee joint may help lessen the symptoms of an arthritis flare-up and offer temporary pain relief. Not every instance of these injections results in success.
- Hyaluronic acid: Hyaluronic acid, a thick fluid that resembles the fluid that naturally lubricates joints, can be injected into your knee to increase your range of motion and reduce pain. Even though research on this treatment’s efficacy has yielded conflicting results, relief following a single or series of shots may endure up to six months.
- Platelet-rich plasma (PRP): PRP has a concentration of numerous growth factors, which seem to lessen inflammation and aid in the healing process. According to some research, PRP may help some patients with osteoarthritis, but more research is required.
Surgical Treatment
Surgery is often necessary for many fractures and injuries near the knee to fully restore leg function. In certain instances, like numerous ACL tears, arthroscopic surgery can be performed with tiny tools and tiny incisions.
Contrarily, fractures frequently call for open surgery with a wider incision, which gives your surgeon a better view and easier access to the damaged structures.
In most cases, you don’t have to have surgery right away if you have an injury that might require it. Before making a choice, weigh the benefits and drawbacks of surgical reconstruction and nonsurgical rehabilitation about your top priorities. You might have the following options if you decide to have surgery:
- Arthroscopic surgery: Depending on the nature of your injury, your doctor might be able to use a fiber-optic camera and long, narrow tools that are inserted through a few tiny incisions around your knee to examine and repair joint damage. Arthroscopy can be used to reconstruct torn ligaments, remove loose bodies from your knee joint, and repair or remove damaged cartilage—especially if it’s causing your knee to lock.
- Partial knee replacement surgery: During this procedure, your surgeon uses metal and plastic parts to replace just the damaged area of your knee. You’re likely to heal faster from this surgery than from surgery to replace your entire knee because it can usually be done through small incisions.
- Total knee replacement: Your kneecap, shinbone, and thighbone are all surgically removed along with any damaged bone and cartilage, and in their place is an artificial joint composed of polymers, metal alloys, and premium plastics.
- Osteotomy: The purpose of this procedure is to better align the knee and relieve arthritis pain by extracting bone from the shinbone or thighbone. You might be able to postpone or avoid having a total knee replacement with this surgery.
Physical therapy
Your knee will become more stable if you strengthen the surrounding muscles. Depending on the particular condition causing your pain, your doctor might suggest physical therapy or various strengthening exercises.
Exercises may be necessary if you engage in physical activity or play a sport to establish proper technique during your activity and to correct movement patterns that might be harming your knees. Exercises that increase your balance and flexibility are also crucial.
Arch supports, which occasionally have wedges on one side of the heel, can assist in distributing pressure off the osteoarthritis-affected side of the knee. To help support and shield the knee joint under specific circumstances, several brace styles may be utilized.
How is knee pain treated after a fall?
When treating a fall-related knee injury, rest and, if required, a brace to stabilize the joint are the usual courses of action. Anti-inflammatory painkillers like ibuprofen (Advil, Motrin) may be beneficial in the majority of cases.
Many times, minor knee injuries can be healed at home. Nonetheless, it’s critical to visit a physician if symptoms worsen or if the pain is accompanied by:
- Considerable swelling of the joints.
- A lack of capacity to support weight.
- A feeling of yielding.
- More indications of tendon or ligament injury.
Surgery might be required if the injury is severe to restore function and relieve pain.
Which exercises are advised against during the recovery process for a knee injury?
The patient will receive targeted exercises from the physical therapist to stabilize and strengthen the knee joint during physical therapy for the rehabilitation of a knee injury. Strengthening the quadriceps, hamstrings, calf, and hip are among the thigh’s top muscles targeted by these exercises. Before beginning any exercise regimen, get advice from your physical therapist and doctor. Before you attempt the exercises on your own, your physical therapist should make sure you execute them correctly.
See your physician or physical therapist if you experience any pain or discomfort while performing the recommended exercises.
The following are some exercises that your physical therapist might suggest:
- Quad sets.
- Straight leg raises: Straight-leg raises to the front.
Straight-leg raises to the back. - Hamstring curls.
- Heel raises.
- Heel dig bridging.
- Shallow standing knee bends.
There is an exercise guide available from the American Academy of Orthopedic Surgeons (AAOS) that has illustrations and instructions. Be sure to speak with your physician or physical therapist before performing any of these exercises independently.
The following are some exercises you should avoid doing after a knee injury:
- Full-arc knee extensions.
- Lunges.
- Deep squats.
- Hurdler’s stretches.
- These exercises may aggravate knee joints that are already damaged.
How long does it take to heal from an injury to the knee?
The kind and extent of a knee injury determine how long it will take to heal. A more extensive recovery period may be necessary if the injury is such that surgery and/or physical therapy are necessary.
- A simple sprain or strain may persist for a week or two.
- Healing from more serious injuries that need arthroscopic surgery can take one to three months.
- Knee trauma that is severe enough to require a year to heal.
Recovery will go more quickly if you adhere to the doctor’s recommendations for immobilization, rest, staying off your feet, and avoiding strenuous exercise that could aggravate the injuries.
Also, physical therapy can expedite the healing process. To make sure you are performing the exercises correctly and getting the best results, it is crucial to adhere to your physical therapist’s instructions.
There may be periodic flare-ups from non-surgical chronic knee injuries. For short-term relief, cortisone injections, anti-inflammatory drugs, and physical therapy are utilized.
What is the prognosis for a knee injury?
The kind and extent of the injury determine the prognosis for a knee injury.
The majority of mild knee injuries, such as strains and minor sprains, heal on their own with conservative care. For these kinds of injuries, the prognosis is favorable.
Surgery may be necessary if injuries to the ligaments or cartilage cause the knee to malfunction or become unstable. Patients can eventually regain their entire or nearly full range of motion in their knees thanks to these injuries, which typically respond well to surgery.
Prevention
Although preventing knee injuries isn’t always feasible, there are steps one can take to lower the chance. People who run or participate in sports, for example, should wear the proper footwear and safety equipment.
One might want to think about cutting back on their running mileage if they have overuse injuries or iliotibial band syndrome.
To help prevent injuries, several workouts also develop the muscles in the smaller legs. Lastly, stretching both before and after exercise can aid in preventing knee injuries.
It’s also crucial to eat healthily, particularly for athletes. The maintenance of healthy bones, muscles, and ligaments depends on protein, calcium, and vitamin D.
Although preventing knee pain isn’t always possible, the following tips might help avoid injuries and degenerative joint disease:
- Keep extra pounds off: It’s one of the best things you can do for your knees to maintain a healthy weight. Your joints are under more stress with every extra pound you gain, which raises your risk of osteoarthritis and other injuries.
- Be in shape to play your sport: Make time for conditioning to get your muscles ready for the rigors of playing sports.
- Practice perfectly: Make sure that your sports or activity-related technique and movement patterns are as good as they can be. Professional guidance can be very beneficial.
- Get strong, and stay flexible: One of the main causes of knee injuries is weak muscles. It will help you to strengthen the muscles on the front and rear of your thighs that support your knees, called quadriceps and hamstrings. The efficiency with which the muscles surrounding your knees cooperate is improved by training for balance and stability.
- In addition, stretching is crucial because taut muscles can also lead to injury. Incorporate some flexibility exercises into your training regimen.
- Be smart about exercise: Should you suffer from osteoarthritis, persistent knee pain, or recurrent injuries, it might be necessary to modify your exercise regimen. At least for a few days a week, think about moving to low-impact activities like swimming, water aerobics, or other sports. Occasionally, relief can be obtained by merely reducing high-impact activities.
Summary
Common knee injuries involve ligament, tendon, and cartilage tears, and patellofemoral pain syndrome. Any knee injury that is treated medically quickly improves the patient’s chances of making a full recovery.PT, arthroscopic surgery, and open surgery are available as treatment options.
The components of your knee joint are cartilage, ligaments, fluid, and bone. Tendons and muscles facilitate knee joint movement. Knee problems occur when any of these structures are injured or diseased. Knee issues can lead to pain and make walking difficult.
People of all ages experience extremely common knee problems. Knee issues can make it difficult to do anything, even get out of a chair and walk, let alone play sports. This could significantly affect your life.
The most prevalent condition affecting the knee is osteoarthritis. As the knee’s cartilage progressively deteriorates, pain and swelling result.
Knee issues can also be caused by injuries to the ligaments and tendons. The anterior cruciate ligament is frequently injured (ACL).ACL injuries are typically caused by abrupt twisting motions. ACLs and other knee injuries are frequent sports-related ailments.
The cause of knee issues will determine how to treat them. In certain circumstances, your physician might advise knee replacement.
FAQs
How can I determine the severity of my knee injury?
Swelling is a crucial symptom to watch out for. “Severe injuries result in significant knee swelling, particularly in younger patients,” says Christina Allen, MD, head of the Sports Medicine division. This is particularly true if the swelling appears suddenly.
What are the 3 most common knee injuries?
Sprains, which are caused by overstretching the knee ligaments, torn ligaments, such as the anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL), and strains, which are caused by overstretching the muscles and tendons, are common knee injuries.
What is the estimated healing time for a knee injury?
The healing time for soft tissue knee injuries varies from 6 to 12 weeks, depending on their severity. Pain and Swelling: You might have swelling in your knee. Your leg will benefit from rest and elevation.
Is it acceptable to walk with a knee injury?
Your knee won’t get any worse while you walk. Always attempt to walk normally, that is, with your heel down. Early on after an injury, excessive weight bearing may make pain and swelling worse. To assist you with this, crutches might be provided for a brief period.
Can knee injuries heal on their own?
While minor knee injuries might heal on their own, all injuries need to be examined and diagnosed by a physician or physical therapist. Expert assistance is required for persistent knee pain. Any knee injury has a better chance of recovering fully if medical attention is sought out quickly.
How do you treat a damaged knee?
The RICE method is typically effective in treating knee pain at home: Rest: To prevent aggravating the injury, cease the physical activity that is causing you pain. Ice: For the first 24 hours following your injury, apply an ice pack or cold compress for 15 to 20 minutes every hour. You can start applying ice every three to four hours after a day.
Which five signs indicate a knee injury?
You require immediate medical assistance if:
Your knee joint is crooked or twisted.
The moment the injury occurred, there was a “popping” sound.
You can’t put weight on your knee.
You’re in excruciating pain.
Your knee suddenly grew larger.
Should I wrap my knee if it hurts?
Embrace your knee.
Alternatively, use a knee brace for assistance. We refer to this as compression. Although not too tight, the wrap should be snug. The proper compression should be able to reduce knee swelling.
What is the treatment for a knee injury?
Make use of “RICE.”For knee pain brought on by a small injury or a flare-up of arthritis, RICE (rest, ice, compression, and elevation) is beneficial. Rest your knee, use ice to reduce swelling, wrap it in a compressive bandage, and keep it raised. Remember how much you weigh.
What is the quickest way for a knee injury to heal?
Self-care techniques for a knee injury include:
Rest — Give the damaged joint no use for at least two days.
Ice: Apply cold packs multiple times a day, for 20 minutes at a time. Avoid putting ice right on your skin.
Compression: Apply a thin bandage or ace wrap to the injured area.
Elevation: Raise the injury above your heart while you’re at rest to help with swelling.
Can a knee be repaired without surgery?
Treatments for Minimally Invasive Knee Pain
Injections and implantations of autologous cells or stem cells hold great promise for the future of joint therapy. These therapies entail taking a patient’s stem cells or chondrocytes—bone marrow cells that form cartilage—and cultivating them in a lab.
Is it OK to exercise an injured knee?
Your knee pain shouldn’t get worse after you exercise. However, as the body adjusts to new movements, trying out new exercises can occasionally result in temporary muscle soreness.
Which workouts are best avoided if you have a knee injury?
Exercises like running, jumping, and deep squats that put a lot of strain on the knees should be avoided as they can cause joint hypermobility. Select more moderate workouts that will keep you in shape without aggravating your knee pain. Go for a walk.
Can you bend your knee with a knee injury?
The majority of knee injuries hurt. Another symptom of a knee injury is the knee “giving way,” “locking,” or feeling weak. A knee injury may prevent a person from bending or straightening their knee to its full potential. There might be bruises or swelling on the hurt knee.
References
- Knee Injuries. (n.d.). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/knee-injuries#:~:text=Common%20knee%20injuries%20include%20fractures,from%20a%20high-impact%20tr.
- orthoinfo.aaos.org%2Fen%2Fdiseases–conditions%2Fcommon-knee-injuries%2F&psig=AOvVaw0fd-e_BwevS2S5O4FPVDoP&ust=1706529350280000&source=images&cd=vfe&opi=89978449&ved=0CBMQjRxqFwoTCJD0h8CDgIQDFQAAAAAdAAAAABAD.
- Common Knee Injuries – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/common-knee-injuries/.
- Knee injuries. (n.d.). Symptoms, Treatments, and Causes | Healthdirect. https://www.healthdirect.gov.au/knee-injuries#:~:text=Common%20knee%20injuries%20include%3A,stretching%20of%20muscles%20and%20tendons).
- El-Feky, Mostafa, and Andrew Dixon. “Popliteal Artery Entrapment Syndrome.” Radiopaedia.org, 15 Apr. 2010, https://doi.org/10.53347/rid-9410.
- “Mayo Clinic: Symptoms and Causes of Knee Pain.” Mayo Clinic, January 25, 2023, www.mayoclinic.org/diseases-conditions/knee-pain/symptoms-causes/syc-20350849.
- Fletcher, Jenna. Ten Common Knee Injuries and Treatment. 9 Sept. 2017, www.medicalnewstoday.com/articles/319324.
- Knee injuries. (n.d.). Better Health Channel. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/knee-injuries
- What’s Causing My Knee Pain? (2016, December 22). WebMD. https://www.webmd.com/pain-management/knee-pain/knee-pain-causes.
- Knee Injuries and Disorders. (n.d.). https://medlineplus.gov/kneeinjuriesanddisorders.html.
- Roland, James. “The Eight Most Common Fall-Related Knee Injuries.” September 22, Healthline.. Healthline, 22 Sept. 2020, www.healthline.com/health/8-most-common-knee-injuries-from-falling.
- Facoep, J. P. C. D. (2023, July 13).The signs, treatments, and recuperation of meniscus tears and knee injuries. MedicineNet. https://www.medicinenet.com/knee_injury_and_meniscus_tears/article.htm.
- Nelson, F. R., & Blauvelt, C. T. (2015, January 1). Musculoskeletal Diseases and Related Terms. Elsevier eBooks. https://doi.org/10.1016/b978-0-323-22158-0.00002-0.
- Dutton, A. A. (2023, April 21). 10 Common Knee Injuries (Especially Among Athletes). Dr. Dutton Orthopaedic & Sports Medicine Clinic In Singapore. https://www.drandrewdutton.com/blog/knee-injuries/.
- Spine, N. (2023, October 19). The 9 Most Common Knee Injuries. NJ Spine & Orthopedic. https://www.njspineandortho.com/the-9-most-common-knee-injuries/.
- Willigmann, A. (n.d.). 5 Most Common Knee Injuries | Rothman Orthopaedic Institute. https://rothmanortho.com/stories/blog/the-5-most-common-knee-injuries.