ULNAR TUNNEL SYNDOME
OVERVIEW :
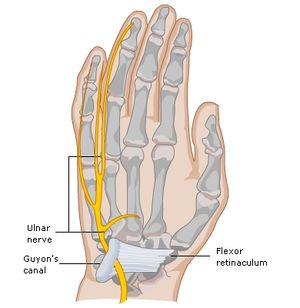
Ulnar tunnel syndrome is a condition that affects the wrist. It happens when the ulnar nerve is compressed going from the wrist into the hand through a space referred to as Guyon’s canal. You may have weakness, tingling, numbness, or pain because of the nerve compression.
The ulnar nerve is a large nerve that runs from your neck to your hand. It’s responsible for some hand movements and function. Bones and muscles don’t protect the ulnar nerve, though, so injuries are common. When you “hit your funny bone” — or experience a feeling of shock after hitting your elbow — that pain comes from the ulnar nerve.
Which are the Causes of Ulnar tunnel syndrome?
Repetitive trauma or chronic pressure is applied to the area of the hand. Repetitive trauma can result from the use of a jackhammer. Chronic pressure can occur in the hand of a bicyclist against the handlebars.
Ulnar tunnel syndrome occurs when the ulnar nerve becomes compressed in the Guyon’s canal region. This is often due to a ganglion developing in the wrist. A ganglion is a fluid-filled lump also known as a cyst and is benign.
- However, anything which places pressure on the ulnar nerve in the wrist can cause ulnar tunnel syndrome, including:
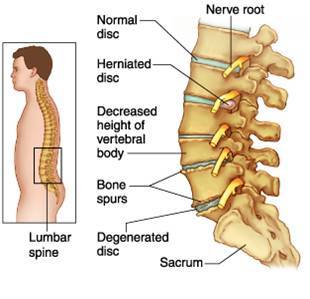
- Changes in osteoarthritis cause pressure on the nerve.
- Tumors in the wrist tissue.
- Enlargement of the bursa (fluid-filled sacs) in the wrist.
- Abnormalities in the muscles or ganglions.
- Fracture of the hook of the hamate in the wrist, a type of injury that golfers or baseball players might experience.
- Ulnar tunnel syndrome can also result from repetitive strain or injury due to sports that put a strain on the wrist. Examples include weight lifting and cycling.
The risk of developing ulnar tunnel syndrome is greater if a person:
- Has had a previous injury to their wrist.
- Performs repetitive tasks with the hands, such as typing.
- Does activities or sports that put the wrist under strain.
- Uses vibrating tools.
Which Symptoms is common in Ulnar tunnel syndrome?
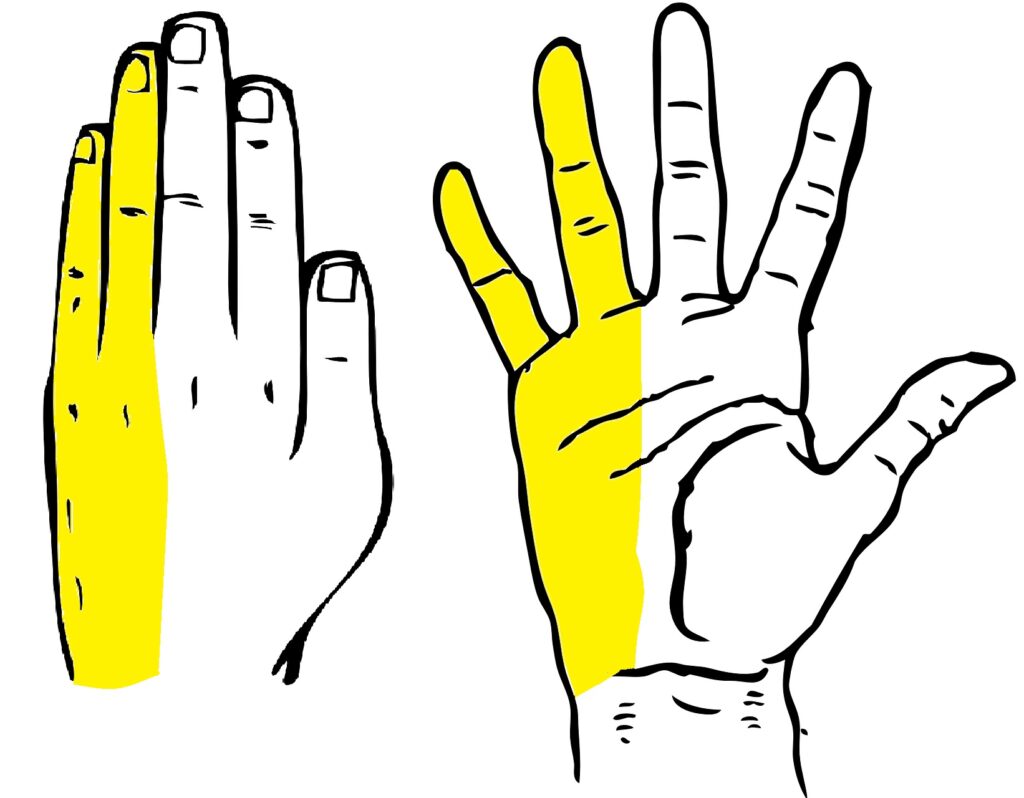
Ulnar tunnel syndrome usually produces symptoms in the hands and wrist, especially the little finger and ring finger. A person with ulnar tunnel syndrome may experience the following:
- Numbness or tingling sensations (paresthesia).
- A burning pain.
- Muscle weakness in the hand.
- Difficulty gripping with the fingers and thumb.
- The hands and fingers bending into a claw shape.
- Fatigue in the hand with repetitive or sustained activities.
- Inability to use fourth and fifth digits for spherical or cylindrical power grips, thumb for adduction, and finger abduction and adduction.
- Decrease ability to perform provoking activity.
- These symptoms can affect the hand, wrist, and fingers and may get progressively worse over time, especially if left untreated. The location of the compression will determine the severity of the symptoms.
CLINICAL PRESENTATION :
As the ulnar nerve passes through Guyon’s canal it splits into deep motor branch and superficial sensory branch.
Guyon’s canal is divided into 3 zones, compression on the ulnar nerve at each zone results in specific symptoms.
Zone 1 :
Zone 1 compression refers to compression at the proximal end of Guyon’s canal, proximal to the bifurcation of the ulnar nerve into sensory and motor branches.
Compression at zone 1 leads to mixed sensory and motor symptoms resulting in sensory dificits over the hypothenar, little finger and the medial half of the ring finger and motor weakness of all ulnar innervated intrinsic muscles.
Zone 2:
Zone 2 compression refers to compression only at the deep motor branch of the nerve, distal to the bifurcation.
Only motor symptoms would develop resulting in motor weakness in the hand muscles innervated by the ulnar nerve.
Compression at zone 2 may occur at pisohamete hiatus after the nerve to abductor digiti minimi takeoff, which would result in weakness in the intrinsic muscles of the hand with possible sparing of the hypothenar muscles.
Zone 3:
Zone 3 compression refers to compression at the superficial sensory branch, it manifests as sensory deficits on the palmer side of the ring finger and the palmer-medial side of the ring finger without hypothenar and interosseous weakness. Compression on the ulnar nerve in zone 1 at the palmer aspect of the nerve can also result in pure sensory symptoms.
EXAMINATION :
HISTORY:
The patient describes sensory symptoms in the little finger and ulnar side of the ring finger and may complain of fatigue or weakness in the hand with repetitive motions and difficulty with some activities, such as opening jars or turning doorknobs.
POSITIVE CLINICAL FINDINGS:
Depending on the severity, there may be atrophy of the hypothenar eminence and intinsic muscles and a partial claw hand posture.
Results of tests include intrinsic muscle weakness, positive Tinel’s sign over the tunnel of Guyon (tapping ulnar nerve).
ASSOCIATED AREAS TO CLEAR:
There can be other causes of ulnar nerve symptoms, such as tension, compression, or restricted mobility of the nerve roots in the cervical intervertebral foramen, the brachial plexus in the thoracic outlet syndrome, or the ulnar nerve as it courses through the bicipital groove; or there could be impingement between the heads of the carpi ulnaris muscle. Therefore, each of these sites must be examined to rule put or determine if any is the causes of the symptoms. In addition, with nerve irritability, it is possible to develop what is known as a double crush injury, so the nerve develops symptoms in other areas along its course as well as at the primary site.
DIAGNOSIS:
IMAGING TEST :
- RADIOGRAPHS
- Useful to evaluate hook of hamate fractures.
- CT SCAN
- Useful to evaluate hook of hamate fractures.
- MRI
- Use to evaluate for ganglion cyst.
- A gradient echo MRI will also show an ulnar artery aneurysm.
- DOPPLER US OR ARTERIOGRAM
- Useful to diagnose ulnar artery thrombosis and aneurysm.
STUDIES :
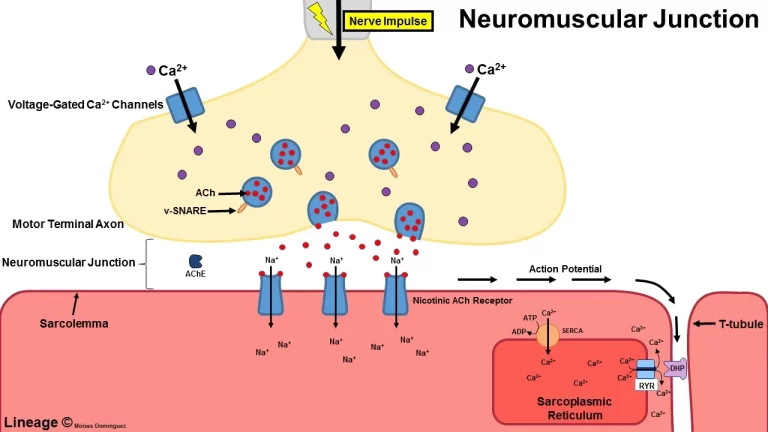
- EMG AND NCV
- Helpful to establishing diagnosis and prognosis
- Threshold for diagnosis
- conduction velocity, 50 m/ sec across the elbow
- low amplitudes of sensory nerve action potentials and compound muscle action potentials.
DIFFERENTIAL DIAGNOSIS :
CUBITAL TUNNEL SYNDROME
- Compared to ulnar tunnel syndrome, cubital tunnel demonstrates.
- Less clawing.
- Sensory deficit to dorsum of the hand.
- Motor deficit to ulnar-innervated extrinsic muscles.
- Tinel sign at the elbow.
- Positive elbow flexion test.
Treatment of Ulnar tunnel syndrome :
PHYSIOTHERAPY MANAGEMENT (NON-OPERATIVE MANAGEMENT) :
In patients with mild to moderate symptoms, conservative intervention is directed toward minimizing or eliminating the causative factor. Considerations include :
NERVE PROTECTION.
Initially, the wrist may have to be splinted to provide rest from the provoking activity. Splint the wrist in the neutral position, so there is minimal pressure in the tunnel.
MOBILITY TECHNIQUES:

- JOINT MOBILIZATION.
- If there is restricted joint mobility, mobilize the carpals for increased carpal tunnel space.
- TENDON – GLIDING EXERCISES.
- Teach the patient tendon – gliding exercise for mobility in the extrinsic tendons, they should be performed gently to prevent increased swelling.
- ULNAR NERVE MOBILIZATION.
- Move the wrist into extension and radial deviation, then apply over-pressure stretch into extension against the ring and little finger. Include forearm pronation and elbow flexion to move the nerve in a proximal direction.
- EXERCISES.
- Active finger and thumb flexion / extension, abduction/adduction, and thumb opposition.
- Active wrist flexion/extension.
- Active radial and ulnar deviation of the wrist ( with the splint removed and the wrist supported in slight extension ).
OPERATIVE MANAGEMENT :
If the patient’s symptoms do not improve with 6 to 12 weeks of conservative treatment, or if there is progressive paralysis ,long – standing muscle wasting, and clawing of the digits, surgical release of the ulnar tunnel is performed.
Local decompression:
Indications.
severe symptoms that have failed nonoperative treatment.
Tendon transfers:
Indications.
- correction of clawed fingers.
- loss of power pinch.
- Wartenberg sign (abduction of small finger).
Carpal tunnel release:
Indications.
patients diagnosed with both ulnar tunnel syndrome and CTS :
HOME CARE TO TREAT THE SYMPTOMS :
- You can do several things at home to manage the symptoms of ulnar tunnel syndrome. Try these tips:
- Adjust how you work or type.
- Use ergonomic and padded tools.
- Avoid activities that aggravate your symptoms.
- Avoid resting your elbow on furniture or armrests. This could put pressure on the nerve.
- Apply ice to the area.
- Wear a wrist brace or splint.
- Take OTC pain relievers or anti-inflammatory medications.
COMPLICATIONS:
- Without treatment or intervention, ulnar tunnel syndrome can continue to get worse. You may lose the ability to hold things with your hand. Simple tasks such as opening a jar or typing on a computer can become impossible.
- Over time, permanent damage to the ulnar nerve may develop. You may also have permanent numbness, weakness, pain, and tingling in your wrist or hand.
- However, there are several treatment options for ulnar tunnel syndrome. With proper treatment, you may be able to recover completely.




5 Comments