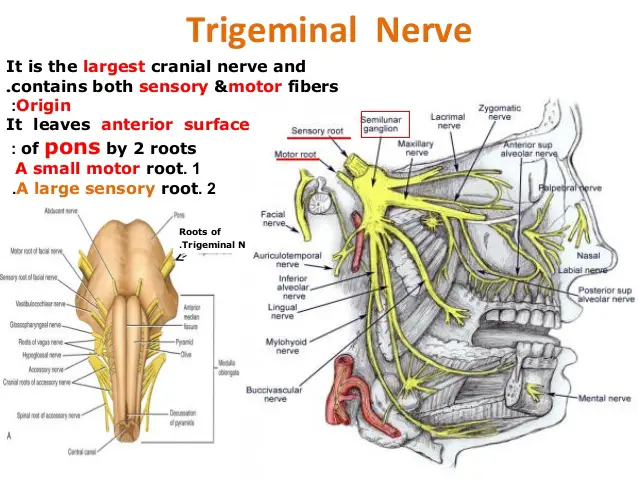
Trigeminal Nerve
Introduction
The trigeminal nerve (the fifth cranial nerve, or simply CN V) is a nerve responsible for sensation in the face and motor functions such as biting and chewing; it is the most complex of the cranial nerves.
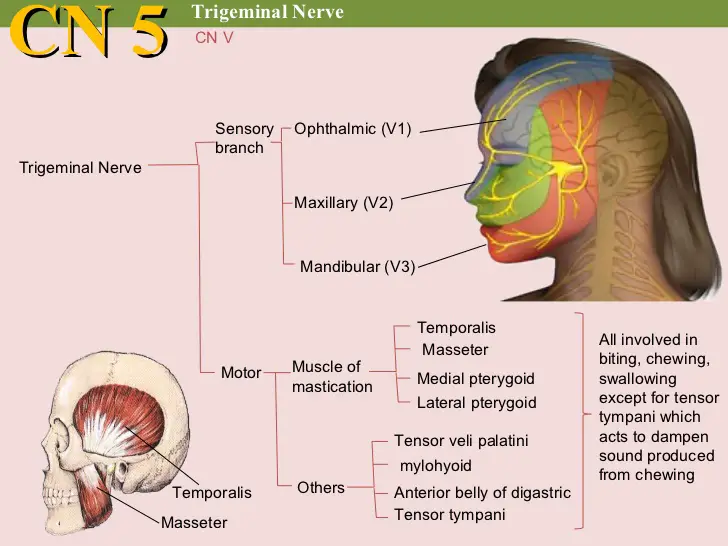
Its name (“trigeminal” = tri-, or three, and – geminus, or twin: thrice-twinned) derives from the fact that each of the two nerves (one on each side of the pons) has three major branches:
- Ophthalmic nerve (V1)
- Maxillary nerve (V2)
- Mandibular nerve (V3).
The ophthalmic and maxillary nerves are purely sensory, whereas the mandibular nerve supplies motor as well as sensory (or “cutaneous”) functions.
Adding to the complexity of this nerve is the fact that autonomic nerve fibers as well as special sensory fibers (taste) are contained within it.
The motor division of the trigeminal nerve derives from the basal plate of the embryonic pons, and the sensory division originates in the cranial neural crest.
Sensory information from the face and body is processed by parallel pathways in the central nervous system.
Anatomical Course
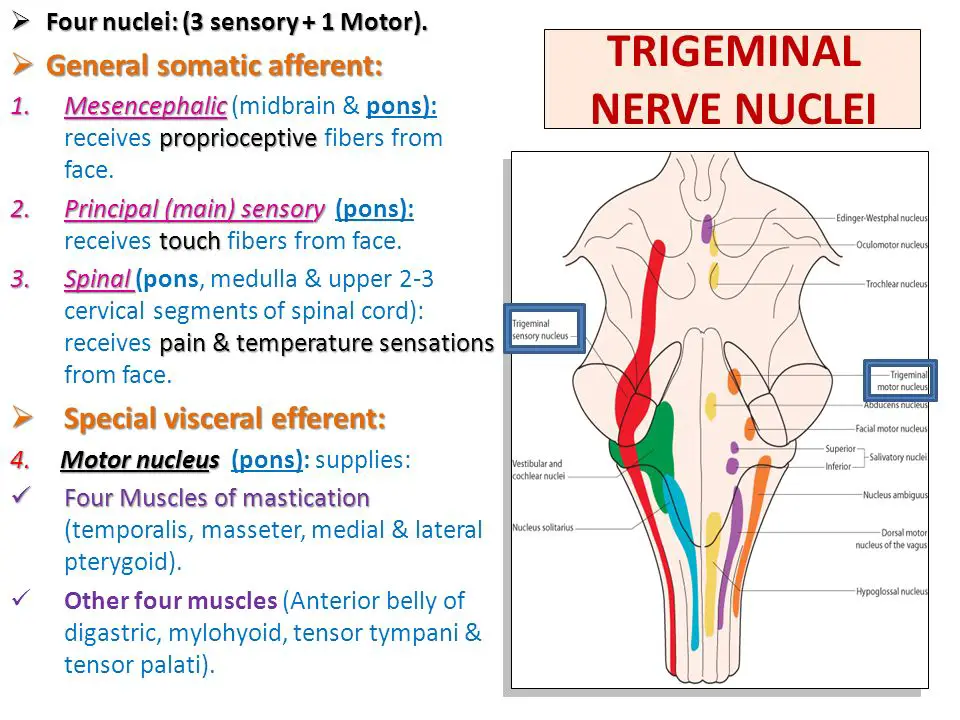
The trigeminal nerve originates from three sensory nuclei (mesencephalic, principal sensory, and spinal nuclei of the trigeminal nerve) and one motor nucleus (motor nucleus of the trigeminal nerve) extending from the midbrain to the medulla.
A nucleus (pl. nuclei) is a collection of neurone cell bodies within the central nervous system.
At the level of the pons, the sensory nuclei merge to form a sensory root. The motor nucleus continues to form a motor root. These roots are analogous to the dorsal and ventral roots of the spinal cord.
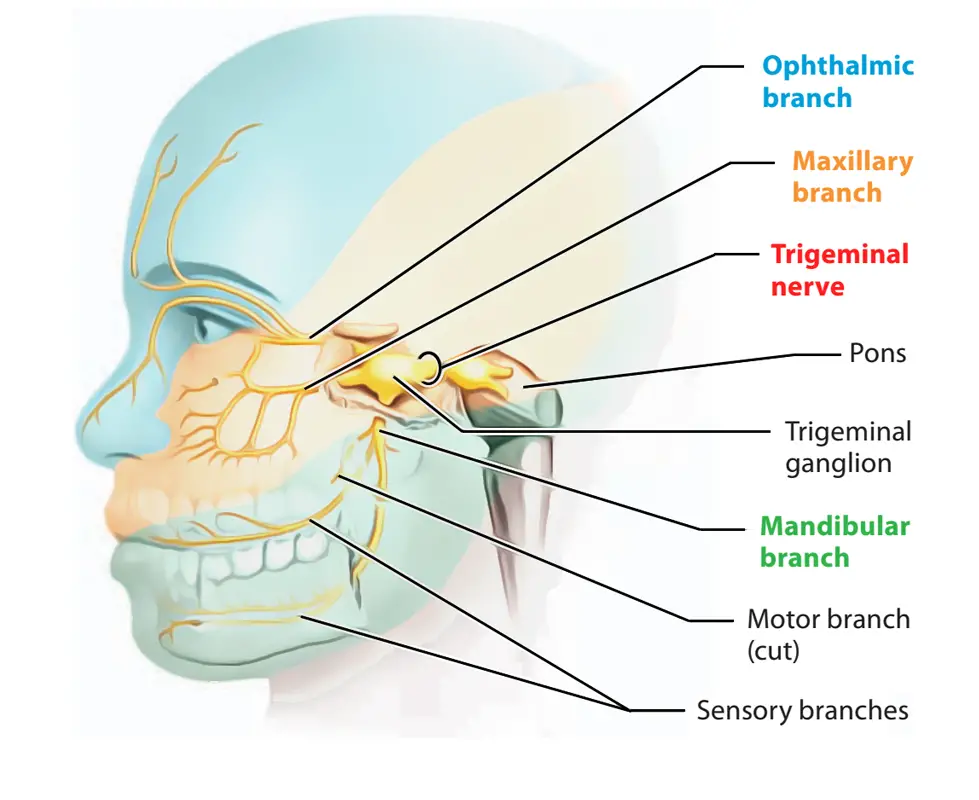
In the middle cranial fossa, the sensory root expands into the trigeminal ganglion. A ganglion (pl. ganglia) refers to a collection of neurone cell bodies outside the central nervous system.
The trigeminal ganglion is located lateral to the cavernous sinus, in a depression of the temporal bone. This depression is known as the trigeminal cave.
The peripheral aspect of the trigeminal ganglion gives rise to 3 divisions: ophthalmic (V1), maxillary (V2), and mandibular (V3).
The motor root passes inferiorly to the sensory root, along the floor of the trigeminal cave. Its fibres are only distributed to the mandibular division.
The ophthalmic nerve and maxillary nerve travel lateral to the cavernous sinus exiting the cranium via the superior orbital fissure and foramen rotundum respectively.
The mandibular nerve exits via the foramen ovale entering the infra-temporal fossa. (Note – be aware that while we talk about the nerves exiting the cranial cavity, the sensory components can also be said to be entering the cranial cavity, since they are afferent fibres).
Divisions of Trigeminal Nerve
Ophthalmic Nerve:
The ophthalmic nerve gives rise to 3 terminal branches: frontal, lacrimal, and nasociliary, which innervate the skin and mucous membrane of derivatives of the frontonasal prominence derivatives:
- Forehead and scalp
- Frontal and ethmoidal sinus
- Upper eyelid and its conjunctiva
- Cornea (see clinical relevance)
- Dorsum of the nose
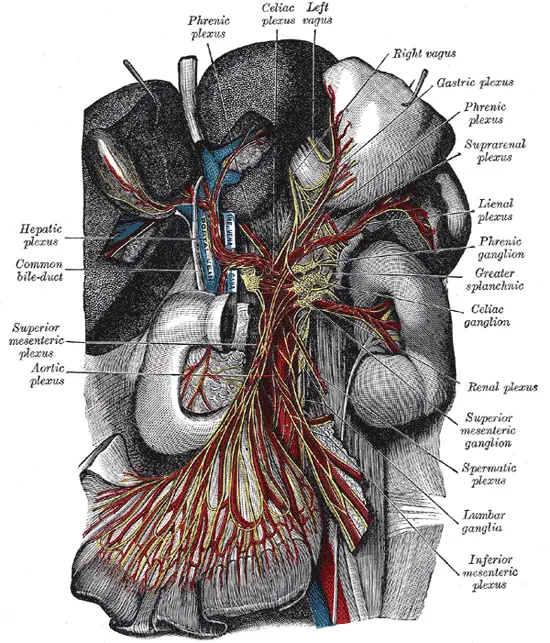
Parasympathetic Supply:
Lacrimal gland: Post-ganglionic fibres from the pterygopalatine ganglion (derived from the facial nerve), travel with the zygomatic branch of V2 and then join the lacrimal branch of V1. The fibres supply parasympathetic innervation to the lacrimal gland.
Maxillary Nerve:
The maxillary nerve gives rise to 14 terminal branches, which innervate the skin, mucous membranes, and sinuses of derivatives of the maxillary prominence of the 1st pharyngeal arch:
- Lower eyelid and its conjunctiva
- Cheeks and maxillary sinus
- Nasal cavity and lateral nose
- Upper lip
- Upper molar, incisor, and canine teeth and the associated gingiva
- Superior palate
Parasympathetic Supply:
Lacrimal gland: Post-ganglionic fibres from the pterygopalatine ganglion (derived from the facial nerve), travel with the zygomatic branch of V2 and then join the lacrimal branch of V1. The fibres supply parasympathetic innervation to the lacrimal gland.
Nasal glands: Parasympathetic fibres are also carried to the mucous glands of the nasal mucosa. Post-ganglionic fibres travel with the nasopalatine and greater palatine nerves (branches of V2)
Mandibular Nerve:
Mandibular nerve gives rise to four terminal branches in the infra-temporal fossa: buccal nerve, inferior alveolar nerve, auriculotemporal nerve and lingual nerve.
These branches innervate the skin, mucous membrane and striated muscle derivatives of the mandibular prominence of the 1st pharyngeal arch.
Sensory supply:
- Mucous membranes and floor of the oral cavity
- External ear
- Lower lip
- Chin
- Anterior 2/3 of the tongue (only general sensation; special taste sensation supplied by the chorda tympani, a branch of the facial nerve)
- Lower molar, incisor, and canine teeth and the associated gingiva
Motor Supply:
- Muscles of mastication: medial pterygoid, lateral pterygoid, masseter, temporalis
- Anterior belly of the digastric muscle and the mylohyoid muscle (these are suprahyoid muscles)
- Tensor veli palatini
- Tensor tympani
Parasympathetic Supply
Submandibular and Sublingual glands: Post-ganglionic fibres from the submandibular ganglion (derived from the facial nerve), travel with the lingual nerve to innervate these glands.
Parotid gland: Post-ganglionic fibres from the otic ganglion (derived from the glossopharyngeal nerve, CN IX), travel with the auriculotemporal branch of the V3 to innervate the parotid gland.
Brainstem Nuclei
The trigeminal nerve’s motor and sensory nuclei are located in the brainstem. The primary sensory nucleus, spinal trigeminal nucleus, and mesencephalic nucleus are the three sensory nuclei of the trigeminal nerve.
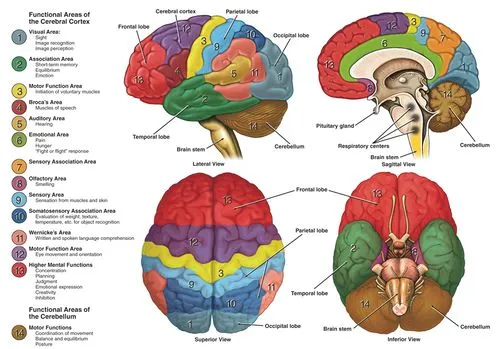
Principal Sensory Nucleus
Within the posterolateral surface of the pontine tegmentum, the primary sensory nucleus is situated lateral to the motor nucleus. The primary sensory nucleus is where fibers transmitting delicate touch and pressure synapse. From there, they rise in the trigeminal nerve, which decusses to the opposite side of the brainstem. Both the uncrossed dorsal trigeminothalamic tract and the trigeminal l end in the thalamus’s ventroposteromedial (VPM) nucleus, and they eventually form synapses in the somatosensory cortex on the ipsilateral side of each thalamus.
Spinal Trigeminal Nucleus
The spinal trigeminal nucleus, which descends from the lower pons to the upper cervical levels of the spinal cord (C2-4) and connects to the dorsal horn of the spinal cord, is a caudal extension of the primary sensory nucleus. The pars oralis, pars interpolaris, and pars caudalis are additional divisions of the spinal trigeminal nucleus that run from rostral to caudal. The pars interpolaris runs from the rostral third of the inferior olive to the obex, the pars caudalis from the obex to the upper cervical levels, and the pars oralis runs from the mid-pontine level to the rostral third of the inferior olive in the medulla oblongata. The primary function of the spinal trigeminal nucleus is to support the facial thermoceptive and nociceptive fibers.
Mesencephalic Nucleus
From the level of the superior colliculus in the upper midbrain to the middle pontine level, the mesencephalic nucleus is a cephalad extension of the primary sensory nucleus. Because it is the sole instance when primary sensory neurons are found inside the central nervous system rather than in a peripheral ganglion, the mesencephalic nucleus is special. Proprioceptive fibers from the hard palate, teeth, periodontium, temporomandibular joint capsule, Golgi tendon organs, and muscle spindles from the extraocular and masticatory muscles are received by the mesencephalic nucleus. The ipsilateral VPM of the thalamus, the motor trigeminal nucleus, and finally the ipsilateral somatosensory cortex are the primary destinations of the mesencephalic nucleus’s projections.
Motor Nucleus
The motor nucleus is situated on the lateral side of the pontine tegmentum, medial and anterior to the main trigeminal sensory nuclei.
CN V is divided into three branches, each of which has a unique innervation territory. The ocular (V1), maxillary (V2), and mandibular nerves (V3) are the names of these branches.
Trigeminal Ganglion
The trigeminal ganglion, also known as the Gasterion or semilunar ganglion, is reached by the three divisions of the trigeminal nerve and houses the cell bodies of the majority of the trigeminal sensory axons. Meckel’s cave, a CSF-filled void between two layers of dura mater covering the petrous section of the temporal bone, is home to the trigeminal ganglion. The three trigeminal nerve roots and the trigeminal ganglion are enclosed by Meckel’s cave. Two axonal branches, one reaching proximally to the brainstem and the other distally towards one of the trigeminal divisions, are characteristic of the pseudo-unipolar trigeminal neurons found in the trigeminal ganglion.
Consequently, trigeminal neurons are able to conduct action potentials in two directions: antidromically, towards branches of the trigeminal divisions, and orthodromically, into the brainstem, with pain and temperature.
Trigeminal Root
Sensory fibers that run from the trigeminal ganglion to the ventrolateral side of the pons are carried by the trigeminal root. The trigeminal root entry zone (TREZ) is thought to be the most susceptible location along the nerve for neurovascular compression. It is situated around 12 mm distal to the pons, where peripheral myelin replaces central myelin.
Clinical Relevance
Trigeminal Neuralgia
Sharp, electrical, shock-like, paroxysmal, lancinating pain in one or more trigeminal nerve branches is the hallmark of the clinical illness known as trigeminal neuralgia. The superior cerebellar artery compresses the trigeminal nerve at the root entrance zone in the majority of instances.
Additional causes of trigeminal neuralgia include tumors, arteriovenous malformations, compression from nearby aneurysmas, and intrinsic abnormalities such demyelinating plaques in multiple sclerosis. The combination of radiographic imaging and clinical presentation is used to make the diagnosis. MRI of the brain, with a focus on the cisterns, is commonly used for this type of imaging, and MRI sequences like Fast-Imaging-Employing-Steady-state-Acquisition (FIESTA) can help.
The underlying cause of trigeminal neuralgia determines how it should be treated. Carbamazepine is the first-line therapy; other second-line treatments include baclofen, lamotrigine, oxcarbazepine, phenytoin, gabapentin, and pregabalin.
If the patient experiences severe adverse effects from the medicines or if the pain grows unresponsive to treatment, surgery can be necessary.
Surgical Treatment of Trigeminal Neuralgia
A surgical intervention for trigeminal neuralgia is one of the most popular treatments involving the trigeminal nerve. There are two sorts of surgical procedures for trigeminal neuralgia: non-destructive and destructive. Through a process known as microvascular decompression, any structure that may be pressing on the nerve—typically the superior cerebellar artery—is removed in an attempt to relieve nerve compression.
Percutaneous rhizotomy and stereotactic radiosurgery are examples of destructive techniques that totally damage the trigeminal nerve to stop it from transmitting pain. Within the ablated nerve distribution, a damaging operation causes the affected side of the face to lose feeling permanently.
Cluster Headache
Trigeminal neuralgia presents similarly to cluster headaches. Cluster headaches often manifest as a severe headache on one side of the head that affects the trigeminal nerve region and occurs at short intervals, frequently several times in a single day. Autonomic symptoms including nasal congestion, puffiness, and lacrimation on the afflicted side may accompany these headaches. Although the exact etiology of cluster headaches is yet unknown, the beginning of symptoms is frequently brought on by an outside stimulation. Typically, preventive care consists of both medication and trigger avoidance. Acute episodes can be treated with oxygen and fast-acting triptans.
Lateral Medullary Syndrome (Wallenberg Syndrome)
A stroke of the posterior inferior cerebellar artery or vertebral artery usually causes damage to the lateral part of the medulla in the brainstem, resulting in the clinical state known as lateral medullary syndrome. In addition to other indications and symptoms including vertigo, ataxia, horner syndrome, dysphagia, and hoarseness, a lesion in this area of the brain stem causes an ipsilateral sensory loss in the trigeminal nerve’s domain and contralateral sensory loss in the rest of the body.
Jaw-Jerk Monosynaptic Reflex
When the masseter muscle is suddenly stretched, the jaw jerk reflex causes the jaw to close. Afferent impulses from the masticatory muscle spindles, which project onto the trigeminal motor nucleus, are received by the trigeminal mesencephalic nucleus. The motor trigeminal nucleus sends efferent output via V3 to the masticatory muscles.
Corneal Reflex:
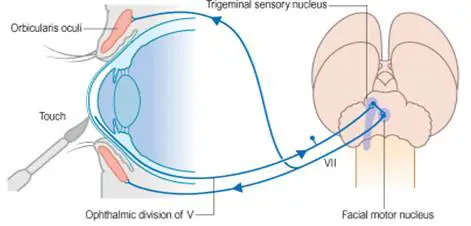
- The corneal reflex is the involuntary blinking of the eyelids – stimulated by tactile, thermal, or painful stimulation of the cornea.
- In the corneal reflex, the ophthalmic nerve acts as the afferent limb – detecting the stimuli. The facial nerve is the efferent limb, causing contraction of the orbicularis oculi muscle.
- If the corneal reflex is absent, it is a sign of damage to the trigeminal/ophthalmic nerve, or the facial nerve.
Inferior Alveolar Nerve Block:
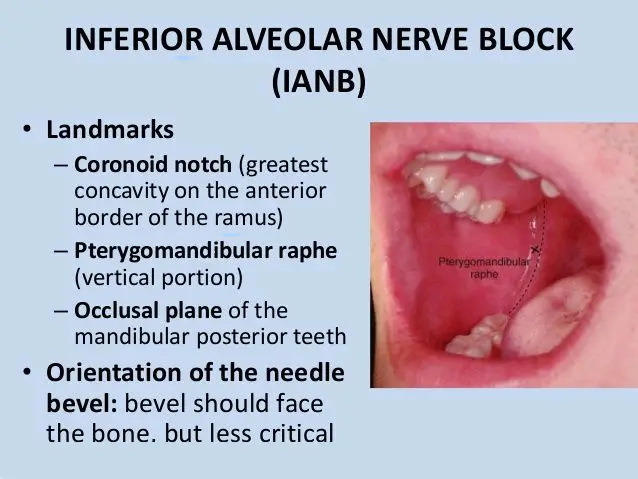
- The inferior alveolar nerve, a branch of V3, travels through the mandibular foramen and mandibular canal. Within the mandibular canal, the inferior alveolar nerve forms the inferior dental plexus, which innervates the lower teeth.
- A major branch of this plexus, the mental nerve, supplies the skin and mucous membranes of the lower lip, the skin of the chin, and the gingiva of the lower teeth.
- In some dental procedures which require local anaesthesia, the inferior alveolar nerve is blocked before it gives rise to the plexus.
- The anaesthetic solution is administered at the mandibular foramen, causing numbness of the area supplied by the inferior alveolar nerve.
- The anaesthetic fluid also spreads to the lingual nerve which originates near the inferior alveolar nerve, causing numbness of the anterior 2/3 of the tongue.
Examination of the Trigeminal Nerve
Testing sensory supply: ask the patient to close their eyes and introduce a cotton wisp to areas of the face supplied by the three divisions of the trigeminal nerve to detect tactile sensory competence.
Testing motor supply: ask the patient to clench their jaw as you palpate superior to the zygomatic arch to feel for contraction of the temporalis and then repeat palpating inferiorly for the masseter.
Ask the patient to open their mouth and deviate their mandible to the right and left to check for competence of the medial and lateral pterygoid muscles.
Test for corneal reflex – note this requires a competent ophthalmic branch and temporal and zygomatic branches of the facial nerve.
FAQ
What happens if trigeminal nerve is damaged?
In addition to causing severe neurosensory deficits and face pain, trigeminal nerve injuries can result in substantial comorbidities such as altered oral mucosa feeling or changes in eating habits caused by masticator muscle denervation.
What is the spinal trigeminal nerve?
Along with the principal sensory nucleus, the spinal nucleus of the trigeminal nerve is sometimes referred to as the trigeminal sensory nuclear complex (TSNC). It is a longitudinally shaped nucleus located in the caudal pons and medulla that receives sensory afferents related to pain and temperature from the orofacial region supplied by the trigeminal nerve.
Can trigeminal nerve repair itself?
Damage to the trigeminal nerve can vary from mild discomfort to total nerve amputation. There are two categories for injuries: recoverable (meaning they may recover on their own) and non-recoverable (meaning they cannot).
How do you test for trigeminal nerve?
Request that the patient tighten their jaw. Check the masseter and temporal muscles for tone and volume asymmetry. As the jaws open, look for any deviation in the mandibular tip. If there is weakness in the seventh nerve, align a tongue blade with the tip of the nose and the middle of the mouth.
What is the function of the trigeminal nerve?
The portion of the neurological system that transmits touch, temperature, and pain signals from your face to your brain is called the trigeminal nerve. Your head’s huge, three-part nerve is what gives you feeling. The mandibular nerve is one area that controls motor function, which aids in chewing and swallowing.
What part of brain is trigeminal nerve?
The trigeminal nerve originates as a larger sensory root (portio major) and a smaller motor root (portio minor) on the anterolateral surface of the mid-pons.
What is a trigeminal headache?
A localized peripheral neuropathy called trigeminal neuralgia is brought on by irritation of the trigeminal nerve, which is the fifth cranial nerve. Severe, sporadic facial pain, usually affecting one side of the face, is its defining feature. The pain is of the usual throbbing kind.
References
Huff, T. (2022, November 9). Neuroanatomy, Cranial Nerve 5 (Trigeminal). StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482283/


7 Comments