Sciatic Nerve: Overview
Anatomy and Physiology Of Sciatic Nerve
Origin and Branches of the Sciatic Nerve:
The sciatic nerve starts in the lower spine and follows a long path through the buttock, down the back of the thigh and leg, and finally ends in the foot.
Origin of Sciatic Nerve :
The sciatic nerve is formed by the combination of 5 nerves in the lumbar (lower) and sacral spine—L4, L5, S1, S2, and S3. These nerve fibers are typically responsible for motor and sensory functions of the lower body. The 5 nerves group together near the front surface of the piriformis muscle deep in the buttock and form the large, thick sciatic nerve. At its thickest portion, the nerve measures around 2 cm in diameter.2,3
The nerve leaves the pelvis along with its surrounding nerves and blood vessels through the greater sciatic foramen below the piriformis muscle. It progresses downward between the muscles of the thigh and is surrounded by a single long fatty sheath from the pelvis to the knee, where it divides. In around 10% of the population, the nerve may divide above the knee.
Branches of Sciatic Nerve
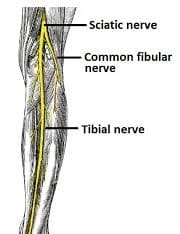
At the popliteal fossa near the back of the knee, the sciatic nerve divides into 2 main branches: the tibial nerve and the common peroneal nerve. The popliteal fossa is a rhomboid-shaped space that serves as a conduit for blood vessels and nerves in the leg.
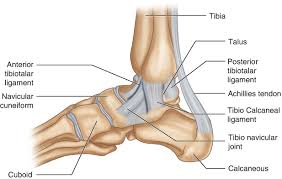
The tibial nerve continues down the back of the leg to the heel and sole of the foot.
The common peroneal travels sideways along the outer part of the knee to the outer border of the leg and foot.
Both these nerves finally terminate into sural nerves.
Illustration of the Sciatica Nerve variants :
This nerve is usually undivided and leaves the pelvis through the greater sciatic foramen below the piriformis muscle (left). Sometimes, the nerve may be divided, with one part passing through the piriformis and the other below the muscle (right).
Anatomic Variants of the Sciatic Nerve
It is estimated that around 16% of the population may have variations in the anatomical structure of the sciatic nerve.1,4
These variations include :
The sciatic nerve divides above the piriformis muscle; one portion passes through the piriformis, and the other leaves the pelvis below the muscle. This variant is the most common among others.
This nerve divides above the piriformis muscle; one portion passes through the piriformis, and the other leaves the pelvic area above the muscle.
The sciatic nerve divides above the piriformis, one portion travels in front of it, and the other travels behind it.
An undivided sciatic nerve exits through the piriformis muscle.
An undivided sciatic nerve exits from behind the top part of the piriformis.
In cases where the sciatic nerve divides, both portions of the nerve immediately merge again and course downward as a single nerve.
While the variants are considered normal, these individuals may be at a higher risk of developing sciatica pain due to impingement, entrapment, or irritation of the nerve.
Motor functions of the sciatic nerve
The motor functions include:
- Knee flexion: Bending the knee
- Hip adduction: Bringing the thighs together/movement of the leg toward the midline of the body
- Plantar flexion: Pointing the foot downward
- Flexion of toes: Pointing the toes downward
- Dorsiflexion of the foot: Pointing the foot upward
- Extension of toes: Pointing the toes upward
- When the sciatic nerve is compressed, it is common to experience reduced motor functions and weakness in the affected leg.
Sensory functions:
This nerve provides sensations to the skin (dermatome) over the following areas:
- Front, back, and outer part of the thigh
- Front, back, and outer part of the lower leg
- The top and outer sides of the foot
- Sole of foot
- The web between the first and second toes
- Sensory symptoms such as burning, tingling, and/or numbness may be experienced when the sciatic nerve is inflamed or irritated.
Innervation of Sciatic Nerve:
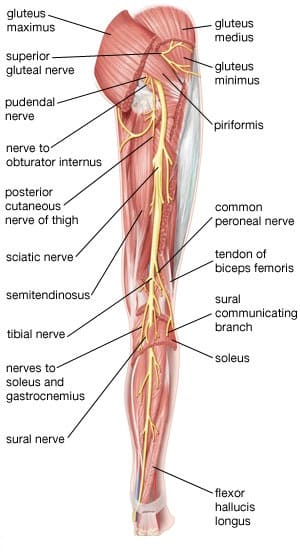
Tibial division
motor
- semitendinous
- semimembranous
- long head biceps femoris
- gastrocnemius
- popliteus
- plantaris
- soleus
- tibialis posterior
- flexor digitorum longus
- flexor hallucis longus
- sensory innervation
- none
- Peroneal division
- motor
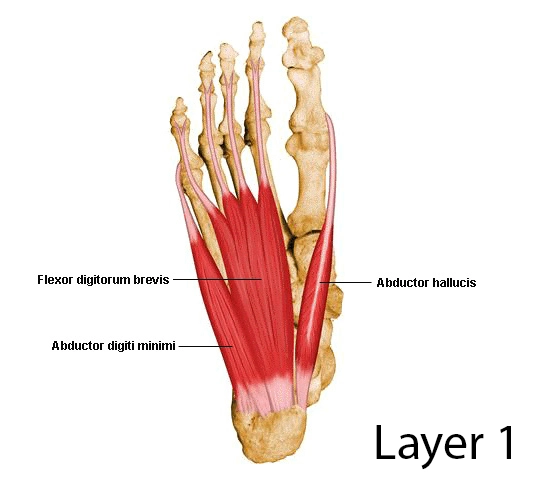
- abductor hallucis
- flexor digitorum brevis
- flexor hallucis brevis
- foot lumbricals
- quadratus plantae
- flexor digiti minimi
- adductor hallucis
- foot interossei
- abductor digiti minimi
- sensory
- articular branch to the knee joint
- sural nerve branch
- runs distal with the small saphenous vein
- anastomoses with a branch from the peroneal nerve
- continues distal on the lateral aspect of the Achilles tendon
- terminates as the lateral dorsal cutaneous nerve of the foot
- common peroneal nerve
motor
- short head of biceps femoris
- deep peroneal nerve
leg
- tibialis anterior
- extensor digitorum longus
- peroneus tertius
- extensor hallucis longus
foot
- extensor digitorum brevis (lateral terminal branch)
- extensor hallucis brevis (lateral terminal branch)
sensory
- articular branch to the ankle joint
- medial terminal branch: 1st dorsal webspace
- superficial peroneal nerve
motor
- lateral compartment of the leg
- peroneus longus
- peroneus brevis
sensory
- majority of the skin on the dorsum of the foot, excluding the webspace between the hallux and second digit (deep peroneal nerve)
- anterolateral distal 1/3 of leg
Origin
- The nerve originates from lumbosacral plexus L4-S3
- tibial division
- originates from anterior preaxial branches of L4,L5,S1,S2,S3
- peroneal division
- originates from from postaxial branches of L4,L5,S1,S2
Course
- Exits sciatic notch
- runs anterior or deep to piriformis
- runs posterior or superficial to short external rotators (superior gemellus, inferior gemellus, obturator internus)
Posterior leg
- It then runs down the posterior leg where it breaks into its three main divisions at the level of the mid-thigh
Terminal branches
- common peroneal nerve
- tibial nerve
Blood Supply and Lymphatic Drainage
The extrinsic and intrinsic systems supply the blood to peripheral nerves, such as the sciatic nerve and its branches. The extrinsic system is supported by the vasa nervorum, a collection of nearby arteries and veins.
The arteries and veins that run longitudinally, just deep to the epineurium, make up the intrinsic vasculature of the sciatic nerve. There are several connection locations where this vascular joins the extrinsic vasculature. The vasculature of the nerve has several collateral networks and extremely variable flow. The tibial section of the sciatic nerve has a better blood supply than the fibular branches when comparing the branches.
Location of the sciatic nerve
The sciatic nerve is a mixed nerve, meaning it contains both motor and sensory fibers, and it runs from the lower back to the foot. In the lower limbs, these fibers give function to motor and sensation.
Embryology
After the 3rd week following fertilization, a process called neurulation takes place. The neural plate is formed as a layer of cells covering the ectoderm thickens. The neural tube and neural crest cells are derived from the neural plate. The neurons in the peripheral nervous system, which includes the sciatic nerve, are descended from neural crest cells. Furthermore, neural crest cells give rise to Schwann cells, which myelinate the peripheral nervous system.
Sciatic Nerve Assessment
Straight leg raise Test
One type of neurodynamic exam is the Straight Leg Raise exam (SLR). Neurodynamic examinations assess the neurological tissues’ mechanical motion and their susceptibility to mechanical strain or compression. Regardless of the severity of disc damage, some believe that these tests, coupled with a related medical history and a reduced range of motion, are the most significant physical indicators of disc herniation injury.
Slump Test
In this test, the sciatic nerve is stretched by extending the knees, bending the hips, and stretching the spine. In order to create a neutral spine, have the patient sit with their hands behind their back to start the exam. The patient should initially hunch forward at the lumbar and thoracic spines. If the patient is not in discomfort in this posture, have them bend their neck by resting their chin on their chest and then extending one knee as far as they can.
Ask the patient to extend their neck into neutral if extending their knee gives them any pain. The test is counted as positive if the patient is still in pain and unable to extend the knee.
Ask the patient to aggressively dorsiflex their ankle if extending their knee does not give them any pain. Have the patient bend their knee slightly while continuing dorsiflexing if dorsiflexion is painful. The test is counted as positive if the pain is reproduced.
The test is then conducted again on the other side.
Clinical Significance of Sciatic Nerve
Sciatica
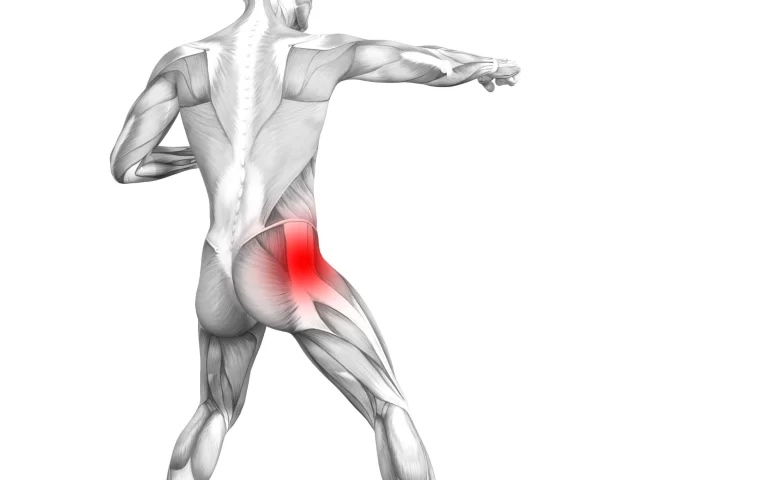
- Sciatica is defined as irritation or compression of the sciatic nerve that causes pain in the buttock area with radiation to the lower leg. The vast majority of cases have a spinal cause, such as disc herniation or rupture causing impingement of L5 or S1 nerve roots.
- Other common causes include spinal stenosis, degenerative disc disease, and lumbar spondylolisthesis. There are also many non-spinal causes of sciatica, which are less common. These include piriformis syndrome, trauma, post-operative complications, gynecologic conditions, and herpes zoster.
- Symptoms include mid-buttock pain that radiates down the leg, most often unilaterally. The patient will often experience paresthesias in a dermatomal distribution, either L5 or S1 depending on where the sciatic nerve is being irritated. Weakness and changes in reflexes are less commonly seen.
- One test that should always be done in patients with low back pain is straight leg raising with the patient supine. The test is positive if there is ipsilateral pain between 10 to 60 degrees. This test is quite sensitive (90%), but not specific. If this test elicits pain in the contralateral leg, one should suspect disc herniation and order an imaging test. MRI is very useful when the exact level of compression in the spine is unclear.
- MRI can also assess the soft tissues or the presence of an infection or a neoplastic cause. If there is urine retention or dysesthesia around the anus in a patient with sciatica, one should suspect cauda equina syndrome. Prompt surgical decompression is indicated for this disorder.
- The majority of cases of sciatica are treated conservatively with rest for a few days, pain medication, and some physical therapy. Surgery may be required in cases where there is significant stenosis, or there is evidence of irritation of the nerve.
Intramuscular injections
Intramuscular injections frequently take place in the buttocks. The conventional opinion holds that an injection into the inferomedial buttock puts the sciatic nerve in danger, whereas the superolateral buttock is safe. The fact that many persons have a fatty elevation on the inferomedial buttock complicates this idea. Using the “upper and outer” quadrant as a reference puts the sciatic risk at risk of injury. Sciatic neuropathy may result from sciatic nerve injection. Pediatric patients have been reported to have sciatic nerve MRIs. Adults frequently utilize it.
Alpha-motor neurons in the ventral horns of rats exhibit inflammatory responses in response to injuries in the L4 and L5 segments that make up the sciatic nerve. The first three days following damage cause a significant upregulation of the NLRP3 inflammasome in the motor neurons. The regeneration of the sciatic nerve is significantly delayed by this inflammatory response. Extracellular ATP has a significant role in regulating the pro-inflammatory process that raises microgliosis and prevents these motor neurons from regenerating.



Great article.!! Can you tell me if problems with the sciatic nerve can cause skin irritations. Both of my legs have been affected the same way and I must put eucerin on each leg (thigh to bottom of my feet) to prevent itching and/or irritation. The bottom of my feet seem to be kind of numb.
Yes, it can affect skin irritation seen sometimes, numbness is common in sciatica, consultation and treatment is required urgently so please don’t late in your treatment.
i think you should contact nearby Doctor for the proper diagnosis and accordingly treatment. Early treatment surely help to relive your left foot pain and other related issue!