Recurrent Shoulder Dislocation And Physiotherapy Management
Recurrent shoulder dislocation definition
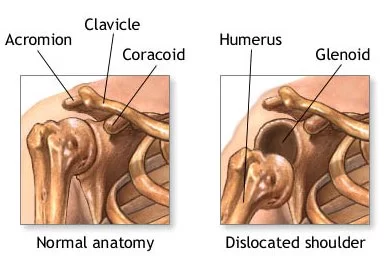
Recurrent shoulder dislocation is a disorder that occurs when the glenohumeral joint, or shoulder joint, is repeatedly dislocating. The shoulder is one of the most mobile joints in the human body, and as such is the most likely to dislocate.
Shoulder dislocation can be either anterior or posterior, with the anterior being more common. Shoulder dislocation can be caused by a traumatic event such as falling onto an outstretched arm, but can also be caused by repeated stress on the joint due to certain sports or activities. The most common symptom of shoulder dislocation is pain, which may occur suddenly or gradually depending on whether it was traumatic or chronic.
A dislocated shoulder is when the head of the humerus is out of the shoulder joint. The shoulder is one of the most mobile and the least stable of all the joints in the body. This makes it the joint which is most vulnerable to dislocations or subluxation. In a proportion of these patients, the shoulder tends to dislocate or sub-luxate repeatedly after the first dislocation. Patients with a tendency for recurrent (repeated) dislocation or subluxation are said to have an unstable shoulder or shoulder instability.
What causes Recurrent Shoulder Dislocation?
The cause of recurrent shoulder dislocation is not fully understood and there are many factors that could contribute to its development. There are many other causes of recurrent shoulder dislocations, but the most common cause is having surgery on that same shoulder after it has been previously injured.
Recurrent shoulder dislocation may have traumatic or atraumatic causes. There is a high recurrence rate after a primary shoulder dislocation, which is greatest in individuals < 20 years old
There are three main common causes that a shoulder can become unstable:
Earlier History of Shoulder Dislocation
Severe injury or trauma is often the cause of an initial shoulder dislocation. When the head of the humerus dislocates, the socket bone (glenoid) and the ligaments in the front of the shoulder are often injured.
The labrum — the cartilage rim around the edge of the glenoid — may also tear. This is commonly called a Bankart lesion.
A severe first dislocation can lead to continued dislocations, giving out, or a feeling of instability.
Repetitive Strain
Some people with recurrent shoulder instability have never had a dislocation. Most of these patients have looser ligaments in their shoulders.
This increased looseness is sometimes just their normal anatomy. Sometimes, it is the result of repetitive overhead motion.
Swimming, tennis, and volleyball are among the sports that require repetitive overhead motion and that can stretch out the shoulder ligaments. Many jobs also require repetitive overhead work.
Looser ligaments can make it hard to maintain shoulder stability. Repetitive or stressful activities can challenge a weakened shoulder. This can result in a painful, unstable shoulder.
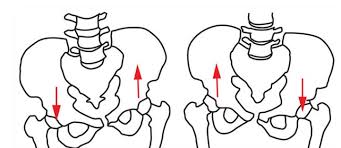
Multi-directional Instability
In a small minority of patients, the shoulder can become unstable without a history of injury or repetitive strain.
In such patients, the shoulder may feel loose or dislocated in multiple directions, meaning the ball may dislocate out the front, out the back, or out the bottom of the shoulder. This is called multidirectional instability.
These patients have naturally loose ligaments throughout the body and may be “double-jointed.”
Signs and symptoms:
Significant pain is sometimes felt along the arm past the shoulder.
A sensation that the shoulder is slipping out of the joint during abduction and external rotation.
Shoulder and arm held in external rotation (anterior dislocation), or adduction and internal rotation (posterior dislocation). Resistance of all movement.
Numbness of the arm.
Visibly displaced shoulder. Some dislocations result in the shoulder appearing unusually square.
No palpable bone on the side of the shoulder.
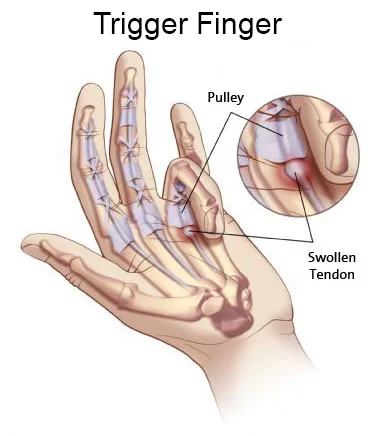
Complications may include a Bankart lesion, Hill-Sachs lesion, rotator cuff tear, or injury to the axillary nerve.
A shoulder dislocation often occurs as a result of a fall onto an outstretched arm or onto the shoulder.
They are classified as anterior, posterior, inferior, and superior with most being anterior. Males are affected more often than females.
How To Diagnosis is done in Shoulder Dislocation (Recurrent)?
Diagnosis is typically based on symptoms and confirmed by X-rays.
A diagnosis of shoulder dislocation is often suspected based on patient history and physical examination. Radiographs are made to confirm the diagnosis. Most dislocations are apparent on radiographs showing incongruence of the glenohumeral joint. Posterior dislocations may be hard to detect on standard AP radiographs but are more readily detected on other views. After reduction, radiographs are usually repeated to confirm successful reduction and to detect bony damage. After repeated shoulder dislocations, an MRI scan may be used to assess soft tissue damage. In regards to recurrent dislocations, the apprehension test (anterior instability) and sulcus sign (inferior instability) are useful methods for determining predisposition to future dislocation.
Shoulder dislocation is classified on the basis of the direction in which the ball dislocates in relation to the socket. It is termed unidirectional if it dislocates in one direction only, or multidirectional if it dislocates in more than one direction. Thus there are the following types of dislocation:
1) Unidirectional – These are usually traumatic in nature
a.Anterior – the ball dislocates in front of the socket. This is the commonest type.
b.Posterior – the ball dislocates behind the socket
c. Inferior – the ball dislocates below the socket
2) Multidirectional – These are usually traumatic in nature and occur in patients who have inborn laxity in their joints.
There are three main types of dislocations: anterior, posterior, and inferior.

Types of Shoulder Dislocation :
There are 3 main types of Shoulder dislocation :
- Anterior Dislocation
- Posterior Dislocation
- Inferior Dislocation
Anterior (forward) Dislocation of Shoulder Joint :
In over 95% of shoulder joint dislocations, the humerus is displaced anteriorly. In most of those, the head of the humerus comes to rest under the coracoid process, referred to as a sub-coracoid dislocation. Sub-glenoid, subclavicular, and, very rarely, intrathoracic or retroperitoneal dislocations may also occur.
Anterior dislocations are usually caused by a direct blow to, or fall on, an outstretched arm. The patient typically holds his/her arm externally rotated and slightly abducted.
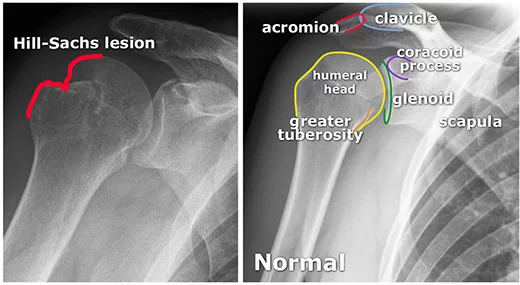
A Hill-Sachs deformity is an impaction of the head of the humerus left by the glenoid rim during dislocation.
Damage to the axillary artery and axillary nerve (C5, C6) may result. The axillary nerve is injured in 37% making it the most commonly injured structure with this type of injury. Other common, associated, nerve injuries include injury to the suprascapular nerve (29%) and the radial nerve (22%). Axillary nerve damage results in a weakened or paralyzed deltoid muscle and as the deltoid atrophies unilaterally, the normal rounded contour of the shoulder is lost. A patient with an injury to the axillary nerve will have difficulty in abducting the arm from approximately 15° away from the body. The supraspinatus muscle initiates abduction from a fully adducted position.
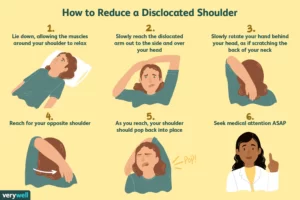
Treatment is by shoulder reduction which may be accomplished by a number of techniques including traction-counter traction, external rotation, scapular manipulation, and the Stimson technique. After reduction X-rays are recommended for verification. The arm may then be placed in a sling for a few weeks. Surgery may be recommended for those with recurrent dislocations.
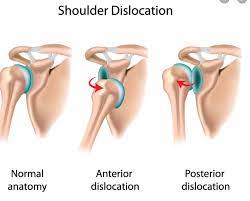
Posterior (backward) Dislocation of shoulder :
Lightbulb sign indicative of posterior shoulder dislocation is shown on the left. On the right, the same shoulder after reduction.
Posterior dislocations are uncommon and are typically due to muscle contraction from electric shock or seizure. They may be caused by a strength imbalance of the rotator cuff muscles. Patients typically present holding their arm internally rotated and adducted, and exhibiting flattening of the anterior shoulder with a prominent coracoid process.
Posterior dislocations may go unrecognized, especially in an elderly patient and in the unconscious trauma patient. An average interval of 1 year was noted between injury and diagnosis in a series of 40 patients.
Inferior (downward) Shoulder Dislocation :
An inferior dislocation of the shoulder after an automobile accident. Note how the humerus is abducted. Also present is a fracture of the greater tuberosity.
Inferior dislocation is the least likely, occurring in less than 1%. This condition is also called luxation erect because the arm appears to be permanently held upward or behind the head. It is caused by a hyper abduction of the arm that forces the humeral head against the acromion. Such injuries have a high complication rate as many vascular, neurological, tendon, and ligament injuries are likely to occur from this mechanism of injury.
Treatment of recurrent shoulder dislocation :
Prompt medical treatment should be sought for suspected dislocation. Usually, the shoulder is kept in its current position by use of a splint or sling. A pillow between the arm and torso may provide support and increase comfort. Strong analgesics are needed to allay the pain of dislocation and the distress associated with it.
Reduction Of Shoulder Dislocation Joint :
specifically the Cunningham technique
Shoulder reduction may be accomplished with a number of techniques including traction-countertraction, external rotation, scapular manipulation, Stimson technique, Cunningham technique, or Milch technique. Pain can be managed during the procedures either by procedural sedation and analgesia or injected lidocaine into the shoulder joint. Injecting lidocaine into the joint may be less expensive and faster. If a shoulder cannot be relocated in the emergency room, relocation in the operating room maybe required. This situation occurs in about 7% of cases.
Post-reduction treatment :
There does not appear to be any difference in outcomes when the arm is immobilized in internal versus external rotation following an anterior shoulder dislocation. A 2008 study of 300 people for almost six years found that conventional shoulder immobilization in a sling offered no benefit.
MRI of the shoulder after dislocation with Hill-Sachs lesion and labral Bankart’s lesion.
In young adults engaged in highly demanding activities shoulder surgery may be considered. Arthroscopic surgery techniques may be used to repair the glenoidal labrum, capsular ligaments, biceps long head anchor, or SLAP lesion or to tighten the shoulder capsule.
Arthroscopic stabilization surgery has evolved from the Bankart repair, a time-honored surgical treatment for recurrent anterior instability of the shoulder. However, the failure rate following Bankart repair has been shown to increase markedly in patients with significant bone loss from the glenoid (socket). In such cases, improved results have been reported with some form of bone augmentation of the glenoid such as the Latarjet operation.
Although posterior dislocation is much less common, instability following it is no less challenging, and, again, some form of bone augmentation may be required to control instability.
There remain those situations characterized by multi-directional instability, which have failed to respond satisfactorily to rehabilitation, falling under the AMBRI classification previously noted. This is usually due to an overstretched and redundant capsule that no longer offers stability or support. Traditionally, this has responded well to a ‘reefing’ procedure known as inferior capsular shift.
Recurrent shoulder dislocation surgery:
In cases where non-surgical treatment does not give result in recurrent shoulder dislocation, surgery may be needed to fix the problem.
More recently, the procedure has been carried out as an arthroscopic procedure, rather than open surgery, again with comparable results. Most recently, the procedure has been carried out using radio frequency technology to shrink the redundant shoulder capsule, although the long-term results of this development are currently unproven.
Open surgery and arthroscopic surgical procedures are treatment options in patients with traumatic recurrent anterior instability of the shoulder when conservative treatment fails to recover.
The arthroscopic surgery of glenohumeral instability requires that a level of expertise be achieved and retained. Although open stabilization was reported as more effective than arthroscopic stabilization in the aspect of post-operative recurrence rates in 1990s, clinical outcomes have become similar over time.
Technological improvements in arthroscopic surgery as well as the development of innovative surgical techniques as a result of the cumulative experience with an improved understanding of the factors leading to failure in such patients have played a key role.
In their prospective randomized study, Fabbriciani et al (surgeon) reported equal results between arthroscopic and open surgical repair of Bankart lesion in the aspect of recurrence shoulder dislocation.
According to the results of another recent prospective randomized clinical trial comparing open and arthroscopic techniques, the difference in quality of life between the patients in the two groups was neither significant nor clinically important at two years follow-ups; however, significantly lower risk of recurrence was obtained in patients for whom open repair was preferred.
The surgical treatment of athletes participating in sports person is still controversial.
Post-operative Treatment course after surgery:
The patient may leave the hospital on the same day or the next day in case of an arthroscopic repair, and after 2-3 days after open surgery. The arm is placed in a shoulder immobilizer type of sling which restricts movement of the arm upwards, outwards, and outward rotation of the arm. Depending upon the type of surgery performed and the strength of the repair achieved, the arm will be immobilized in the sling for a period of 3- 6 weeks. At around 2-3 weeks after surgery, pendulum exercises (gravity-assisted movements of the arm) are initiated. At around 6 weeks after surgery, full range-of-motion exercises as well as shoulder strengthening exercises are started.
Shoulder Muscle Strengthening Exercises
Strengthening exercises which may form part of a dislocated shoulder rehabilitation program.
A strengthening program for an anterior dislocated shoulder can begin as soon as pain allows. It is important for the athlete to avoid any movements which abduct and laterally rotate the shoulder in the early stages as this is the position in the shoulder that is most likely to dislocate again. Initially, static exercises involving no movement should be done and progressed gradually.
Isometric shoulder exercises
Isometric means without movement, also known as static contractions. These are exercises where the muscles are being worked without moving the joint and are often quite useful if the joint itself is still healing.
Isometric extension – Standing with your back against a wall, with your arms by your side. While keeping your elbows and wrists straight, push back into the wall and hold for 5 seconds. Work to increase this to 10 seconds. Repeat this 5 times.
To do the same for isometric flexion face the wall and use it as resistance in the same way as for extension exercises.
Isometric adduction – With a small pillow or a rolled-up newspaper between your injured arm and your torso, squeeze inwards and try to hold it in position. Start with a small item and gradually move to larger sizes to work through a larger range of movements. Hold for 5 seconds (work to increase to 10). Repeat this 5 times (work to increase to 10).
Isometric Abduction – Stand side-on to a wall, with the arm to be worked next to it. Place the back of the wrist against the wall and push outwards as if trying to raise the arm to the side. Hold for 5 seconds (work to increase to 10). Repeat this 5 times (work to increase to 10).
External Rotation – Stand facing a door frame. Keep the elbow bent to 90 degrees and place the back of the hand against the frame. Push against it. Hold for 5 seconds (work to increase to 10) and repeat 5 times (work to increase to 10).
Internal Rotation – Stand facing a door frame. Bend the elbow to 90 degrees, and place the palm of the hand on the side of the door frame and push against it. Hold for 5 seconds (work to increase to 10) and repeat 5 times (work to increase to 10).
Internal rotation
This is the most important exercise as it strengthens the muscles which helps prevent an anterior shoulder dislocation. Three of the five muscles which medially or internally rotate the shoulder are the pectoralis major, subscapularis, and latissimus dorsi. In the early stages, it is important to keep the shoulder joint in the inner range of motion. This means working from the position where the hand is out in front so it works across the body. Taking the shoulder into the outer range of motion puts it at risk of dislocation.
External rotation
This exercise works the muscle which externally rotates the shoulder. It can be done with a resistance band or a dumbbell. This exercise should be avoided in the very early stages. When the shoulder has healed enough to begin external rotation exercises it is important to remain within the internal range of movement until told otherwise by your therapist.
Externally rotating the shoulder before it is ready puts it at risk of dislocation. Wrap the resistance band around something stable and hold the other end standing so that the band crosses the body. Keeping the elbow bent to 90 degrees and the upper arm by the side, rotate the shoulder to pull the band away from the body.
Abduction
Stand on one end of the band and hold the other end. Keeping the elbow straight, pull your arm out to the side so that the hand ends up level with your shoulder.
Flexion
Stand on the band holding the other end in the hand of your injured arm. Keeping the elbow straight, pull your hand straight up in front of you to about shoulder height. Once the athlete is comfortable with the exercises above, the resistance band can be replaced with weights to progress the strengthening exercises described above.
Adduction
Wrap the band around something secure, hold the other end, and stand with your injured side closest to the attachment. Keeping the elbow straight, pull your hand across your body as far as is comfortable.
Shoulder press
Stand on the center of the band and hold the ends in either hand. Start with the elbows bent and hands at shoulder height. From there, straighten your arms and push up above your head. Slowly return to the starting position and repeat. Many of these exercises can also be performed with free weights as your strength progresses.





6 Comments