PROLAPSED INTER VERTEBRAL DISC (PIVD) PHYSIOTHERAPY MANAGEMENT
Slipped Disc: PROLAPSED INTERVERTEBRAL DISC (PIVD)
Definition of Slipped Disc:
- When the protrusion or extrusion of the nucleus pulposus through a rent in the annulus fibrosus, PIVD occurs.
- Full Form Of PIVD is Prolapse Intervertebral Disc Disease.
- A prolapsed disc is commonly known as ‘slipped disc’, where a disc does not actually slips but the part of the inner softer part of the disc bulges out or herniates through a weakness in the outer part of the disc.
- The prolapsed intervertebral disc is also known as a herniated disc.
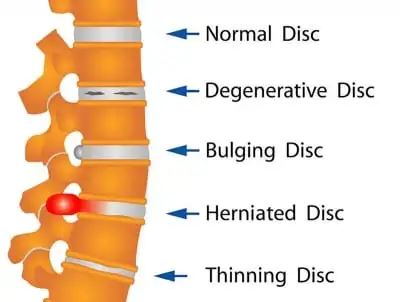
Stages of PIVD:
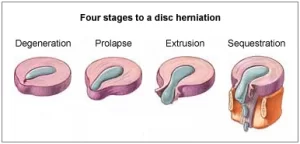
- It has four stages:
- (1) Bulging: At this early stage, the disc is stretched and doesn’t completely return to its normal shape when pressure is relieved. It retains a slight bulge at one side of the disc. Some of the inner disc fibres could be torn and the soft jelly ( nucleus pulposus ) is spiling outwards into the disc fibres but not out of the disc.
- (2) Protrusion: At this stage, the bulge is very prominent and the soft jelly centre has spilled out to the inner edge of the outer fibres, barely held in by the remaining disc fibres.
- (3) Extrusion: In the case of a herniated spinal disc, the soft jelly has completely spilled out of the disc and now protruding out of the disc fibres.
- (4) Sequestration: Here some of the jelly material is breaking off away from the disc into the surrounding area.
- prolapsed disc (commonly called a ‘slipped disc’), a disc does not actually ‘slip’.
- What happens is that part of the inner softer part of the disc (the nucleus pulposus) bulges out (herniates) through a weakness in the outer part of the disc.
- A PIVD /prolapsed disc is sometimes called a herniated disc. The bulging disc may press on nearby structures such as a nerve coming from the spinal cord.
- Some inflammation also develops around the prolapsed part of the disc. Any disc in the spine can prolapse. However, most prolapsed discs occur in the lumbar part of the spine (lower back). The size of the prolapse can vary.
- As a rule, the larger the prolapse, the more severe the symptoms are likely to be.
Lower Back Anatomy:
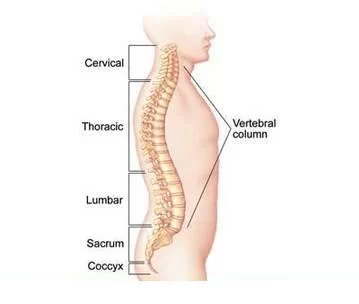
- The spine is made up of many bones called vertebrae. These are roughly circular and between each vertebra is a ‘disc’.
- The discs are made of strong ‘rubber-like’ tissue which allows the spine to be fairly flexible. A disc has a stronger fibrous outer part, and a softer jelly-like middle part called the nucleus pulposus.
- The spinal cord, which contains the nerves that come from the brain, is protected by the spine. Nerves from the spinal cord come out from between the vertebrae to take and receive messages to various parts of the body. Strong ligaments attach to the vertebrae.
- These give extra support and strength to the spine. Various muscles also surround, and are attached to, various parts of the spine.
Anatomy of Intervertebral Discs
- Intervertebral Discs are soft, rubbery pads found between the hard bones (vertebrae) that make up the spinal column. The spinal canal is a hollow space in the middle of the spinal column that contains the spinal cord and other nerve roots.
- The discs between the vertebrae allow the back to flex or bend. Discs also act as shock absorbers. Normal anatomy of lumbar spine. Discs in the lumbar spine (low back) are composed of a thick outer ring of cartilage (annulus fibrosus) and an inner gel-like substance (nucleus pulposus). In the cervical spine (neck), the discs are similar but smaller in size.
- Two layers of cartilage cover the top and bottom aspects of each disc called a vertebral end plate. It separates the disc from the adjacent vertebral body.
- (1) Nucleus pulposus: It is a semi-fluid mass of mucoid material that seems like toothpaste. It consists of a few cartilage cells and irregularly arranged collagen fibers. The fluid nature of the nucleus pulposus allowed it to be deformed under pressure. The nucleus attempt to deform and will thereby transmit the applied pressure in all direction.
- (2) Annulus fibrosus: The annulus fibrosus consists of collagen fibers. The collagen fibers are arranged in between 10 to 20 sheets called lamellae. These are arranged in concentric rings that surround the nucleus pulposus. They are thick in the anterior and lateral portions of the annulus but posteriorly they are finer and more tightly packed. The collagen fibers lie parallel to each other. The posterior portion of the annulus fibrosus is innervated by fibres of sinuvertebral nerve (branch of the dorsal root ganglion). Irritation of the sinuvertebral nerve is responsible for axial back pain.
- Vertebral endplates: Each vertebral end plate is a layer of cartilage about 0.6-1 mm thick. Covers the area on the vertebral area encircled by the ring apophysis. The nucleus pulposus is entirely covered but the annulus fibrosus is only 66% covered by the end plates.
Types of Disc Herniation
- Central
- Paramedial
- Lateral
Causes of PIVD:
- Some children may often suffer from prolapsed disc due to birth defect or injury.
- During adolescence, rapid growth may also be a contributing factor.
- Heavy manual labour.
- Sometimes playing sports like football, gymnastics, weightlifting and track and field may also cause your strain to over stretch and put stress on your lower back.
- Repetitive lifting and twisting.
- Postural stress.
- obesity.
- Poor and inadequate strength of the trunk.
- Sitting for long hours.
- increasing age (a disc is more likely to develop a weakness with increasing age).
Symptoms of PIVD:
- Lower Back /Lumbar Herniated Disc Symptoms:
- Severe low-back pain.
- Pain radiating to the buttocks, legs, and feet.
- Walking can be painful or difficult.
- Pain made worse with coughing, straining or laughing.
- Muscle spasm.
- Tingling or numbness in legs or feet.
- Muscle weakness or atrophy in later stages.
- Loss of bladder or bowel control in case of cauda equina syndrome.
- Some people do not have symptoms of PIVD Research studies where routine back scans have been done on a large number of people have shown that some people have a PIVD without any symptoms. It is thought that symptoms mainly occur if the prolapse causes pressure or irritation of a nerve. This does not happen in all cases. Some prolapses may be small, or occur away from the nerves and cause minor, or no symptoms.
- Neck /Cervical Herniated Disc Symptoms:
- Arm muscle weakness.
- Deep pain near or over the shoulder blades on the affected side.
- Increased pain when bending the neck or turning head to the side.
- Pain made worse with coughing, straining or laughing.
- Neck pain, especially in the back and sides along with spasm.
- Burning pain radiating to the shoulder, upper arm, forearm, and rarely the hand, fingers or chest.
- Tingling (a “pins-and-needles” sensation) or numbness in one arm.
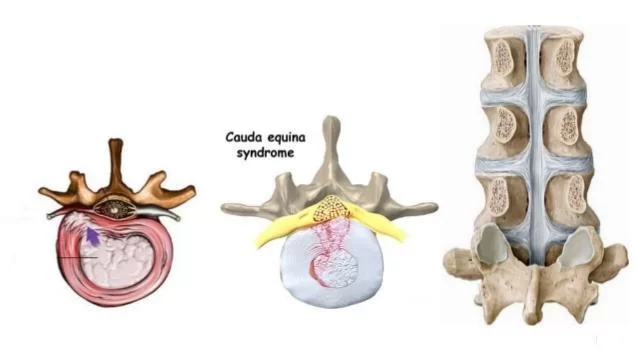
- Cauda equina syndrome is a particularly serious type of nerve root problem that can be caused by a prolapsed disc. This is a rare disorder where the nerves at the very bottom of the spinal cord are pressed on.
- This syndrome can cause low back pain plus: problems with bowel and bladder function (usually unable to pass urine), numbness in the ‘saddle’ area (around the anus), and weakness in one or both legs.
- This syndrome needs urgent treatment to preserve the nerves to the bladder and bowel from becoming permanently damaged. See a doctor immediately if you develop these symptoms.
Bulging Discs vs. Herniated Discs:

- The primary difference between bulging discs and herniated discs are whether they are contained or non-contained:
- A contained disc- such as a bulging disc, has not broken through the outer wall of the intervertebral disc, which means the nucleus pulposus remains contained within the annulus fibrosus.
- A non-contained disc- such as a herniated or ruptured disc, has either partially or completely broken through the outer wall of the intervertebral disc.
- A bulging disc may be a precursor to a herniation. The disc may protrude into the spinal canal without breaking through the disc wall. The gel-like interior (nucleus pulposus) does not leak out. The disc remains intact except a small bubble appears on the outside of the disc.
- When a disc herniates, the contents may compress the spinal cord or the spinal nerve roots. To complicate matters, sometimes fragments from the annulus (the outer disc wall) may breakaway from the parent disc and drift into the spinal canal.
Diagnosis
SPECIAL TESTS FOR PIVD:
- SLR test.
- Laesegue test.
- Bowstring test.
- Femoral stretch test.
IMAGINARY DIAGNOSIS:
- X-Ray:

- An X-ray can be taken by your doctor to diagnose a decrease in the height of space between discs, nerve bundle sclerosis, bone spurs, facet hypertrophy and instability during flexion and extension of limbs.
- CT Scan:
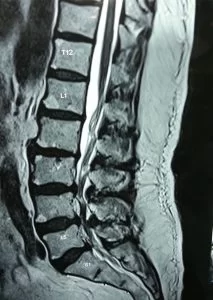
- To provide a detailed anatomic picture of your lumbar spine, also of the phone, which will help your doctor to identify abnormalities.
- MRI Scan:

- The magnetic resonance imaging which diagnoses using magnetic and radio waves, and creates computer-generated images. It is able to show the cut through multiple layers of the tissues.
- EMG Study: An electromyogram test looks at the function of the nerve roots leaving the spine. It is done by inserting tiny electrodes into the muscle of lower extremity. On the basis of the electrical signals in the muscles, it show if the muscle is being pinched or irritated as it leaves the spine.
Gait Pattern in PIVD:
- Excessive Hip Flexion: Due to IT band contractures, Hip flexor spasticity, Hip flexion contractures, hip pain, Compensation for excessive knee flexion and ankle DF, Compensation for excess ankle plantar flexion in mid swing, most commonly the excessive hip flexion can significantly change the gait pattern.
- Hip Abductor Weakness: During the swing phase to allow the opposite leg to lift, the abductor muscles stabilize the pelvis
Treatment of PIVD:
1. Conservative Management:
- (a) Rest: Rest and Anti-inflammatory and analgesics.
- (b) Reduction: Continue bed rest and traction for 2 weeks may reduce the herniation in over 90% cases. If no improvement with rest and traction, epidural injection of corticosteroid and local anaesthetic are given.
- (c) Chemonucleolysis: dissolution of the Nucleus Pulposus by percutaneous injection of a proteolytic enzyme (chymopapain). This enzyme has the property of dissolving fibrous and cartilaginous tissue.
2. Operative Management:
- Indications for operative removal of disc.
- (a) cauda equina compression syndrome that does not clear up with 6 hours of starting bed rest and traction (emergengy).
- (b) Neurological deterioration while under conservative management.
- (c) Persistant pain and signs of sciatic tension after 3 weeks of conservative treatment.
3. Home treatment:


- Patients can also use hot water bags or ice bags to reduce localized pain. Heat can be applied to relax the muscles and to promote blood flow. Ice can be applied to relieve pain.
- Painkillers such as acetaminophen, ibuprofen or oral steroids can be taken to reduce inflammation in the area but with your doctor’s prescription.
The disc is removed by following techniques:
- (a) Hemilaminectomy/Partial laminectomy- Part of the lamina and ligamentum flavum on one side is removed, taking great care not to damage the facet joint.
- (b) Laminectomy:
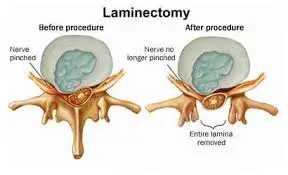
- Laminae on both sides with spinous process are removed. Such wide exposure is required for big, central disc producing cauda equina syndrome.
- (c) Microdiscectomy:
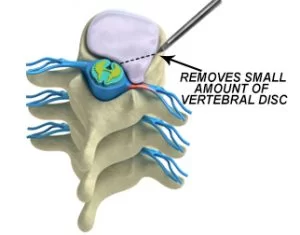
- Done with an operating microscope. Exposure is very limited. Morbidity and hospitalisation is less.
- (d) Fenestration: Ligamentum flavum bridging the two adjacent laminae is excised and spinal canal at affected level exposed.
Physiotherapy Treatment of PIVD:
- Before planning the treatment, determine the position of comfort or symptom reduction i.e FUNCTIONAL POSITION. The patient may have,
- (a) Extension bias: Patient’s symptoms are lessened in position of extension (bending back) and provoked in flexion (bending forwards) e.g PIVD.
- (b) Flexion bias: Patient’s symptoms are lessened in position of spinal flexion (bending forwards) and provoked in spinal extension (bending backwards) e.g spinal stenosis, spondylolisthesis.
Spinal Extension (bending back) is contraindicated if:
- (a) when no position or movement decreases or centralizes the pain.
- (b) when saddle anaesthesia and/or urinary incontinence is present (could indicate spinal cord or cauda equina lesion due to large central disc herniation).
- (c) when patient is in such extreme pain that he rigidly holds the body immobile.
Spinal flexion (bending forward) is contraindicated if:
- (a) when extension relieves the symptoms.
- (b) when flexion increases or peripheralises the symptoms.
Acute Phase:
Aims:
- (a) To relieve pain.
- (b) To promote muscle relaxation.
- (c) To relieve inflammation and pressure against the pain sensitive or neurologic structures.
- (d) patient education.
- (e) prevention.
Physiotherapy management in acute phase of PIVD:
- (A) CONTROLLED REST: is recommended i.e rest in the form of,
- Posture and activity modification- Avoid flexed postures, sitting for long duraton, bending or lifting activities, asymmetric postures ( flexion and rotation). All these increase the disc pressure.
- Local support in the form of corset (lumbosacral belt), abdominal binder, tape etc. These measures will enhance healing and prevent reinjury to the healing disc. Within 10 days fibrin is laid down. If spine is maintained in lordosis, the annulus will heal in shortened position and nucleus will be retained centrally.
- If symptoms are severe, bed rest (maximum for 2 days) on a hard bed is indicated with short periods of walking at regular intervals ( with corset). Walking promotes lumbar extension and stimulates fluid mechanics to help reduce swelling in the disc/connective tissues.
- If patient presents with inability to straighten up, make the patient lie prone with 2-3 pillows under the abdomen. As the pain subsides, remove the pillows and prop up the trunk by placing pillows under the thorax. By this nucleus pulposus is shifted forwards and relieves pain and gains a lordosis.
- (B) MODALITIES TO REDUCE PAIN AND SPASM:
- Cryotherapy: reduces muscle spasms and inflammation in the acute phase.
- TENS: relieves pain in both acute and chronic phases.
- US: as phonophoresis increases extensibility of connective tissues
- Moist heat: used as an adjunct before applying specialised techniques to decrease muscle spasm.
- SWD- pulsed SWD in acute condition and continuous SWD in chronic cases.
- IFT
- Soft tissue manipulation- to reduce local muscle spasm and induce relaxation.
- Traction- may be beneficial to relieve nerve root compression and radiculopathy or paraesthesias in the acute phase of PIVD. Reduces nuclear protrusion by decreasing the pressure on the disc or by placing tension on the posterior longitudinal ligament. Time of traction should be short in acute phase else there could be an increase in disc pressure leading to increased pain due to fluid imbibition ( less than 15 minutes of intermittent traction and less than 10 minutes of sustained traction).
- Traction is contraindicated in disc protrussion medial to the nerve root.
Exercises for Slipped Disc
- Herniated disc exercises play a vital role in treatment of pain and inflammation. Extension exercises are useful in early treatment of disc related signs and symptoms.
- Techniques to mechanically reduce a nuclear disc protrusion- These are used if the test movements show that these movements and postures improve the symptoms:
- (a) Posterior or posterolateral protrusion:
- (i) Passive Extension: Patient is lying prone (i.e on belly). If patient is in such extreme pain, place pillows under the abdomen for support, gradually increase the amount of extension by removing pillows. Progress by having the patient prop himself up on the elbows, allowing the pelvis to sag. Wait for 5-10 minutes between each increment of extension to allow for reduction of water content and size of bulge. Progress by having patient prop on the hands. If sustained postures are not well tolerated, have the patient perform passive lumber extension intermittently by repeating the prone press ups.
- (ii) Lateral shift correction: If patient has lateral shift, first correct lateral shift then start with extension exercises. Therapist stands on the side to which the thorax is shifted and places his shoulder against the patient’s elbow which is flexed against the rib cage. Therapist wraps the arms around patient’s pelvis and pulls pelvis towards him while pushing the patient’s thorax away.
- Self correction: Patient places the hand on the side of the shifted rib cage on the lateral aspect of the rib cage and place the other hand over the crest of opposite ilium. Then gradually push these regions towards midline and hold.
- (b) Anterior protrusion:
- (i) Correction of lateral shift: Patient stands in front of a chair and places the leg opposite to the shift on a chair so the hip is in about 90 degree of flexion. Leg on the side of lateral shift is kept extended. Patient then flexes the trunk onto the raised thigh and applies pressure by pulling on the ankle.
- (ii) Passive flexion: Bring both knees to the chest and hold this position with arm around the thighs.
- (c)Active range of motion exercises within painfree range to the lower limb can be done e.g ankle toe movements, heel drag, hip abduction/adduction.
- (d) Mobilization of thoracic spine Mobilization of segments above and below the affected segmental level.
- (e) Piriformis muscle stretching
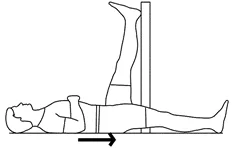
- (f) Maintain/ improve mobility of neural tissues- These exercises should be performed with caution in acute stage, usually in recumbent position. These will prevent chronic complications from increased neural tension e.g passive SLR with foot dorsiflexion.
- (g) Hydrotherapy exercises
- (h) Patient education-These are some movements you should try to avoid:
- bending over to lift very heavy items
- performing squats with too much weight
- low back extensions, as they put high stress levels on discs
- running, since it can place strains on the discs
- any form of resistance training
Subacute Phase:
- Usually the acute symptoms decrease in 4-6 days.
- (a) Continue with the exercises done in acute phase e.g prone press ups, nerve mobility exercises, modalities.
- (b) Simple spinal movements in pain free ranges using gentle pelvic tilts. Pelvic rocking can be done in supine, sitting, prone lying, side lying, standing, quadripud (cat and camel exercise). Emphasize on anterior pelvic tilt so that spine is in extension. Pelvic rolling can be added.
- (c) Isometrics of extensors but caution against holding breath and causing valsalva.
- (d) Encourage aerobic activities, walking, swimming with patient’s tolerance.
Chronic Phase: When the disc symptoms have stabilized.
Aims:
- (a) Restore range of motion.
- (b) Restore muscle strength, endurance and function.
- (c) Retrain kinesthetic awareness and control of normal alignment.
- (d) Patient involvement and education to manage posture to prevent recurrences.
PIVD Exercises In Chronic Stage:
- (a) Gentle active painfree range of motion exercises:
- After 3 weeks from the onset of PIVD symptoms, start side flexion and extension in standing. Progress to adding flexion only when the disc has healed.
- (b) Stretching and flexibility exercises:




- Stretching of the lumbar erector spinae and soft tissues posterior to the spine ( knee to chest position). Following any flexion exercises, conclude with extension exercises such as prone press ups/ standing back extension.
- Hamstring stretch on wall.
- Quadriceps stretch.
- Hip adductor stretch.
- Gluteal stretch.
- Isometric hip adduction.
- (c) Core stability exercises:
- Whenever there is a slight imbalance in the core muscles, you suffer from back pain. Core strengthening exercises help in relieving back pain and form the base of the core stability training program. The aim of these exercises is to provide more support to your back by strengthening the muscles of your spine.
- The Bridging exercise: Strengthens several core muscle groups – e.g buttocks, back, abs for PIVD patients. Lie flat on back; bend knees at 90-degree angle, feet flat on floor. Tighten abs. Raise buttocks off floor, keeping abs tight. Tighten buttocks. Shoulder to knees should be in straight line. Hold for a count of five. Slowly lower buttocks to floor. Repeat five to fifteen times.
- The Plank exercise: Strengthening exercise for back, abs and neck (also strengthens arms and legs)for PIVD patients. Lie on stomach, place elbows and forearms on floor. In a push-up position, balance on your toes and elbows. Keep your back straight and legs straight. (Like a plank) Tighten abs. Hold position for 10 seconds. Relax. Repeat five to ten times. If this exercise is too difficult (as it often is for beginners), balance on your knees instead of your toes.
- The Side Plank: Strengthens the obliques (side abdominal muscles)for PIVD patients. Lie on right side. Place right elbow and forearm on floor. Tighten abs. Push up until shoulder is over elbow. Keep your body in a straight line – feet, knees, hips, shoulders, head aligned. Only forearm and side of right foot are on floor (feet are stacked). Hold position for 10 seconds. Relax. Repeat five times. Repeat on left side. If this exercise is too difficult, balance on stacked knees (bend knees and keep feet off floor) instead of feet.
- The Wall Squat: Strengthening exercise for back, hips and quads in PIVD patients. Stand with your back against a wall, heels about 18 inches from the wall, feet shoulder-width apart. Tighten abs. Slide slowly down the wall into a crouch with knees bent to about 90 degrees. If this is too difficult, bend knees to 45 degrees and gradually build up from there. Count to five and slide back up the wall. Repeat 5 -10 times.
- Leg and arm raises: Strengthening exercise for back and hip muscles in PIVD patients. Lie on stomach, arms reached out past your head with palms and forehead on floor. Tighten abs. Lift one arm (as you raise your head and shoulders) and the opposite leg at the same time, stretching them away from each other. Hold for 5 seconds and then switch sides. Repeat 5 – 10 times.
- Leg lifts: Quad Strengthening Exercise for PIVD patients. Lie flat on back. Bend left knee at 90-degree angle, keeping foot flat on floor. Tighten abs. Keep the right leg straight and slowly lift right foot to the height of the left knee. Hold for a count of 3. Do 10 repetitions. Switch sides and repeat.
- Basic Crunches: upper abdominal exercise for PIVD patients.
- Lie on back, knees bent, feet flat on floor. Do not anchor feet. (Anchoring the feet or keeping the legs straight along the floor can strain the lower back). Head and back should be in neutral position. A rolled up towel may be placed under the natural curve of the lower back to provide extra support – the small of the back should be about an inch above the floor. Place hands behind head with elbows pointing outward. Your hands are used to support your head (to avoid neck from tiring out before abs) but do not pull head forward.Tighten abs. Raise your head and shoulders off the floor – three to six inches is enough. Look at the ceiling to help prevent tilting your head. Keep elbows back.Exhale when raising your torso off the floor and inhale when lowering. Do ten – fifteen repetitions.
- (d)Strengthening exercises:
- Opposite Arm and Leg Extension: balancing / stabilization exercise for PIVD patients: Strengthens muscles running down sides of spine, back of shoulders, hips and buttocks. Begin on all fours, hands directly under your shoulders and knees directly under your hips. Keep head aligned with spine (to help avoid tilting head, look at floor). Keep buttocks and abdomen tight. Do not arch the back. Lift one arm up and forward until it is level with torso; simultaneously lift the opposite leg in the same manner. Keep arm, spine, and opposite leg aligned as if they are forming a tabletop. Balance yourself for 10 seconds then slowly return to starting position. Switch sides and repeat. Remember to breathe. Do five repetitions.
- Leg Lifts: lower abdominal exercise for PIVD patients. Lie flat on back. Bend left knee at 90-degree angle, keeping foot flat on floor. Tighten abs. Keep the right leg straight and slowly lift it until right foot is at the height of the left knee. Hold for a count of 5. Do 5 to 15 repetitions. Switch sides and repeat.
- Backward Leg Swing: Gluteal exercise for PIVD patients.
- (The muscles of the buttocks help support the spine) Stand, holding onto the back of a chair for support. Tighten abs. Swing leg back at a diagonal until you feel your buttocks tighten. Tense muscles as much as you can and swing leg back a couple more inches. Return leg to floor. Do 10 – 15 repetitions. Switch sides and repeat.
- Abdominal strengthening exercises: Isometric abs, knee to chest, bicycle exercises.
- (e) Hydrotherapy exercises for back pain:
- Warm up, mobilising exercises
- Stretching exercises
- Strengthening exercises
- Relaxatation exercises
- Swimming workouts
- (f) Patient Education:
- Teach safe movement patterns and body mechanics.
- Teach patient preventive exercises and mechanics for relief of mechanical stress in daily activities.
- Teach relaxation exercises to cope with muscle tension.
- Instruct patient on how to modify environment e.g bed, chairs, car seats, work area etc.
Electrotherapy treatments for PIVD:
- Ultrasound:- An ultrasound can help to reduce muscle spasms, stiffness, cramping, swelling and pain upto a great extent. It helps by sending sound waves deep inside your tissues creating a gentle heat which increases healing and blood circulation.
- TENS:- A transcutaneous electrical nerve stimulation machine stimulates your muscle with the help of variable intensities of electrical current. It reduces your muscle spasms and increases your body’s production of endorphins, your natural pain killers. ( Electrode placement for PIVD)
- LASER:- Laser therapy treatment is very advance method for pain relief and decrease inflamation,In physiopoint clinic we are using LASER treatment for many painful condition ,and we are getting very good result.It gives an high intensity of light into the tendon. This helps in reduction of inflammation, pain. It also motivates cell reproduction
- Lumbar traction: Lumbar traction can be a emphatic auxillary for the treatment of a number of common musculoskeletal complaints including facet joint pain, disc degeneration and disc protrusion. If the traction is correctly applied for the patients with lumbar disc protrusion, it may reduce the bulging disc, but the mechanical effect is usually transient. To overcome the inertia of the body, 80 to 200 lb of traction is needed to produce effective distraction of disc. Traction treatment time should be kept relatively short which is 10 minutes for sustained traction and 15 minutes intermittently are probably safe and maximum effective.
Manual mobilization for PIVD:
- Manual mobilization is very effective in the treatment of PIVD ( prolapse intervertebral disc),with the help of some hand manual technique we can adject the lumbar disc alingment ,which help in decreasing radiate pain and other symptoms.
FAQs
What is a PIVD?
PIVD stands for “Prolapsed Intervertebral Disc,” which is a medical condition that affects the spine. The spine is made up of individual bones called vertebrae, and between each pair of vertebrae, there is a cushion-like structure known as an intervertebral disc. These discs consist of a tough outer layer called the annulus fibrosus and a gel-like inner core called the nucleus pulposus.
A prolapsed intervertebral disc, also commonly referred to as a herniated disc or slipped disc, occurs when the soft inner core (nucleus pulposus) of the disc pushes through a tear or weak spot in the tough outer layer (annulus fibrosus). This can result in pressure on nearby spinal nerves, leading to pain, numbness, tingling, or weakness in the area of the body served by those nerves.
How do you treat PIVD?
Treatment for PIVD typically begins with conservative measures such as rest, physical therapy, pain medications, and exercises aimed at relieving pressure on the affected nerve. If conservative treatments are not effective, more invasive options might be considered, including epidural steroid injections or, in severe cases, surgical intervention to remove or repair the herniated portion of the disc.
What is the reason for PIVD?
Actually, PIVD is an age-related issue. But disc prolapse/hernias can also be caused by trauma, stresses, twisting, or hard lifting. Although it can happen in any disc of the spine, prolapsed lumbar and cervical discs are the most typical locations.
What is PIVD stages?
There are 4 stages of PIVD
Bulging disc
Protrusion.
extrusion
sequestrization
What are the symptoms of L4-L5 PIVD?
Symptoms Of Lumbar Spine L4-L5 are:
Many individuals experience tingling, numbness (pins and needles), and soreness or burning in their legs and on the top of their feet. In extreme circumstances, a slipped disc in the L4-L5 causes weakness in the legs or feet. Some people could even be unable to walk, which makes it impossible for them to stand.
Can PIVD be cured without surgery?
A herniated disc is one in which the center, or nucleus, of the disc pushes outward, perhaps even through the wall of the disc. The good news is that the majority of herniated discs can be solved with manual therapy, exercise, or IDD Therapy disc treatment without requiring surgery.




The information regarding pivd was very helpful to me ..
But I want to know is masturbating is also relates with this desease or not
It’s actually very helpful as it not only provides the basic knowledge but also the best treatment in a simple way…..
I hopefully wait for the other topics took
it’s actually very helpful as it not only provides the basic knowledge but also the the best treatment in a simple way ..
I hopefully wait for the other topics took .
very useful thnkuuu
Thank you so much for lot of to understand about pivd it’s very helpful to me ❤️