Rheumatoid Arthritis (RA)
What is Rheumatoid Arthritis (RA)?
Rheumatoid arthritis is an autoimmune disease where your immune system damages your healthy cells, causing joint pain, and inflammation with swelling in the affected parts of the body mainly the small joint of the hands on both sides of your body.
RA mainly affects the joints, mostly many joints at once. It mainly affects joints in the hands, wrists, and knees. This may lead to long-lasting joint pain, deformity, and difficulty in walking.
Rheumatoid arthritis can also affect other body parts and cause problems in organs eg. lungs, heart, and eyes.
Treatments in RHEUMATOID ARTHRITIS(RA) with emphasis on Resistive exercise protocol
DEFINITION:
- RA is a chronic, systemic inflammatory disorder that may affect many tissues and organs, but principally affects synovial membranes of multiple joints.
- Prevalence is 1 to 2 %.
- Female: Male ratio is 3:1.
- The usual age of onset is 20 to 40 years though individuals of any age group may be affected.
Causes of Rheumatoid Arthritis:
- The cause of rheumatoid arthritis is unknown.
- Even though infectious agents such as viruses, bacteria, and fungi have long been suspected, none has been proven as the cause.
- The cause of rheumatoid arthritis is a very active area of worldwide research.
- Some researchers believe an infection with a bacteria or virus can trigger the development of RA in someone who is genetically susceptible.
Pathophysiology:
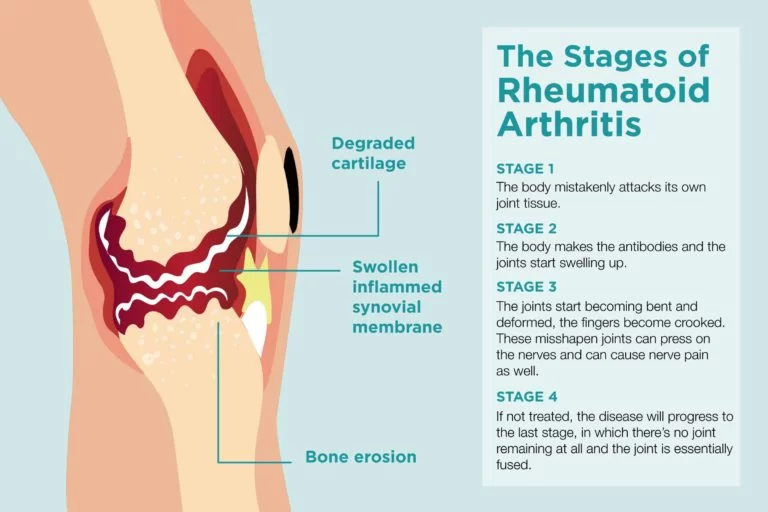
- RA is a complex process, involving synovial cell proliferation and fibrosis, pannus formation, and cartilage and bone erosion.
- This process is mediated by an interdependent network of cytokines, prostanoids, and proteolytic enzymes.
Proinflammatory cytokines, such as interleukin-1 (IL-1) and tumour necrosis factor-alpha (TNF-a), are central mediators in RA. - In the acute phase, effusion and other manifestations of inflammation are evident.
- In the later stages, ankylosis of the joint may set in.
- So in both the acute and chronic phases, there may be widespread inflammation of the tissues around the joint that can lead to significant joint destruction.
Symptoms of RA:
- Usually presents insidiously.
- Prodromal syndrome of malaise, weight loss, and vague periarticular pain and stiffness may be seen.
- Less commonly, the onset is acute, triggered by a stressful situation such as infection, trauma, emotional strain, or in the postpartum period.
- The joint involvement is characteristically symmetric with associated stiffness, warmth tenderness, and pain
- The stiffness is characteristically worse in the morning and improves during the day; its duration is a useful indicator of the activity of the disease. The stiffness may recur especially after strenuous activity.
- The usual joints affected by rheumatoid arthritis are the MCP joints, the PIP joints, the wrists, knees, ankles, and toes.
- Entrapment syndromes may occur, especially carpal tunnel syndrome.
- 20% of patients with rheumatoid arthritis will have subcutaneous nodules, usually seen over bony prominences.
Splenomegaly and lymphadenopathy can occur. Low-grade fever, anorexia, weight loss, fatigue, and weakness can occur. - After months to years, deformities can occur; the most common are:
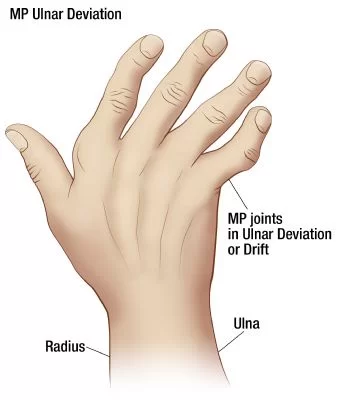
- Ulnar deviation of the fingers.
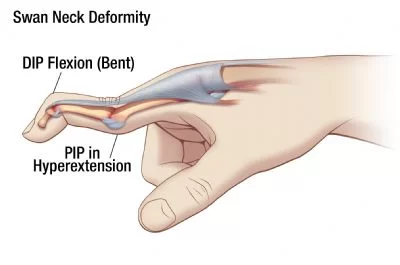
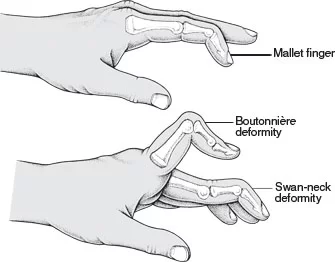
- Swan neck deformity, which is hyperextension of the distal interphalangeal joint and flexion of the proximal interphalangeal joint.
- Boutonniere deformity, which is flexion of the distal interphalangeal joint and extension of the proximal interphalangeal joint.
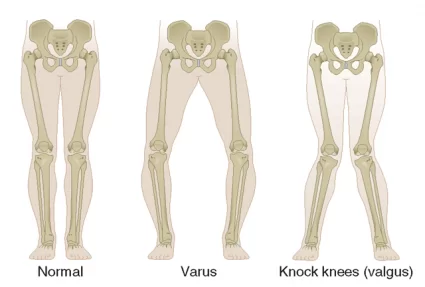
- Valgus deformity of the knee.
- Dryness of the eyes, mouth, and other mucus membranes is found, especially in advanced disease.
Pericarditis and pleuritis can occur but are usually clinically silent.
Diagnosis
Diagnosis
Diagnosis
Based on your symptoms, a physical examination, and the outcomes of x-rays, scans, and blood tests, rheumatoid arthritis is diagnosed.
Since there isn’t a single test that can confirm you have RA, diagnosing RA can take time. The identical symptoms are also present in a number of different illnesses.
During physical examination, your doctor examines your symptoms. Your Doctor Checks your joints for pain, swelling joint stiffness. Since rheumatoid arthritis can affect multiple body regions at once, it’s critical to report all of your symptoms to your doctor, even if they don’t appear to be connected.
They may schedule blood tests to help confirm a diagnosis and recommend you to a rheumatologist if they believe you have rheumatoid arthritis.
Blood Examinations
It is not possible to diagnose RA with a single blood test. A few tests, however, may be able to identify potential symptoms of the illness. The tests that are most important are listed below.
Erythrocyte sedimentation rate (ESR)
A test tube filled with fluids is filled with a sample of your red blood cells. The cells are timed to determine how long it takes them to reach the tube’s bottom. You may have higher-than-normal levels of inflammation if the cells sink more quickly than usual. Rheumatoid arthritis is but one potential reason.
CRP, or C-reactive protein
This test can determine whether your body is inflamed. It accomplishes this by measuring the level of CRP in your blood. Your body may be inflamed if the CRP level is higher than normal.
Full blood count
A full blood count provides your red blood cell count. Less red blood cells mean that your iron content is low because your body requires them to carry iron. This could indicate that you have anemia (an-ee-me-er), which is prevalent in RA patients but does not establish RA.
Rheumatoid factor as well as antibodies against CCP
In around half of cases, rheumatoid factor is in the blood when rheumatoid arthritis first appears. Rheumatoid factor, however, is also positive in about 1 in 20 individuals without rheumatoid arthritis.
You can also take an additional antibody test known as anti-CCP. Anti-CCP-positive individuals have a high risk of developing rheumatoid arthritis. However, not every patient with the illness possesses this antibody.
Scans
To look for joint injury and inflammation, scans might be performed. These can be used to determine the course of rheumatoid arthritis and to identify the illness.
These could consist of:
- X-rays: they will reveal any alterations to your joints.
- Ultrasound scans: these procedures use high-frequency sound waves to build an image of your joints.
- Magnetic resonance imaging (MRI) scans employ strong magnetic fields and radio waves to create images of your joints.
DIFFERENT TYPES OF TREATMENTS:
- There are mainly four types of treatment available in RA.
(1) Pharmacological agents
(2) Braces and bandages
(3) Surgery
(4) Activity modification and Exercise therapy
1. Pharmacological treatment for Rheumatoid Arthritis:
Main goals of the Pharmacological treatment is to:
– Reduce the pain
– Reduce the inflammation
– Reduce further damage and disability
Drugs used in RA:
(a) NSAIDs
(b) DMARDs
(c) Corticosteroids
(a) NSAIDs
Ibuprofen, Naproxen, Acetylsalicylic acid, and other NSAIDs are effective in pain relief, and in reducing inflammation.
They are associated with a number of side effects which include:
– GI irritation
– Peptic ulcers
– Kidney damage
– Liver damage
(b) DMARDs
(Disease Modifying Anti-Rhematoid Drugs)
This drug group has various mechanisms of action. They can alter laboratory markers of inflammation such as CRP and ESR.
E.g. Sulfasalazine, Hydroxychloroquine
Use: It is the first line of drug treatment. It can be used for the treatment of moderate to severe active RA in adults over 18 years of age.
(c) Corticosteroids
E.g. Prednisolone, Budesonide
Use: As continuous oral background therapy, to cover the delayed benefits of DMARDs, as intra-articular injections into inflamed joints or i..m. or i.v. injection during a flare of RA
Adverse effect:
-Avascular necrosis of bone
-Depression and psychosis
-Peptic ulceration
-Cataract (chronic use)
-Raised ICP and convulsions,
-Blood hypercoagulability,
-Menstrual disorders,
-Immunosuppression
2. Braces and bandages
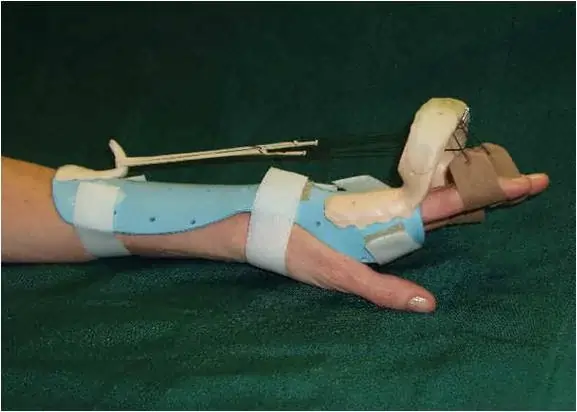

- Braces and splints are designed to relieve pain and stabilize & protect joints during periods of inflammation, when joints (especially those in the hands and wrists) are more prone to injury.
- Usually, Splints are lightweight and are easy to remove, allowing for range-of-motion exercises several times daily.
- Prolonged or improper use of splints can increase stiffness and progressively diminish muscle strength and joint mobility.
3. Surgery in RA
- Surgeries considered for people who have severe rheumatoid arthritis include:
Finger and hand surgeries: To correct joint problems in the hand.
Arthroscopy: This removes debris or inflamed tissue in a joint through a small lighted instrument.
Synovectomy: To remove inflamed joint tissue.
Arthroplasty: To replace part or all of a joint in the hip or knee. - Cervical spinal fusion, to treat severe neck pain and nerve problems.
- Resection of metatarsal heads, to remove deformed bone in the feet.
4. Physiotherapy Treatment and Exercise therapy
- Exercise testing for Resistance exercises
- Benefits of resistance exercise:
(1) Reduces inflammation and pain.
(2) Prevent contractures and deformities.
(3) Maintain or improve range of motion, muscle strength, and cardiovascular fitness.
(4) Improves bone mineral density after corticosteroid administration.
(5) Hand strengthening may improve dexterity and grip strength.
- Types of resistance training:
- Isometric and isotonic exercise
- Hydrotherapy
- Use of Weights
- Elastic bands
- Weight machines
- Benefits of exercise training for persons with arthritis
- Cardiorespiratory:
Aerobic exercise improves cardiorespiratory endurance, pain, function, and with resistance training mood.
Aerobic training improves fitness without worsening disease activity. - Skeletal muscle strength and endurance:
Exercise that includes: Functional strengthening improves strength, pain, fitness, and mobility.
Hand strengthening may improve dexterity and grip strength. - Flexibility:
Joint mobility improves with dynamic exercise training. - Body composition: A combination of aerobic and resistance training decreases the percent body fat without significant weight loss and slow bone mineral density loss
EXERCISES PRESCRIPTIONS:
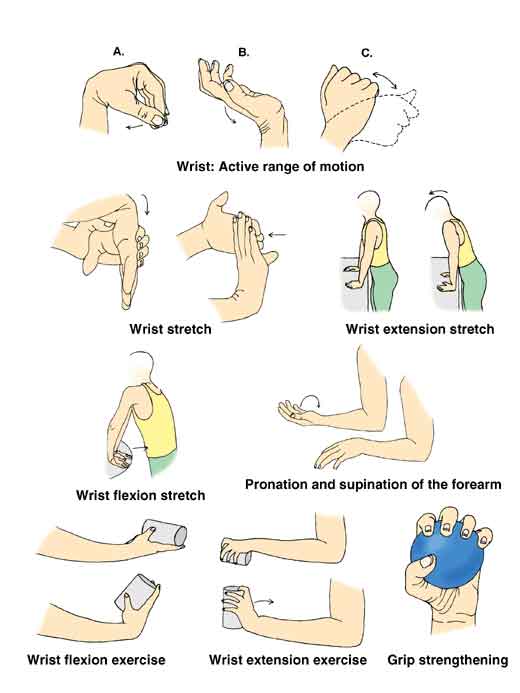
Strengthening exercises (e.g., weight training):- Help to keep or increase muscle strength. Strong muscles help support and protect joints affected by arthritis. Hand strengthening exercise is to improve grip strength.
- Range-of-motion exercises: Help to maintain normal joint movement and relieve stiffness. This type of exercise helps maintain or increase flexibility.
- Aerobic or endurance exercises (e.g., bicycle riding):- Improve cardiovascular fitness, help control weight, and improve overall function. Weight control can be important because extra weight puts extra pressure on many joints.
- Some studies show that aerobic exercise can reduce inflammation in some joints.
- Range-of-motion exercises can be done daily and should be done at least every other day.
- Strengthening exercises should be done every other day.
- Endurance exercises should be done for 20 to 30 minutes three times a week. According to the American College of Rheumatology, 20- to 30-minute exercise routines can be performed in increments of 10 minutes over the course of a day
SPECIAL CONSIDERATION:
- Hydrotherapy may attenuate pain and stiffness and reduce reliance on NSAIDs.
- Stretch and warm up with range-of-motion exercises.
- Start strengthening exercises slowly with small weights.
- Use cold packs after exercising.
- Consider appropriate recreational exercise (after doing range-of-motion, strengthening, and aerobic exercise).
Observation and Continued Care
It’s critical to receive regular medical treatment since your doctor can:
Track the course of the illness.
Assess the effectiveness of the drugs.
Talk to you about any side effects of the medication.
As necessary, modify your course of treatment.
Usually, monitoring involves routine medical appointments. In addition, it could involve imaging tests like X-rays and urine and blood testing. Osteoporosis is more common in people with rheumatoid arthritis, especially those who use corticosteroids. A bone disorder called osteoporosis makes bones brittle and prone to breaking. Discuss with your physician the advantages of taking calcium and vitamin D supplements or other osteoporosis treatments, as well as your risk for the condition.
Because rheumatoid arthritis can impact other organs, your doctor might also keep an eye on your respiratory or cardiovascular health. An increased risk of infection is a potential side effect of many rheumatoid arthritis medicines. Your doctor may keep an eye out for infections. In order to reduce the likelihood and severity of illnesses, vaccinations may be advised.
Rheumatoid arthritis is treated by whom?
Rheumatoid arthritis diagnosis and treatment need collaboration between you and many medical specialists. These could consist of:
- Rheumatologists: Specialists in autoimmune illnesses, arthritis, and other conditions affecting the bones, joints, and muscles are known as rheumatologists.
- Physician assistants: professionals who support physicians in disease diagnosis, treatment, and follow-up.
- Primary care physicians, who focus on adult diagnosis and treatment, include interns and nurse practitioners.
- Orthopedic surgeons are doctors who specialize in treating and operating on conditions affecting the bones and joints.
- Specialist physicians: Patients whose organs, such as the heart or lungs, are affected by rheumatoid arthritis should contact specialists such as cardiologists or pulmonologists.
- Podiatrists are medical professionals who specialize in treating and operating on foot issues.
- Physical therapists: they aid in enhancing joint health.
- Occupational therapists: they provide instruction on how to decrease pain, protect joints, carry out daily tasks, and save energy.
- Pharmacists are those who distribute drugs and assist in determining dosage and possible drug interactions.
- Dietitians, who provide advice on how to eat healthily and keep a healthy weight.
- Nurse educators are experts in assisting patients in comprehending their overall health and formulating treatment strategies.
- Social workers and mental health specialists assist patients in overcoming challenges at work and home that may arise from their medical issues.
Complications
RA gradually destroys joints, which results in some impairment. Both joint pain and stiffness issues may result from it. It might be harder for you to do your regular daily duties and activities. Additional issues like anxiety and sadness may result from this.
Numerous non-joint body organs, including the kidneys, lungs, heart, skin, nerves, muscles, and blood vessels, can also be impacted by RA. Serious sickness or even death may result from these consequences.
Differential Diagnosis
- Osteoarthritis
- Psoriatic arthritis
- Systemic lupus erythematosus
- Sjogren syndrome
- Polymyalgia rheumatic
- Chronic gouty arthritis
- Calcium pyrophosphate deposition disease
Epidemiology
In the developed world, 0.5–1% of adults suffer from RA, and between 5 and 50 out of every 100,000 persons are newly diagnosed with the illness annually. It caused over 49,000 fatalities worldwide in 2010.
Under the age of 15, onset is rare, and from that point on, the incidence increases with age up to the age of 80. Three to five times as many women as men are impacted.
For women, the condition often begins between the ages of 40 and 50, and for men, it begins slightly later. Since RA is a chronic condition, its natural path almost always consists of persistent symptoms that fluctuate in intensity and a progressive degeneration of joint structures that leads to deformities and incapacity. However, spontaneous recovery do occasionally occur.
Rheumatoid arthritis (RA) and periodontitis are connected, and it is thought that this relationship results in increased production of RA-associated autoantibodies. Blood-borne oral bacteria can potentially trigger long-term inflammatory reactions and the production of autoantibodies.
Prognosis
Rheumatoid arthritis is a progressive disease that increases morbidity and death and has no known cure. Every person will go through numerous exacerbations and, in the absence of therapy, often have poor outcomes with increased death and disability. In terms of swollen joint count and sore joint count, early treatment (within six months of symptom onset) has demonstrated better functional capacity and decreased disease activity. However, patients who received treatment early on or later (after six months of symptoms) had identical death rates, and both groups showed a considerable improvement over those who did not receive treatment. Within 10 years of receiving a diagnosis, 40% of RA patients will experience a functional disability that limits their capacity to work and carry out everyday tasks.
The development of other chronic illnesses or problems in RA patients has a significant impact on their prognosis. The association between RA and atherosclerotic cardiovascular disease, which accelerates the development of coronary artery disease, is the most prominent example of this correlation. Patients with RA are more likely to develop lung conditions, cardiovascular disease, and cancer, all of which raise the possibility of these conditions leading to early death.
Living with Rheumatoid Arthritis
Studies reveal that patients who are actively involved in their own care report lower levels of pain and fewer medical visits. Additionally, their quality of life is higher.
You may contribute to managing your RA and enhancing your health by practicing self-care. One may:
- Study up on the symptoms and therapies of rheumatoid arthritis.
- To help you stay active and manage your pain, try several exercises and relaxation techniques.
- To have more control over your illness, establish effective communication with your medical team.
- Seek assistance to manage the psychological, emotional, and physical consequences of rheumatoid arthritis.
By taking part in your care, you can increase your self-assurance in your capacity to carry out daily tasks and live a full, active, and independent life.
Modifications in Lifestyle
There are several things you may do to assist yourself become more independent and optimistic.
Take a break and work out. Maintain a balance between your RA activity and rest, getting more sleep when it’s active and more exercise when it’s not. Fatigue, pain, and active joint inflammation can all be reduced with rest. Shorter rest intervals spaced out throughout the day are generally more beneficial than extended periods of bed rest. Exercise has a crucial role in maintaining flexibility, joint mobility, and strong, healthy muscles.
Exercise is beneficial:
- Become more sleep-oriented.
- Reduce pain.
- Have a positive mentality.
- Sustain a healthy weight.
Low-impact workouts, including swimming exercise regimens, may occasionally be advised by doctors. Consult your medical professionals before starting any fitness regimen.
Collaborative care. Some individuals discover that applying a splint to a troublesome joint for a brief period of time lessens swelling and pain. Splints are typically used on the hands and wrists, although they can also be used on the ankles and feet. Before using a splint, see your physician, a physical therapist, or an occupational therapist.
You may protect your joints in the following ways:
- Using self-help tools, like long-handled shoehorns, zipper pullers, or objects with a wide grasp.
- Using equipment, like silverware or an adaptable toothbrush, to assist with daily tasks.
- Use equipment to assist with getting into and out of beds, chairs, and toilets.
- Selecting actions that will ease the strain on your joints, such as minimizing the usage of stairs or stopping to rest while traveling greater distances on foot.
- Keeping yourself at a healthy weight helps lessen the strain on your joints.
Symptom observation. It’s critical to keep an eye out for any changes in your symptoms or the emergence of new ones. When your pain flares up, you and your doctor can better manage your pain if you have an understanding of your symptoms and how they could change.
Control of stress. Your stress level may rise due to the emotions associated with RA, such as fear, anger, and frustration, as well as any pain, physical restrictions, and the unpredictability of flare-ups. Living with the condition might be more challenging when under stress. Your level of pain perception may also be impacted by stress. Some strategies for managing stress include:
- Regular intervals of rest.
- Methods for relaxing include deep breathing, meditation, or peaceful music or noises.
- Programs for movement exercise, such as tai chi and yoga.
Management of mental health. Living with RA can be difficult and depressing. See your physician, a mental health professional, or an RA support social worker if you are experiencing feelings of isolation, anxiety, or depression due to your illness. Maintain open channels of communication. Inform your loved ones about your RA to assist them in understanding the condition. Getting involved in an online or local support group can be beneficial for you.
A nutritious diet. Maintaining general health requires eating a balanced, nutrient-rich diet that is high in calories, protein, and calcium. Alcohol use should be discussed with your doctor as it may interfere with the rheumatoid arthritis medicine you take.
Consult your doctor before changing your diet or level of exercise.




27 Comments