Osteoarthritis (OA)
What is an Osteoarthritis (OA)?
Arthritis is inflammation of one or more of your joints. Pain, swelling, and stiffness are the primary symptoms of arthritis. Any joint in the body may be affected by the disease, but it is particularly common in the knee.
Knee arthritis can make it hard to do many everyday activities, such as walking or climbing stairs. It is a major cause of lost work time and a serious disability for many people.
The most common types of arthritis are osteoarthritis and rheumatoid arthritis, but there are more than 100 different forms. While arthritis is mainly an adult disease, some forms affect children.
Although there is no cure for arthritis, there are many treatment options available to help manage pain and keep people staying active.
Anatomy of Knee Joint
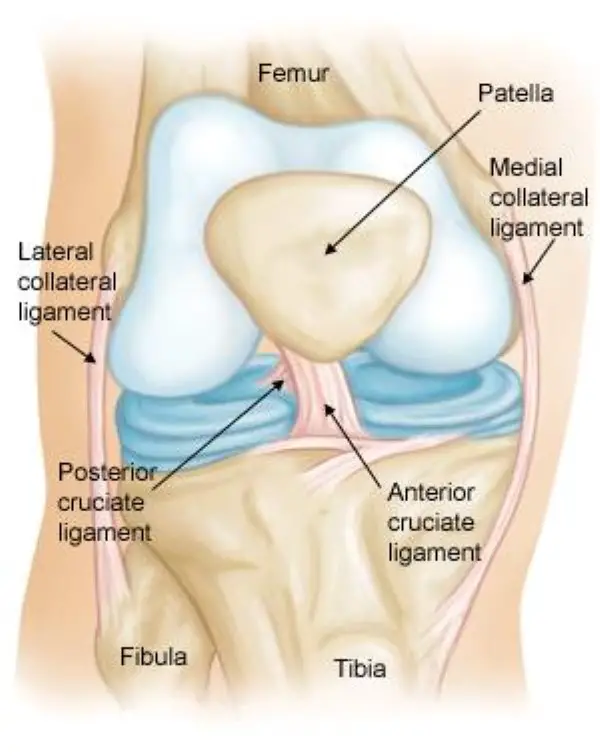
Anatomy of knee joint
The knee is the largest and strongest joint in your body. It is made up of the lower end of the femur (thighbone), the upper end of the tibia (shinbone), and the patella (kneecap). The ends of the three bones where they touch are covered with articular cartilage, a smooth, slippery substance that protects and cushions the bones as you bend and straighten your knee.
Two wedge-shaped pieces of cartilage called meniscus act as “shock absorbers” between your thighbone and shinbone. They are tough and rubbery to help cushion the joint and keep it stable.
The knee joint is surrounded by a thin lining called the synovial membrane. This membrane releases a fluid that lubricates the cartilage and reduces friction.
DEFINITION:
- Osteoarthritis is a chronic, degenerative disorder of multifactorial etiology, characterized by loss of articular cartilage and periarticular bone remodeling, particularly large weight-bearing joints.
- Common in older patients but can occur in younger patients ( genetic mechanism, previous joint trauma).
- The most common form of arthritis.
Pathophysiology
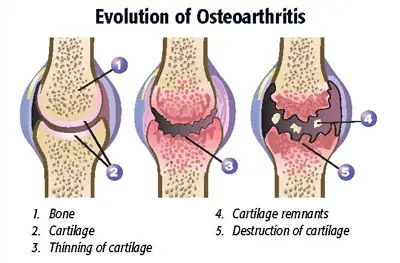
- It is caused by the breakdown of cartilage.
- Cartilage is the tough elastic material that covers and protects the ends of bones. Bits of cartilage may break off and cause pain and swelling in the joint between bones.
- This pain and swelling is called inflammation.
- Degenerative alterations primarily begin in the articular cartilage
- External forces accelerate the catabolic effects of the chondrocytes and disrupt the cartilaginous matrix.
- Enzymatic destruction increases cartilage degradation. proteoglycans and collagen synthesis.
- Decreased strength of the cartilage is compounded by adverse alterations of the collagen.
- Reduced contact area of the cartilage.
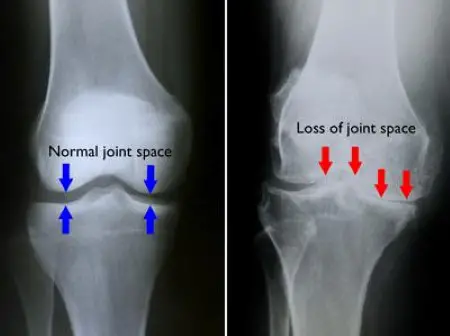
- Loss of cartilage results in the loss of the joint space.
- Progressive erosion of the damaged cartilage occurs until the underlying bone is exposed.
- Subchondral bone responds with vascular invasion and increased cellularity, at areas of pressure.
- The traumatized subchondral bone may undergo cystic degeneration.
- At nonpressure areas along the articular margin? irregular outgrowth of new bone (osteophytes).
- The surface layer of cartilage breaks down and wears away, causing the bones under the cartilage to rub together.
- Pain, swelling, and loss of motion result.
- Formation of bone spurs.
Causes of Osteoarthritis
Primary Osteoarthritis causes:
- Idiopathic
- Defective gene
Secondary Osteoarthritis:
- Obesity
- Repetitive use (ie, jobs requiring heavy labor and bending)
- Previous trauma (ie, posttraumatic OA)
- Infection
- Crystal deposition
- Acromegaly
- Previous rheumatoid arthritis (ie, burnt-out rheumatoid arthritis)
- Heritable metabolic causes (eg, alkaptonuria, hemochromatosis, Wilson disease)
- Hemoglobinopathies (eg, sickle cell disease, thalassemia)
- Underlying orthopedic disorders (eg, congenital hip dislocation, slipped femoral capital epiphysis)
- Disorders of bone (eg, Paget disease, avascular necrosis)
- Joint injury:
- Sports injury (Wear and tear in a joint)
- Occupation (Squat position over many years).
- Other disease RA
- High heel shoes.
Signs and Symptoms of Osteoarthritis
- Knee Pain
- Swelling.
- Stiffness.
- Instability.
- Tenderness.
- Effusion.
- Crepitus.
- Limitation of movement and muscle wasting.
In the early stage,
- Joints may appear normal.
- Gait may be antalgic if weight-bearing joints are involved.
In late stage,
- Visible osteophytes may be noted.
- Joints may be warm to palpation.
- Palpable osteophytes frequently are noted.
- Joint effusion frequently is evidenced in superficial joints.
- Range of motion limitations, because of bony restrictions and/or soft tissue contractures are characteristic.
- Crepitus with range of motion is not uncommon.
Diagnosis of Osteoarthritis
Imagine test:
- Joint aspiration: The doctor will numb the affected area and insert a needle into the joint to withdraw fluid. The fluid will be examined for evidence of crystals or joint deterioration. This test can help rule out other medical conditions or other forms of arthritis.
- X-ray: X-rays can show damage and other changes related to osteoarthritis to confirm the diagnosis.
- MRI: Magnetic resonance imaging (MRI) does not use radiation. It is more expensive than X-rays but will provide a view that offers better images of cartilage and other structures to detect early abnormalities typical of osteoarthritis.
Lab tests
Analyzing your blood or joint fluid can help confirm the diagnosis.
- Blood tests: Although there is no blood test for osteoarthritis, certain tests may help rule out other causes of joint pain, such as rheumatoid arthritis.
- Joint fluid analysis: Your doctor may use a needle to draw fluid out of the affected joint. Examining and testing the fluid from your joint can determine if there’s inflammation and if your pain is caused by gout or an infection.
Treatment Osteoarthritis
- Symptomatic treatment.
- Structure modifying treatment.
- Surgical treatment.
Physiotherapy Treatment of Osteoarthritis
- Physiotherapy and exercise improve flexibility and strengthen the muscles surrounding the joints.
- People who exercise regularly for their arthritis will typically have less pain and better function than those who are inactive.
Physiotherapy treatment program:
- Reduce pain.
- Improve movement and posture.
- Strengthen muscles.
- Improve independent function.
- Assess and treat biomechanical problems that may exacerbate the pain and loss of function.
Exercise can help:
- prevent the disability that results from inactivity.
- It promotes the health and normal function of muscles and bones.
- Exercise keeps the muscles toned and increases bone mineral density, which reduces the risk of osteoporosis and fractures. It also promotes cardiovascular health, which decreases the risk of heart disease.
- In addition, there are also psycho-social benefits to exercise, including an improved sense of well-being and the relief of depression
RANGE OF MOTION EXERCISES:
- Range-of-motion exercises are gentle stretching exercises that move each joint as far as possible in all directions.
- These exercises need to be done daily to help keep joints fully mobile and prevent stiffness and deformities.
- ROM (range-of-motion) exercises are especially important for arthritis patients, who because of intense inflammatory pain tend not to want to move painful joints.
STRENGTHENING EXERCISE:
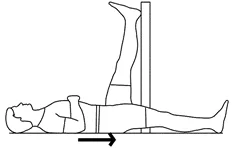
- Strengthening exercises help increase muscle strength. Strong muscles help to support the joints, making the joints more stable, and helping a person move more easily and with less pain.
- The two types of strengthening exercises are isometric and isotonic:
- Isometric exercises involve tightening the muscles, without moving the joints. These exercises are especially useful when joint motion is impaired.
- Isotonic exercises involve strengthening the muscles by moving the joints.
STRETCHING EXERCISE:
- Stretching the muscles that support the knee is important in preventing injury. Flexible muscles are not as easily injured as tight muscles. Tightness of muscles connected to the knee can also pull the knee out of alignment.
- When doing stretching knee exercises, be careful to go slowly and not to overstretch.
AEROBIC EXERCISE:
- Aerobic exercise benefits those with knee problems by toning the muscles of the leg that support the knee joint to absorb shock before it reaches the knee joint.
- Aerobic exercises also help in weight reduction. Losing weight reduces stress on the knee joint – the impact placed upon on the knees is three times the body weight while walking.
- Aerobics also stimulate your body to release endorphins – natural painkillers produced by one’s own body.
- Aerobic exercise is important for the health of the heart, lungs, and overall function of the body.
- Warm up before aerobic exercise to slowly increase your heart rate and breathing rate. Five minutes of slow-paced walking and a few minutes of stretching are sufficient. Cooling down in the same manner is also important be sure to stretch your quadriceps and hamstrings.
WALKING:
- Start with about 5 minutes of slower-paced walking to warm up.
- Walk at a medium pace for about another 10 minutes per day and gradually build up to 30 – 60 minutes by adding a few minutes each time you walk.
- End your walk with 5 minutes of slower-paced walking.
- After you get into better shape you can start walking at a faster pace to increase the intensity of your walks.
SWIMMING AND WATER EXERCISES:
- swimming is an excellent no-impact exercise. Regular ‘land’ exercises can also be done underwater.
- The buoyancy of the water supports most of the body’s weight while the resistance of the water makes your muscles work harder to perform movements.
- You can use dumbbells and weights strapped to the ankles to intensify the workout without stressing the knees and other weight-bearing joints.
STATIONARY BIKE:
- Make sure your seat is high enough so that your knees are not bent beyond a 90-degree angle. Your knee should be slightly bent when your pedal is furthest away. An upright stationary bike (looks like a regular bike) gives you a higher-intensity workout than a recumbent bike.
HEAT AND COLD THERAPIES:
- Applying heat and cold to arthritic joints can help to control symptoms such as pain and stiffness.
- Heat therapy: Heat relieves pain and stiffness in arthritic joints. Heat can be applied to the joints with hot packs, hot water bottles, heating pads, or electrically heated mittens. Heating pads should be set on a timer and used for no more than 20 minutes at a time. The heating pad can be reapplied after 20 minutes of no use.
- Cold therapy: Cold relieves pain in arthritic joints and reduces muscle spasms. Cold can be applied for short periods using ice packs or topical coolant sprays. People with certain medical conditions, such as the Raynaud phenomenon, should not use cold therapy.
ORTHOSIS AND ASSISTIVE DEVICES:
ORTHOSIS For Osteoarthritis:
- Orthoses are devices that promote normal alignment and function of the joints. There are many different types of orthosis that can reduce symptoms and help maintain function in people with osteoarthritis.
- Well-cushioned shoes and shoe inserts may reduce stress on the joints of the spine and leg.
- Splints that immobilize the joints can reduce pain and inflammation, and many splints can be worn throughout the day and night. Braces can help stabilize unstable joints.
ASSISTIVE DEVICES:
- Canes, walkers, electric-powered seat lifts, raised toilet seats, and tub and shower bars can reduce the stress on joints and make it easier to perform daily tasks.
TENS/IFT THERAPY:
- A TENS/IFT unit delivers a mild electrical current to the skin, stimulating nerve fibers in the skin that may interfere with the transmission of pain signals from the arthritic joint.
- The use of TENS for people with osteoarthritis is controversial. Some studies have found that those who use TENS for arthritis of the knee have reduced knee pain, a greater ability to bend the knee, and a reduced duration of morning stiffness.
- However, one study found that the benefits occurred primarily during active use of the TENS unit, and another study found that TENS was no more effective for relieving pain than the drug naproxen.
ACTIVITY LIMITATIONS:
- The following positions and activities place excessive pressure on the knee joint and must be limited until knee pain and swelling resolve: Squatting, Kneeling, Twisting and pivoting, repetitive bending, and Bicycling.
- The preferred exercise equipment for the knee should provide smooth motion of the knee, and maximal toning of the front and back thigh muscles (quadriceps and hamstring muscles).
PRIMARY PREVENTION OF OA:
- Regular exercises.
- Weight control.
- Prevention of trauma.
AIMS OF TREATMENT:
- Pain relief.
- Preservation and restoration of joint function.
- Education.
NON-PHARMACOLOGICAL TREATMENT OF OA:
- Patient education.
- Weight loss (if overweight).
- Aerobic exercise programs.
- Physical therapy.
- Range-of-motion exercises Muscle-strengthening exercises.
- Assistive devices for ambulation Patellar taping Appropriate footwear Lateral-wedged insoles (for genu varum).
- Bracing.
- Occupational therapy.
- Joint protection and energy conservation.
PHARMACOLOGIC TREATMENT OF OA:
- Oral Systemic Medical Agents
– Analgesics (acetaminophen)
– NSAIDs
– Opioid analgesics - Intraarticular agents:
– Hyaluronan
– Glucocorticoids (effusion) - Topical agents
INVASIVE METHODS:
- Joint lavage
- Arthroscopy
- Cartilage grafting- genetic engineering
- Surgery
– Osteotomy
– Joint replacement
Weight loss and a Balanced diet
If you are overweight, even a minor weight loss can have a significant impact on your symptoms, particularly for joints that bear weight (such as the feet, knees, hips, and back).
A healthy, balanced diet is the most effective approach to lose weight.
Reduce the amount of calories you consume from foods heavy in fat and sugar, but don’t forget to include all the major food categories in your diet to avoid deficiency in vital nutrients. You can lose weight by gradually increasing your physical activity level.
Osteoarthritis has not been shown to respond well to any particular diet. It’s advisable to evaluate if a particular meal is aggravating your symptoms by cutting it out for a few weeks and then reintroducing it. Any diet that promises to heal arthritis or that calls for eliminating a specific food group entirely should be avoided.
Certain types of arthritis, particularly rheumatoid arthritis, may have their symptoms lessened by fatty fish or oils derived from fish, according to certain research findings. However, if you’re interested in utilizing food to control osteoarthritis, you might also want to try taking a supplement or boosting your intake of fatty fish.
Steroid injections
A long-acting steroid injection can be injected straight into a joint that is causing a lot of discomfort, such as the thumb or knee. Pain relief from the injection may last for several weeks or months, and it often begins to act within a day or two. Steroid injections are mostly used to treat acute, severe pain caused by crystals in the joint or extremely painful osteoarthritis.
Glucosamine
The body naturally contains glucosamine in tissues like cartilage, ligaments, and tendons. Supplements are typically made from the shells of crabs, lobsters, or prawns, though varieties devoid of shellfish are also available. According to certain research, it might be helpful for excruciating osteoarthritis, particularly in the knee.
The majority of studies have employed a 500 mg dose three times daily, and the data appears to indicate that glucosamine sulfate may work better than glucosamine hydrochloride. Take it for a few months as it takes some time to start helping with the discomfort. It’s doubtful that it will help if, after two months, it hasn’t.
Chondroitin
Our bodies naturally contain chondroitin, which is thought to contribute to the flexibility of cartilage. The data for its potential to slow cartilage degradation is restricted to animal studies.
It will take at least two months before you notice any improvement. Additionally, it is doubtful that chondroitin can help you if your cartilage is severely injured.
Fish oils
It’s well known that fish oils and fish liver oils are beneficial for joints. Actually, there isn’t enough information to determine if fish oils are beneficial for osteoarthritis, but there is strong evidence that they can alleviate rheumatoid arthritis symptoms.
Fish liver supplements are frequently high in vitamin A, which can be hazardous in excess. Whole fish supplements are safer if you find that you need a high dose of fish oils to receive any benefit from them because they often include less vitamin A.
Alternative Treatment
Many therapies are available, and they can usually be used in conjunction with over-the-counter or prescription medications.
Here is a list of some of the most widely used therapies:
Acupuncture
By introducing tiny needles into particular body spots to address abnormalities in the flow of energy, acupuncture strives to restore the body’s natural equilibrium and promote health. There is proof that acupuncture can help with some of the osteoarthritis symptoms.
Alexander technique
You can move with less physical effort and become more conscious of your posture by using the Alexander technique. Evidence suggests that it may be useful in treating low back pain, however not osteoarthritis in particular.
Plant-based oils are utilized in aromatherapy; these oils can be burned, vaporized, ingested, or used in baths or as a component of a massage. While there is no scientific proof that aromatherapy relieves the symptoms of osteoarthritis, some people find it to be calming.
Massage
Massage has the ability to relax tense muscles, enhance muscular tone, release tight muscles, and promote blood flow. A quality massage can help you feel at ease and taken care of, but there isn’t much proof that it can effectively relieve osteoarthritis symptoms.
Osteopaths and chiropractors
Chiropractors and osteopaths use their hands to manually realign the body and exert pressure on its soft tissues. Resolving structural defects, increasing the range of motion, reducing pain, and letting the body recover itself are the goals. A small body of studies supports the effectiveness of chiropractic care for spinal osteoarthritis. On the other hand, there is currently no concrete study to support the effectiveness of osteopathy in treating osteoarthritis.
T’ai chi
Tai chi is a “mind-body” workout consisting of slow, graceful movement sequences that are intended to promote self-healing and relax the mind. Strong data suggests that t’ai chi can reduce the symptoms of osteoarthritis, especially in the knee.
FAQ
How serious is osteoarthritis?
Everybody is affected by osteoarthritis differently. Some people have very mild osteoarthritis that has no effect on their daily activities. Others experience severe pain and incapacity as a result of it. Joint deterioration often occurs gradually over years, though in certain cases, it may worsen abruptly.
What is the first treatment for osteoarthritis?
For mild osteoarthritis, acetaminophen should be the primary line of treatment. When treating osteoarthritis that ranges from moderate to severe, nonsteroidal anti-inflammatory medications are preferable than acetaminophen.
What is the best tablet for osteoarthritis?
When taken as directed, over-the-counter nonsteroidal anti-inflammatory medicines (NSAIDs) such naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, and others) usually reduce osteoarthritis pain. Prescriptions are available for stronger NSAIDs.
Can I live a normal life with osteoarthritis?
You may live a healthy, active life with osteoarthritis if you have the correct support. It’s not always the case that things become worse.
What is the final stage of osteoarthritis?
The gradual degeneration of the cartilage between a joint’s bones, which results in the bones rubbing painfully against one another when the joint is moved, is known as end-stage arthritis. Severe discomfort and a loss of function follow from this.
What is the root cause of osteoarthritis?
The cause of primary osteoarthritis is unknown. An accident, infection, malformation, or other ailment might result in secondary osteoarthritis. The deterioration of joint cartilage is the first sign of osteoarthritis. The ends of the bones may enlarge and develop bony growths (spurs) as the cartilage deteriorates.






Vary informative information