Stroke: Physiotherapy Management
What is a Stroke?
- Stroke are brain attacks. They occur when the blood supply to the brain becomes blocked. A stroke is a medical emergency that needs immediate medical treatment.
- A stroke occurs when the blood supply to part of your brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Brain cells begin to die in minutes.
- A stroke is a medical emergency, and immediate treatment is crucial. Early action can reduce brain damage and other complications.
ANATOMY OF THE BRAIN :
The three main components of the brain—the cerebrum, the cerebellum, and the brainstem—have distinct functions.
The cerebrum is the largest and most developmentally advanced part of the human brain. It is responsible for several higher functions, including higher intellectual function, speech, emotion, integration of sensory stimuli of all types, initiation of the final common pathways for movement, and fine control of movement.
The cerebellum, the second largest area, is responsible for maintaining balance and further control of movement and coordination.
The brain stem is the final pathway between cerebral structures and the spinal cord. It is responsible for a variety of automatic functions, such as control of respiration, heart rate, blood pressure, wakefulness, arousal, and attention.
The cerebrum is divided into a right and a left hemisphere and is composed of pairs of frontal, parietal, temporal, and occipital lobes.
The left hemisphere controls the majority of functions on the right side of the body, while the right hemisphere controls most of the functions on the left side of the body The crossing of nerve fibers takes place in the brain stem. Thus, injury to the left cerebral hemisphere produces sensory and motor deficits on the right side, and vice versa.
One hemisphere has a slightly more developed, or dominant, area in which written and spoken language is organized. Over 95% of right-handed people and even the majority of left-handed people have dominance for speech and language in the left hemisphere Thus, a left hemisphere stroke will be more likely to produce aphasia and other language deficits.
Layers of the Cerebrum – Gray and White Matter
Layers of the Cerebrum
The entire cerebrum is composed of two layers. The 20-millimeter thick outermost layer, called the cerebral cortex (or gray matter), contains the centers of cognition and personality and the coordination of complicated movements. As shall be seen, the gray matter is also organized for different functions.
The white matter is a network of fibers that enables regions of the brain to communicate with each other.
Cerebellum and Brainstem
A stroke involving the cerebellum may result in a lack of coordination, clumsiness, shaking, or other muscular difficulties. These are important to diagnose early, since swelling may cause brainstem compression or hydrocephalus.
Strokes in the brainstem are usually due to basilar occlusion, although in many cases the clinical syndrome may fit the criteria for a lacunar stroke. Brainstem strokes can be serious or even fatal. People who survive may be left with severe impairments or remain in a vegetative state.
DEFINITION OF STROKE :
A stroke happens when there is a loss of blood flow to part of the brain. Your brain cells cannot get the oxygen and nutrients they need from blood, and they start to die within a few minutes. This can cause lasting brain damage, long-term disability, or even death.
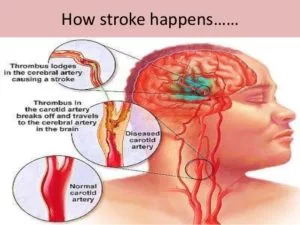
A stroke is a sudden interruption in the blood supply of the brain. Most strokes are caused by an abrupt blockage of arteries leading to the brain (ischemic stroke). Other strokes are caused by bleeding into brain tissue when a blood vessel bursts (hemorrhagic stroke).
Because stroke occurs rapidly and requires immediate treatment, stroke is also called a brain attack. When the symptoms of a stroke last only a short time (less than an hour), this is called a transient ischemic attack (TIA) or mini-stroke.
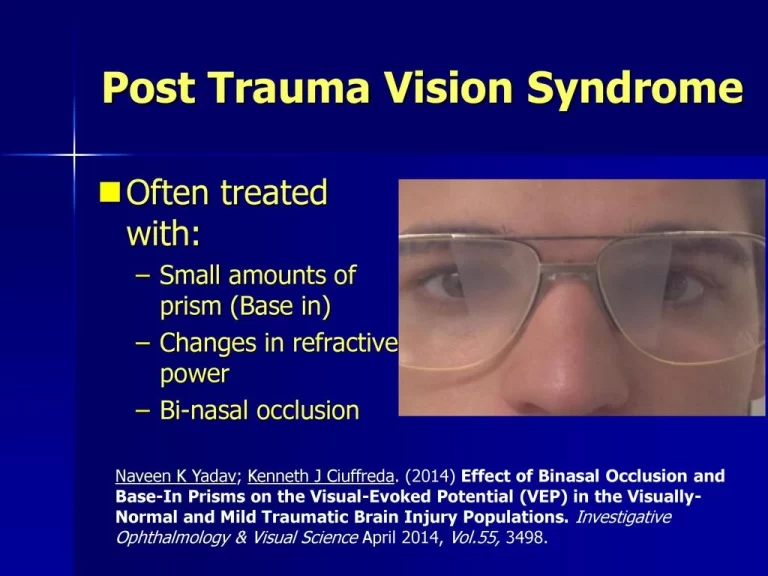
The effects of a stroke depend on which part of the brain is injured, and how severely it is injured. Strokes may cause sudden weakness, loss of sensation, or difficulty with speaking, seeing, or walking. Since different parts of the brain control different areas and functions, it is usually the area immediately surrounding the stroke that is affected. Sometimes people with stroke have a headache, but stroke can also be completely painless. It is very important to recognize the warning signs of stroke and to get immediate medical attention if they occur.
Motor deficits are characterized by paralysis (hemiplegia) or weakness (hemiparesis), typically on the side of the body opposite the side of the lesion.
CLASSIFICATION OF STROKE :
Strokes are classified by etiological categories(thrombosis, embolus, or hemorrhage), specific vascularterritory (anterior cerebral artery syndrome, middle cerebral artery syndrome, and so forth), and management categories (transient ischemic attack, minor stroke, major stroke, deteriorating stroke, young stroke).
- Main three types of stroke:
- Ischemic stroke.
- Hemorrhagic stroke.
- Transient ischemic attack (a warning or “mini-stroke”).
There are two types of hemorrhagic strokes:
- Intracerebral hemorrhage is the most common type of hemorrhagic stroke. It occurs when an artery in the brain bursts, flooding the surrounding tissue with blood.
- Subarachnoid hemorrhage is a less common type of hemorrhagic stroke. It refers to bleeding in the area between the brain and the thin tissues that cover it.
ISCHEMIC STROKE :
NORMAL PHYSIOLOGY: The brain depends on its arteries to bring fresh blood from the heart and lungs. The blood carries oxygen and nutrients to the brain, and takes away carbon dioxide and cellular waste.
PATHOLOGY: If an artery is blocked, the brain cells (neurons) cannot make enough energy and will eventually stop working. If the artery remains blocked for more than a few minutes, the brain cells may die. This is why immediate medical treatment is critical.
Ischemic stroke is by far the most common kind of stroke, accounting for about 88 percent of all strokes.
Types of Ischemic Stroke :
Ischemic stroke can be divided into two main types: thrombotic and embolic.
THROMBOTIC STROKE: A thrombotic stroke occurs when diseased or damaged cerebral arteries become blocked by the formation of a blood clot within the brain. Clinically referred to as cerebral thrombosis or cerebral infarction, this type of event is responsible for almost 50 percent of all strokes.
Cerebral thrombosis can also be divided into additional two categories that correlate to the location of the blockage within the brain: large-vessel thrombosis and small-vessel thrombosis.
Large-vessel thrombosis is the term used when the blockage is in one of the brain’s larger blood-supplying arteries such as the carotid or middle cerebral, while small-vessel thrombosis involves one (or more) of the brain’s smaller, yet deeper, penetrating arteries. This latter type of stroke is also called a lacuner stroke.
EMBOLIC STROKE: An embolic stroke is also caused by a clot within an artery, but in this case, the clot (or emboli) forms somewhere other than in the brain itself. Often from the heart, these emboli will travel in the bloodstream until they become lodged and cannot travel any farther. This naturally restricts the flow of blood to the brain and results in near-immediate physical and neurological deficits.
Causes of Ischemic Stroke :
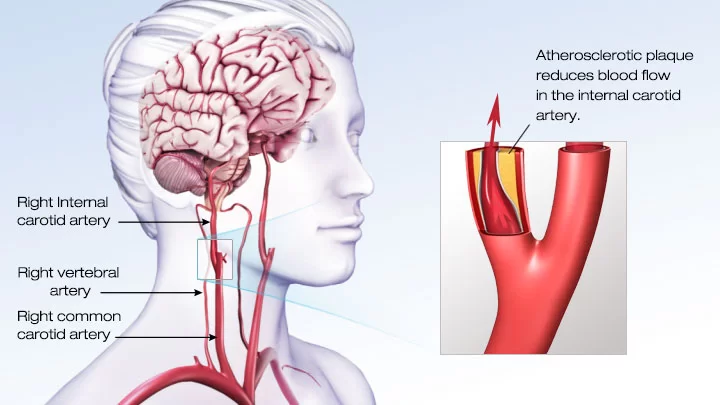
Ischemic stroke can be caused by several different kinds of diseases. The most common problem is the narrowing of the arteries in the neck or head. This is most often caused by atherosclerosis, or gradual cholesterol deposition.
If the arteries become too narrow, blood cells may collect and form blood clots. These blood clots can block the artery where they are formed (thrombosis), or can dislodge and become trapped in arteries closer to the brain (embolism).
Another cause of stroke is blood clots in the heart, which can occur as a result of irregular heartbeat (for example, atrial fibrillation), heart attack, or abnormalities of the heart valves.
While these are the most common causes of ischemic stroke, there are many other possible causes. Examples include the use of street drugs, traumatic injury to the blood vessels of the neck, or disorders of blood clotting.
HEMORRHAGIC STROKE :
Intracerebral Hemorrhage :
Intracerebral hemorrhage occurs when a diseased blood vessel within the brain bursts, allowing blood to leak inside the brain. (The name means within the cerebrum or brain).
The sudden increase in pressure within the brain can cause damage to the brain cells surrounding the blood. If the amount of blood increases rapidly, the sudden buildup in pressure can lead to unconsciousness or death. Intracerebral hemorrhage usually occurs in selected parts of the brain, including the basal ganglia, cerebellum, brain stem, or cortex.
Causes of intracerebral hemorrhage :
The most common cause of intracerebral hemorrhage is high blood pressure (hypertension). Since high blood pressure by itself often causes no symptoms, many people with intracranial hemorrhage are not aware that they have high blood pressure, or that it needs to be treated. Less common causes of intracerebral hemorrhage include trauma, infections, tumors, blood clotting deficiencies, and abnormalities in blood vessels (such as arteriovenous malformations).
Intracerebral Hemorrhage – Coronal Edema
A ruptured blood vessel will leak blood into the brain, eventually causing the brain to compress due to the added amount of fluid.
Intracerebral hemorrhage occurs at all ages. The average age is lower than for ischemic stroke. Less common than ischemic strokes, hemorrhagic strokes make up about 12 percent of all strokes.
Sub-arachnoid Hemorrhage:
Subarachnoid hemorrhage occurs when a blood vessel just outside the brain ruptures.
The area of the skull surrounding the brain (the subarachnoid space) rapidly fills with blood.
A patient with subarachnoid hemorrhage may have a sudden, intense headache, neck pain, and nausea or vomiting. Sometimes this is described as the worst headache of one’s life.
The sudden buildup of pressure outside the brain may also cause rapid loss of consciousness or death.
Causes of Subarachnoid hemorrhage :
Subarachnoid hemorrhage is most often occured by abnormalities of the arteries at the base of the brain, called cerebral aneurysms. These are small areas of rounded or irregular swellings in the arteries. Where the swelling is most severe, the blood vessel wall becomes weak and prone to rupture.
The cause of cerebral aneurysms is not known. They may develop from birth or in childhood and grow very slowly. Some people have multiple aneuryms.
Subarachnoid hemorrhage can occur at any age, including in teenagers and young adults, and is slightly more common in women than men.
TIA (Transient Ischemic Attack) :
A transient ischemic attack (TIA) is sometimes called a “mini-stroke.” It is different from the major types of stroke because blood flow to the brain is blocked for only a short time—usually no more than 5 minutes.
A TIA is a warning sign of a future stroke.
There is no way to know in the beginning whether symptoms are from a TIA or from a major type of stroke.
Like ischemic strokes, blood clots often cause TIAs.
TIAs may result from a number of different etiological factors including
occlusive episodes, emboli, reduced cerebral perfusion (arrhythmias, decreased cardiac output, hypotension, overmedication with antihypertensive medications, subclavian steal syndrome), or cerebrovascular spasm. The major clinical significance of TIA is as a precursor to susceptibility for both cerebral infarction and myocardial infarction.
Epidemiology :
- Stroke is the third leading cause of death and the most common cause of disability among adults in the United States.
- The incidence of stroke is about 1.25 times greater for males than females. Compared to whites, African-Americans have twice the risk of first-ever stroke; rates are also higher in Mexican-Americans, American
- Indians, and Alaska Natives.
- The incidence of stroke increases dramatically with age, doubling in the decade after 65 years of age.
Warning Signs of stroke :
- The most common sign of stroke is sudden weakness of the face, arm or leg, most often on one side of the body.
- Other warning signs can include:
- Sudden numbness of the arm, or leg, especially on one side of the body
- Sudden confusion, trouble speaking or understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance or coordination, instability, paralysis with weak muscles, stiff muscles, overactive reflexes
- Sudden severe headache with no known cause
- Facial: muscle weakness or numbness
- Also common: difficulty swallowing, inability to understand, mental confusion, or rapid involuntary eye movement
- The signs of a stroke depend on the side of the brain that’s affected, the part of the brain affected, and how severely the brain is injured. Therefore, each person may have different stroke warning signs.
Risk Factors for Stroke:
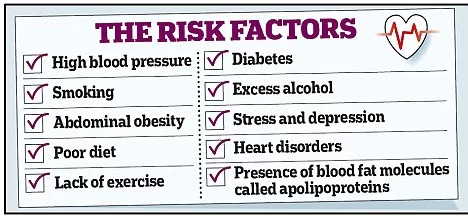
Cardiovascular diseases affecting the brain and heart share a number of common risk factors important to the development of atherosclerosis. Major risk factors for stroke are hypertension, heart disease, and diabetes.
Controllable risk factors and lifestyle choices:
- Smoking.
- Tobacco use is a major preventable risk factor for stroke and heart disease. Even if you have smoked for years, you can still reduce your risk by quitting now.
- Need help quitting? The Freedom From Smoking® plan is free and available online at the American Lung Association.
- Obesity, elevated cholesterol, and elevated lipids.
- Reducing your dietary intake of saturated fats and cholesterol may help reduce your risk of a stroke.
- Physical inactivity.
- A sedentary lifestyle void of regular exercise can contribute to heart disease which may lead to stroke.
- Excessive alcohol intake.
- Illegal drug use.
Uncontrollable risk factors:
- Increasing age.
- Stroke is more common in people over 60.
- Male sex. Men and women both have strokes but stroke is more common at younger ages in men.
- Heredity and ethnicity.
- Stroke is more common in people whose close relatives have had stroke at an early age.
How Are Strokes Diagnosed?
Head CT: One of the most common tests doctors use is a head CT, which is a special type of X-ray that takes a picture of the brain. A patient getting a head CT just has to lie still for a few seconds while the CT scanner takes a picture of the brain. A head CT does not hurt and does not take a long time to perform.
MRI: Another test is magnetic resonance imaging (MRI), which takes a picture of the brain without using X-rays. An MRI takes much more detailed pictures than a CT, and it is a much slower test. it is a painless procedure.
DOPPLER: If doctors need to take a closer look at the arteries that feed the brain, there are several tests they can use. A transcranial Doppler uses ultrasound waves, or sound waves we can’t hear, to look at the blood flowing through the arteries in the brain. For this test, a doctor holds a small ultrasound machine up against a patient’s head for a few minutes in order to take a picture of the arteries in the brain. A transcranial Doppler is not noisy and does not hurt. An angiogram is a test that uses X-rays to take more detailed pictures of the arteries in the neck and head.
The next step is a thorough physical examination. Pulse and blood pressure will be checked, and examine the rest of your body (heart, lungs, etc). The neurologic examination includes detailed tests of your muscles and nerves. The doctor will check your strength, sensation, coordination and reflexes. In addition, you will be asked questions to check your memory, speech and thinking.
Prognosis in Stroke:
- Although stroke is a disease of the brain, it can affect the entire body.
- A common disability that results from stroke is complete paralysis on one side of the body, called hemiplegia. A related disability that is not as debilitating as paralysis is one-sided weakness or hemiparesis.
- Stroke may cause problems with thinking, awareness, attention, learning, judgment, and memory.
- Stroke survivors often have problems understanding or forming speech. A stroke can lead to emotional problems. Stroke patients may have difficulty controlling their emotions or may express inappropriate emotions. Many stroke patients experience depression. Stroke survivors may also have numbness or strange sensations.
- The pain is often worse in the hands and feet and is made worse by movement and temperature changes, especially cold temperatures.
- Recurrent stroke is frequent; about 25 percent of people who recover from their first stroke will have another stroke within 5 years.
Complications of Stroke :
- Musculoskeletal: weakness of upper and lower limbs.
- Cardiovascular/ pulmonary: DVT and thrombophebitis
- Neurological: seizures and hydrocephalus
- Respiratory problems
Role of Physiotherapy in Stroke :
- Stroke often causes paralysis on one side of the body, which means patients lose function in one arm and one leg. In the first weeks and months of recovery, physical therapists work with stroke survivors to keep these muscles toned and stimulated – even before they regain voluntary movement.
- If and when a function does return, physical therapy allows patients to relearn everyday skills and retrain their healthy brain cells to control the affected body parts. This also includes occupational rehabilitation and speech therapy.
- Post-stroke rehabilitation is a huge part of this recovery process, and it often begins as early as 24 hours after a stroke. Stroke physical therapists are able to stimulate affected muscles and nerves to maintain circulation and prevent stiffness.
Treatment for Stroke :
Unfortunately, stroke cannot be cured. The brain cannot heal itself the same way the rest of the body does. If a tiny part of the brain is injured by a stroke, that tiny part of the brain will never “grow back” or be the same as it was before the stroke happened.
Fortunately, the brain has other ways of responding to an injury. If a small part of the brain is permanently injured and cannot do its job anymore, other parts of the brain often “pitch in” and take over the job the injured part of the brain used to do. Retraining parts of the brain to do different jobs is slow, difficult work.
Physiotherapy enables people to relearn lost abilities, regain independence and reduce the risk of further strokes.
Physiotherapy improves recovery of function and mobility after stroke.
Rehabilitation should continue for as long as the person is showing measurable benefit from treatment and has achieved their agreed goals.
Most people who have a stroke already have other long-term conditions. This makes long-term management complex.
What are the treatments for stroke?
Treatments for stroke include medicines, surgery, and rehabilitation. Which treatments you get depends on the type of stroke and the stage of treatment. The different stages are :
- Acute treatment, is to try to stop a stroke while it is happening.
- Post-stroke rehabilitation, to overcome the disabilities caused by the stroke.
- Prevention, is to prevent a first stroke or, if you have already had one, prevent another stroke.
Stroke rehabilitation can help you relearn skills you lost because of the damage. The goal is to help you become as independent as possible and to have the best possible quality of life.
Neurorehabilitation includes many different therapies, such as physical or speech therapy, that are selected to treat individual symptoms.
Physiotherapy treatment for Stroke :
Early Mobilisation: Immobility is associated with a number of post stroke complications such as deep vein thrombosis etc. Early mobilization aims to reduce the time that elapses between stroke and the first time the patient leaves the bed, increasing the amount of physical activity that the patient engages in outside of bed. Early mobilisation (e.g. activities such as sitting out of bed, transfers, standing and walking) aims to minimise the risk of the complications of immobility and improve functional recovery.
Strategies to Improve Sensory Function: The presentation of repeated sensory stimuli stimulates tactile, mechano and muscle receptors. For example, stroking, stretching, superficial and deep pressure, and approximation can be used. The selection of sensory inputs should be direct.
stroking the hand with different textured fabrics, pressing objects into the hand (coin, button, key), or drawing shapes/letters/numbers on the skin. During functional training, approximation can be provided to extended UE
during weightbearing (e.g., in sitting or standing/modified plantigrade position). Approximation can be added to LE tasks such as standing and stepping. Stimulation should be of sufficient intensity to engage the system but not so strong as to produce adverse effects (e.g., withdrawal). During
stimulation, the patient’s attention should be focused directly on the stimulation and task.
Initial attempts are witheyes closed (EC). If the patient fails to recognize the stimulus, the patient can be allowed to look with eyes open (EO).
Strategies to Improve Motor Function: Soft tissue/joint mobilization and ROM exercises are initiated early to maintain joint integrity and mobility and prevent contractures. AROM and passive ROM (PROM) with terminal stretch should be performed daily in all motions.
If a contracture is developing, more frequent ROM (twice daily or more) is necessary and sustained low-load stretching can be considered.
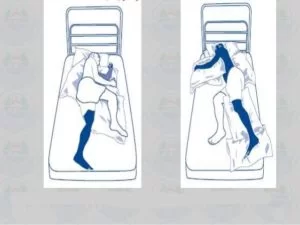
Positioning strategies are also important in maintaining
soft tissue length.
Arm cradling: The more affected UE cradles and lifts the less affected UE to 90°; the arm is moved into positions of horizontal abduction and adduction. Active trunk rotation is combined with arm movements.
Table-top polishing: The affected extremity is positioned in humeral flexion with scapular protraction and elbow extension; both hands are positioned on a towel. The less affected hand moves the paretic hand by pulling on the towel (forward, and side-to-side). Trunk movements and ROM are optimized by placing the chair slightly back from the table.
Sitting, the patient leans forward and reaches both hands down to the floor. This position encourages forward flexion of the humerus with scapular protraction, and extension of the elbow, wrist, and fingers.
Tabletop arm exercise :
Supine, hands are clasped together and placed behind the head, the elbows fall flat to the mat. This activity should be considered only if scapula upward mobility is present.
Hands clasped, self-overhead movements are contraindicated
if scapulohumeral rhythm is lacking.
Strategies to Improve Strength :
- Exercise modalities for strengthening include free weights, elastic bands or tubing, and machines (PRE, isokinetics).
- For patients who are very weak (3/5), gravity-eliminatedexercises using powder boards, sling suspension, or aquatic exercise is indicated. The therapist may need to assist initial movement attempts using active-assisted or facilitated movements (stretch and tracking resistance).
- Gravity-resisted active movements are indicated for patients who demonstrate 3/5 strength (e.g., arm lifts, leg lifts). Patients who demonstrate adequate strength in gravity-resisted exercise (e.g., 8 to 12 reps) can be progressed to exercise using added resistance (e.g., free weights, bands, or machines).
- Combining resistance training with functional activities provides additional benefits in terms of improving function (e.g., step-ups or stair climbing while the patient is wearing weighted ankle cuffs). Lifting free weights or using elastic bands places added demands for postural stability and is an important element of training to improve postural control.
Mirror Therapy for upper limb: Mirror Therapy may be used as an adjunct to routine therapy to improve arm function after stroke for individuals with mild to moderate weakness, complex regional pain syndrome, and/or neglect.
Strategies to Manage Spasticity :
- Patients who demonstrate spasticity benefit from interventions designed to modify or reduce tone.
- These include early mobilization combined with elongation of spastic muscles and sustained stretch through positioning. The technique of rhythmic rotation (a passive manual technique) can be effective in gaining initial range.
- Once the full range is achieved, the limb is positioned in the lengthened position.
- For example, the shoulder is extended, abducted, and externally rotated with the elbow, wrist, and fingers extended and positioned in weight-bearing (4-point kneeling).
- Types of Stretch : (1) Fast / Quick, (2) Prolonged and Maintained.
Strategies to Improve Postural Control and Functional Mobility :
- Rolling
- Supine-to-Sit and Sit-to-Supine
- Sitting
- Bridging
- Standing
- Standing, Modified Plantigrade
- Transfers
Supine to sit transfer activity in stroke :
Positioning: Therapeutic positioning aims to reduce skin damage, limb swelling, shoulder pain or subluxation, and discomfort, and maximise function and maintain soft tissue length. It is also suggested that positioning may assist in reduction of respiratory complications such as those caused by aspiration and avoid compromising hydration and nutrition. The aim of positioning the patient is to try to promote optimal recovery and comfort by modulating muscle tone, providing appropriate sensory information, increasing spatial awareness, improved ability to interact with the environment and prevention of complications such as pressure sores, and contracture.

Balance: Balance difficulties are commone for many individuals post stroke usually due to a combination of reduced limb and trunk motor control, altered sensation and sometimes centrally determined alteration in body representation such that the person misperceives their posture in relation to the upright. Impaired balance often leads to reduced confidence, fear of falling and increases the risk of falls.
sitting and standing balance. Practice of standing balance should be provided for individuals who have difficulty with standing. Strategies could include:
- Practising functional task-specific training while standing
- Walking training that includes challenge to standing balance (e.g.overground walking, obstacle courses)
- Providing visual or auditory feedback
- Receive progressive balance training
- Receive lower limb strengthening exercises
- Consider for an ankle-foot orthosis
Gait & Mobility: The highest priority for many people with limited mobility after stroke is to walk independently. Individuals post stroke benefit from time spent in task-specific, walking-orientated leg exercises which have a cardiorespiratory focus both early and late after stroke. Interventions should be of a sufficient intensity with a focus on progression, task-specificity and challenge to improve outcomes and can include strengthening exercises for the leg, over-ground walking, circuit classes and treadmill training with and without body weight support. If walking performance is poor after stroke, community activity may be limited and people may become housebound and isolated from society.
Repetitive practice of walking (or components of walking) should be practiced as often as possible for individuals with difficulty walking.
- Treadmill Training with or without body weight support
- Virtual Reality Training
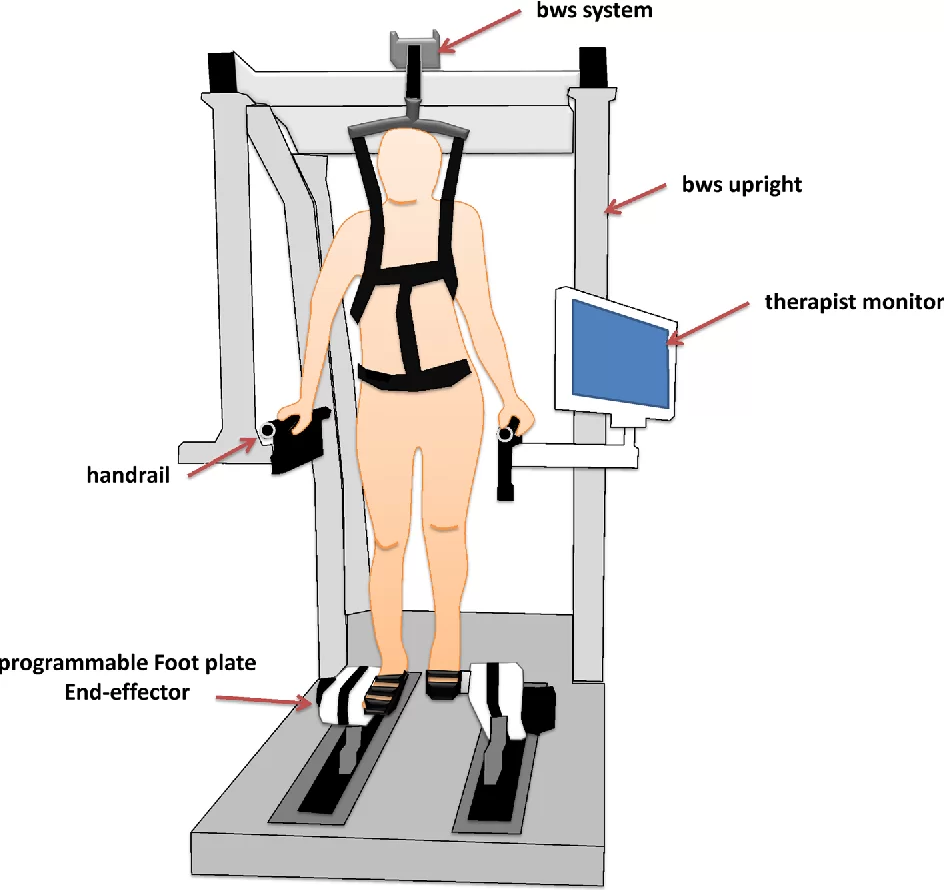
- Electromechanically Assisted Gait Training
- Biofeedback
- Functional Electrical Stimulation
Treadmill Training: Treadmill training can be utilised for both Gait Re-education / Training but also to aid improvements in aerobic function. Treadmill training can be completed with the patient’s body-weight partially supported by a harness in order to grade the amount of body weight supported, which is used for individuals with significant functional limitations. Speed dependent treadmill training without a harness may also be utilised. Therapists facilitate alternating stepping and weight-bearing, and as many as more than one therapists may be required to assist with the complete gait cycle.
- It allows a complete practice of the gait cycle.
- It provides opportunity for gaining improvements in speed and endurance.
- It optimizes aerobic fitness.
People who are able to walk independently after stroke should be offered treadmill training with or without body weight support or other walking-orientated interventions at a higher intensity than usual care.
Electromechanical Assisted: Electromechanical-assisted gait training, with and without partial body weight support, are used as adjuncts to overground gait training for the rehabilitation of patients after stroke and can be used to give non-ambulatory patients intensive practice (in terms of high repetitions) of complex gait cycles. Automated electromechanical gait machines consist either of a robot-driven exoskeleton orthosis or an electromechanical solution with two driven foot-plates simulating the phases of gait aand offer reduced effort for therapists, as they no longer need to set the paretic limbs or assist trunk movements. The main difference between electromechanical-assisted and treadmill training is that the process of gait training is automated and supported by an electromechanical solution. Repetitive gait training in combination with physiotherapy may improve walking ability in patients after stroke.
People who cannot walk independently after stroke should be considered for electromechanical-assisted gait training including body weight support.
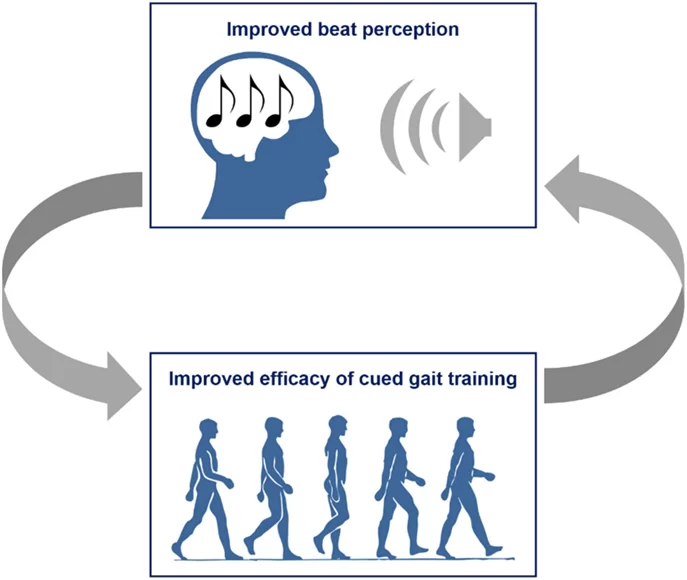
Rhythmic Cueing: Motor Control research provides considerable evidence that auditory rhythm can improve timing and variability of motor responses, specifically, in motor tasks with complex timing requirements or in disorders affecting timing of movement, external rhythm can provide additional stability to timekeeper mechanisms in the brain.
For Rhythmic Cueing the patient’s steps are matched to the beat of the metronome or specially prepared music in order to synchronise motor responses into stable time relationships. The patient is asked to take steps according to the beat, so the rhythmic beat acts as a cue. If the beats are of a consistent frequency, this cueing will promote the temporal symmetry of walking. If the frequency of these consistent beats is increased, cadence and, therefore, speed will also increase.The goal is to influence gait parameters such as pace frequency, stride length and hence walking speed and symmetry.
Systematic review provides evidence that gait training with cueing of cadence is more effective than gait training alone in improving walking after stroke.
Virtual Reality: Advances in virtual reality technology mean that devices using computer and gaming technology are now found in many people’s homes. The potential of these types of adjuncts to maximize task-orientated practice and increase energy expenditure are beginning to be explored. Virtual reality mobility training involves the use of computer technology which enables the patient to move about in a virtual environment and receive feedback on their performance and is suggested that the use of a virtual environment produces cortical reorganization. Furthermore, virtual environments are adaptable and can afford patients the opportunity to practice under a variety of simulated circumstances.

The difficulty level of the training scenarios can be adjusted by varying the speed and slope of the treadmill, the complexity of tasks, and the amount of body weight support and can allow immediate patient feedback on performance, which is an important component of learning. It might be costly to use for an individual.
Overground Walking: Overground waliking involves walking and walking-related activities on a solid surface, where the physiotherapist observes the patient’s gait, usually on a level surface, and has the patient do a range of differnt activities and exercises to influence their gait. The benefit is that over- ground gait training can be used in almost any setting or location without requiring a great deal of high-tech equipment.
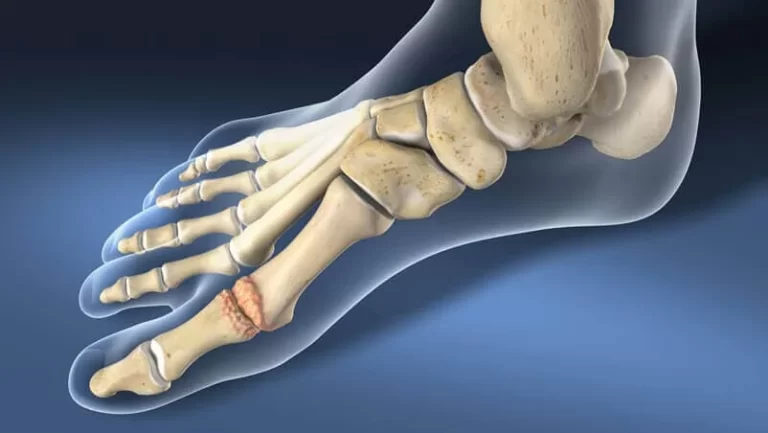
Orthotics: Orthotics, like any tool used in the treatment of a complex and chronic condition, can target all levels of health at once. It may be an intervention designed to change body structures, or an intervention to support and stabilize unresponsive muscles so an activity can be performed, or an adjunct to enable participation in a life role such as work. This helps in :
- Relief of Pain
- Immobilization of Musculoskeletal Segments
- Reduced Axial Loading
- Prevention or Correction of Deformity
- Improved Function

Orthoses are made from various types of materials including thermoplastics, carbon fibre, metals, elastic, EVA, fabric or a combination of similar materials. Some designs may be purchased at a local retailer; others are more specific and require a prescription from a physician, who will fit the orthosis according to the patient’s requirements. Over-the-counter braces are basic and available in multiple sizes. They are generally slid on or strapped on with Velcro, and are held tightly in place. Individually fitted lower limb orthoses may be used to minimises limitations in walking ability. Individually fitted lower limb orthoses may be used to minimises limitations in walking ability.
Strategies to Improve Aerobic Function :
Cardiorespiratory Training : There is an increasing range of aerobic exercise options being accessed by people with following Stroke. These range from aerobic exercise programmes (e.g. overground walking or treadmill training programmes) and an array of sporting and exercise classes to the use of technology (e.g. virtual reality training).
Hydrotherapy: Immersion in water can enhance the treatment of neurologically impaired individuals with both therapeutic, physchological and social benefits. Hydrotherapy is the term used for exercise in warm water and is a popular treatment for patients with neurologic and musculoskeletal conditions and is defined by the Hydrotherapy Association of Chartered Physiotherapists Guidance on Good Practice in Hydrotherapy as a therapy programme using the properties of water, designed by a suitably qualified physiotherapist, to improve function, ideally in a purpose-built and suitably heated hydrotherapy pool .
Contracture Management: A muscle contracture is a permanent shortening of a muscle or joint. It is usually in response to prolonged hypertonic spasticity in a concentrated muscle area. Contractures are not uncommon in limbs affected by spasticity. Contractures can impede activities such as washing or putting on clothes, and may also be uncomfortable or painful and limit the ability to sit in a wheelchair or mobilise.A Systematic Review to determine whether stretch increases joint mobility in people with existing contractures or those at risk of developing contractures provides moderate to high quality evidence that stretch, whether passive or through the means of splint or seriel casting, does not have a clinically important effect on joint mobility in people with neurological conditions.
Fatigue Management : Fatigue is common complaint post-stroke, and is evident even in those individuals who have made an otherwise complete recovery. Over 40% of long-term stroke survivors report ongoing issues with fatigue which impact on their daily living activities with lack of energy and/or an increased need to rest every day, as the main characteristics which can be brought on by both mental and physical activity. Fatigue has also been associated with depression, and may be a predictor of shorter survival. Management strategies include the identification of triggers and re-energisers, environmental modifications and lifestyle changes, scheduling and pacing, cognitive strategies to reduce mental effort, and psychological support to address mood, stress and adjustment.




52 Comments