Osteoporosis
Introduction
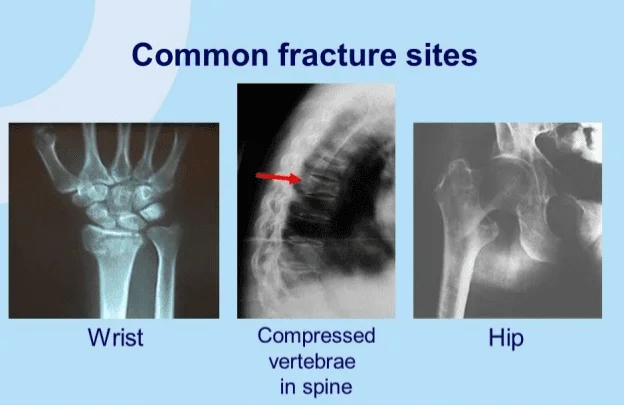
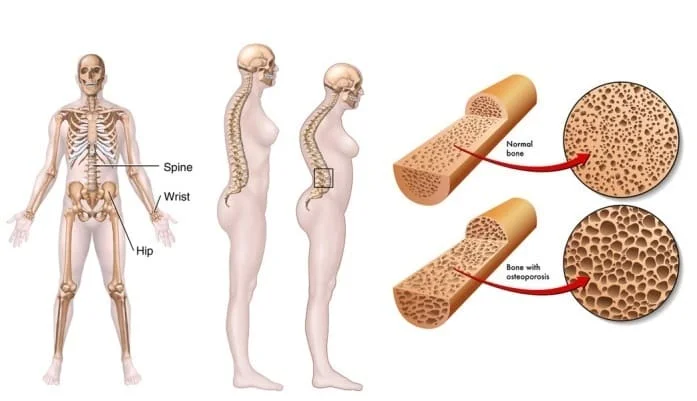
Osteoporosis causes bones to become weak and brittle — so brittle that a fall or even mild stresses such as bending over or coughing can cause a fracture. Osteoporosis-related fractures most commonly occur in the hip, wrist, or spine.
Bone is living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn’t keep up with the loss of old bone.
Osteoporosis affects men and women of all races. But white and Asian women — especially older women who are past menopause — are at highest risk. Medications, a healthy diet, and weight-bearing exercise can help prevent bone loss or strengthen already weak bones.
In people with osteoporosis, the bones become porous and weaker, increasing the risk of fractures, especially in the hip, spinal vertebrae, and some peripheral joints, such as the wrists.
The International Osteoporosis Foundation (IOF) estimates that over 44 million people in the United States currently have osteoporosis.
Defination
Osteoporosis is a bone disease that occurs when the body loses too much bone, makes too little bone, or both. As a result, bones become weak and may break from a fall or, in serious cases, from sneezing or minor bumps. Osteoporosis means “porous bone.”
Signs and Symptoms
There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include.
- Back pain, caused by a fractured or collapsed vertebra
- Loss of height over time
- A stooped posture
- A bone that breaks much more easily than expected
- receding gums
- weakened grip strength
- weak and brittle nail
Osteoporosis develops slowly, and a person may not know they have it until they experience a fracture or break after a minor incident, such as a fall. Even a cough or sneeze can cause a break in osteoporotic bones.
Breaks will often occur in the hip, wrists, or spinal vertebrae for people who have osteoporosis.
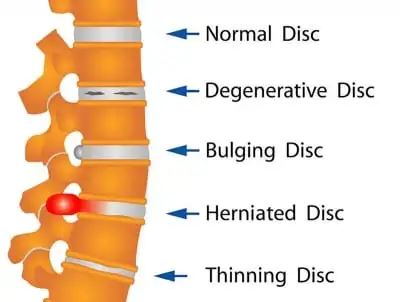
If a break occurs in the spinal vertebrae, it can lead to changes in posture, a stoop, and curvature of the spine.
People might also notice a decrease in height or their clothes may not fit as well as they did previously.
Back or neck pain or loss of height can be caused by a compression fracture. This is a break in one of the vertebrae in your neck or back, which is so weak that it breaks under the normal pressure in your spine.
There is an increased risk of falls associated with aging.
Part of the fall risk is because of impaired eyesight due to many causes, (e.g. glaucoma, macular degeneration), balance disorder, movement disorders (e.g. Parkinson’s disease), dementia, and sarcopenia (age-related loss of skeletal muscle).
If you don’t have symptoms but have a family history of osteoporosis, talking to your doctor can help you assess your risk.
Risk factors
Age:
The biggest risk factor of osteoporosis is age. Throughout your life, your body breaks down old bone and grows new bone.
However, when you’re in your 30s, your body starts breaking down bone faster than it’s able to replace it. This leads to bone that’s less dense and more fragile, and thus more prone to breakage.
Menopause:
Menopause is another primary risk factor, which occurs in women around the ages of 45 to 55 years. Due to the change in hormone levels associated with it, menopause can cause a woman’s body to lose bone even more quickly.
Men continue to lose bone at this age, but at a slower rate than women do. However, by the time they reach the ages of 65 to 70, women and men are usually losing bone at the same rate.
Other risk factors for osteoporosis include:
- being female
- being Caucasian or Asian
- having a family history of osteoporosis
- Poor nutrition
- physical inactivity
- smoking
- low body weight
- small-boned frame
You can control some of these risk factors for osteoporosis, such as poor nutrition and inactivity. For instance, you can improve your diet, and starting an exercise program can benefit your bone health. However, you can’t control other risk factors, such as your age or gender.
Cigarette smoking, eating disorders such as anorexia nervosa or bulimia, low amounts of calcium in the diet, heavy alcohol consumption, inactive lifestyle, and use of certain medications, such as corticosteroids and anticonvulsants, are also risk factors.

Thyroid problems:
Too much thyroid hormone can cause bone loss. This can occur if your thyroid is overactive or if you take too much thyroid hormone medication to treat an underactive thyroid.
Rheumatoid arthritis itself is a risk factor for osteoporosis.
Causes
Osteoporosis occurs when there is an imbalance between new bone formation and old bone resorption. The body may fail to form enough new bone, or too much old bone may be reabsorbed, or both.
If calcium intake is not sufficient or if the body does not absorb enough calcium from the diet, bone production, and bone tissue may suffer. Thus, the bones may become weaker, resulting in fragile and brittle bones that can break easily.
The leading cause of osteoporosis is a lack of certain hormones, particularly estrogen in women and androgen in men.
Women, especially those older than 60 years of age, are frequently diagnosed with the disease. Menopause is accompanied by lower estrogen levels and increases a woman’s risk for osteoporosis.
Other conditions that may lead to osteoporosis include overuse of corticosteroids (Cushing syndrome), thyroid problems, lack of muscle use, bone cancer, certain genetic disorders, use of certain medications, and problems such as low calcium in the diet.
Diagnosis
Your bone density can be measured by a machine that uses low levels of X-rays to determine the proportion of minerals in your bones. During this painless test, you lie on a padded table as a scanner passes over your body. In most cases, only a few bones are checked — usually in the hip and spine.
The diagnosis of osteoporosis can be made using conventional radiography and by measuring the bone mineral density (BMD). The most popular method of measuring BMD is dual-energy X-ray absorptiometry.
Conventional radiography is useful, both by itself and in conjunction with CT or MRI, for detecting complications of osteopenia (reduced bone mass; pre-osteoporosis), such as fractures; and for differential diagnosis of osteopenia. Radiography is relatively insensitive to the detection of early disease and requires a substantial amount of bone loss (about 30%) to be apparent on X-ray images.
The main radiographic features of generalized osteoporosis are cortical thinning and increased radiolucency. Frequent complications of osteoporosis are vertebral fractures for which spinal radiography can help considerably in diagnosis and follow-up. Vertebral height measurements can objectively be made using plain-film X-rays by using several methods such as height loss together with area reduction, particularly when looking at vertical deformity in T4-L4, or by determining a spinal fracture index that takes into account the number of vertebrae involved. Involvement of multiple vertebral bodies leads to kyphosis of the thoracic spine, leading to what is known as the dowager’s hump.
Dual-energy X-ray:
Dual-energy X-ray absorptiometry (DEXA scan) is considered the gold standard for the diagnosis of osteoporosis. Osteoporosis is diagnosed when the bone mineral density is less than or equal to 2.5 standard deviations below that of a young (30–40-year-old).Because bone density decreases with age, more people become osteoporotic with increasing age.
Biomarkers:
Chemical biomarkers are a useful tool in detecting bone degradation.
Other measuring tools:
Quantitative ultrasound has many advantages in assessing osteoporosis.
Differential Diagnosis
- Osteomalacia/ Rickets
- Bone Infection
- Pediatric osteogenesis imperfecta
- Cancer: Fractures caused by little or no force often occur due to osteoporosis, but may also be the result of bone cancer or metastatic cancer.
- Multiple Myeloma
- Renal osteodystrophy
- Scurvy: Vitamin C deficiency
- Management:
Lifestyle:
Weight-bearing endurance exercise and/or exercises to strengthen muscles improve bone strength in those with osteoporosis. Aerobics, weight-bearing, and resistance exercises all maintain or increase BMD in postmenopausal women. Fall prevention can help prevent osteoporosis complications. There is some evidence for hip protectors specifically among those who are in care homes.
Avoiding smoking, as this can reduce the growth of new bone and decrease estrogen levels in women
Limiting alcohol intake to encourage healthy bones and prevent falls
Getting regular weight-bearing exercise, such as walking, this promotes healthy bones and strengthens their support from muscles
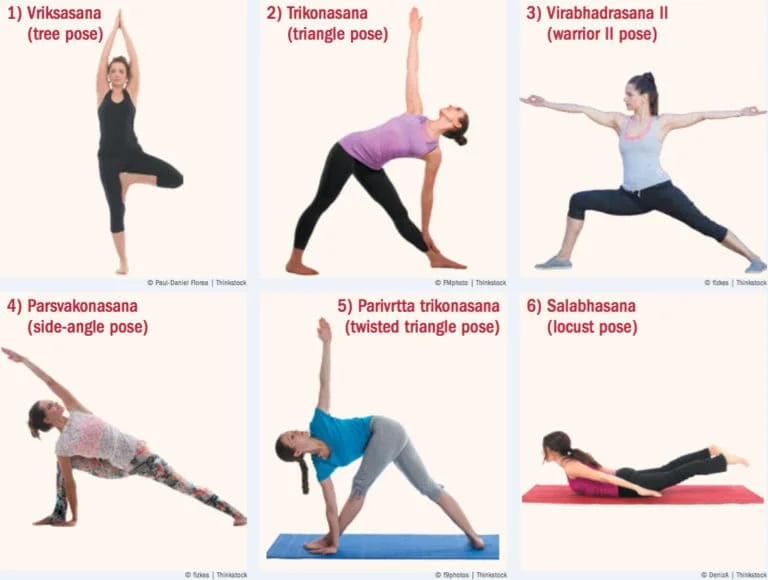
Exercises to promote flexibility and balance, such as yoga, which can reduce the risk of falls and fractures
Medications:
Bisphosphonates are useful in decreasing the risk of future fractures in those who have already sustained a fracture due to osteoporosis.
For both men and women at increased risk of fracture, the most widely prescribed osteoporosis medications are bisphosphonates.
Examples include:
- Alendronate (Binosto, Fosamax)
- Risedronate (Actonel, Atelvia)
- Ibandronate (Boniva)
- Zoledronic acid (Reclast, Zometa)
Side effects include nausea, abdominal pain, and heartburn-like symptoms. These are less likely to occur if the medicine is taken properly.
Prevention
Certain alterations to lifestyle can reduce the risk of osteoporosis.
Calcium and vitamin D intake:
Calcium is essential for bones. People should make sure they consume enough calcium daily.
Adults aged 19 years and above should consume 1,000 milligrams (mg) of calcium a day. Women who are over 51 years of age and all adults from 71 years onward should have a daily intake of 1,200 mg.
Dietary sources include:
- dairy foods, such as milk, cheese, and yogurt
- green leafy vegetables, such as kale and broccoli
- fish with soft bones, such as tinned salmon and tuna
- fortified breakfast cereals
Physiotherapy Treatment
Physiotherapy exercises can help you strengthen your bones, as well as your muscles. It can prevent bone thinning, reduce falls, and help you manage any pain.
Bone is a living tissue that can be improved through some types of exercise. A physiotherapist can work with you to find activities that suit your needs and that will strengthen your bones.
Sometimes a compression fracture, when bones in the spine collapse, can produce pain. Physiotherapy can help to manage this pain.
Osteoporosis is more common in older people and is often the reason why they fall. Falling is a common problem for people aged 65 and over. If you are at risk of falling, a physio can help you improve your balance.
Weight-bearing exercise, such as walking or dancing, can help to strengthen your bones. Weight-bearing exercise is any exercise in which you are supporting your own body weight through your feet and legs (or arms and hands).
Weight-bearing exercises, such as walking, can help to strengthen bones strengthening exercises, using weights or resistance bands, have also been shown to maintain or improve bone density at the location of the targeted muscle attachments. Maintaining bone health in this population is extremely important, especially in the elderly as there is typically a decline in bone mass with age.
- Brisk walking
- Climbing stairs
- Dancing
- Hiking
- Jogging
- Jumping rope
- Step aerobics
- Tennis or other racquet sports
- Yard work, like pushing a lawnmower or heavy gardening
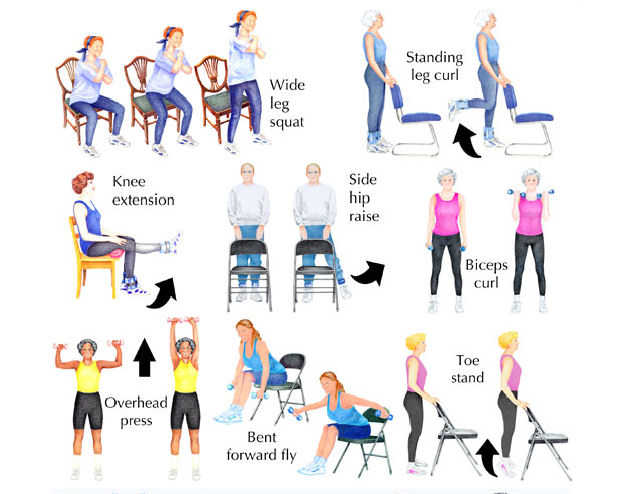
Exercises to improve your balance and strength will help to prevent falls, balance exercises are also important to incorporate to further reduce the risk of falls.
Postural exercises
These are crucial to prevent structural changes that often accompany osteoporosis, such as thoracic kyphosis. Every osteoporosis program should include extension exercises;
- Chin tucks
- Scapular retractions
- Thoracic extensions
- Hip extensions
- Strengthening the extensor muscles will promote improved posture and improved balance.
Flexion exercises are CONTRAINDICATED. Anterior compressive forces on the vertebra can contribute to compression fractures.
Follow a healthy diet that includes enough calcium and Vitamin D
Use this handy calcium calculator to make sure you are getting enough calcium.
Wear sensible, well-fitting shoes to avoid falls
Avoid rugs and sloppy slippers – both can cause trips
Have good lighting on your stairs
Get your eyesight checked regularly (free for people over 60)
Try to avoid heavy lifting – consider home delivery grocery shopping
Hydrotherapy (gentle exercise in warm water), was received by several of those we interviewed with spinal fractures to help relax their muscles.
FAQ
What is the main cause of osteoporosis?
A diet poor in calcium and vitamin D can raise your risk of osteoporosis and fractures starting in childhood and continuing into old age. Your risk of osteoporosis and bone loss may rise if you overeat or consume insufficient amounts of protein.
What happens if you have osteoporosis?
Because of osteoporosis, bones become weak and brittle, easily breaking from simple stressors like bending over or coughing. The hip, wrist, or spine are the most frequently broken bones associated with osteoporosis. Living tissue, such as bone, is continually being replenished and broken down.
Is osteoporosis is Cured?
Osteoporosis cannot be cured, but its symptoms can be controlled with medication and lifestyle modifications. Your doctor will suggest several treatments to aid you based on your age, sex, and medical history. Strengthening your bones to make them less prone to breaking is the goal of treatment.
What are the 5 stages of osteoporosis?
The four stages of osteoporosis are as follows. As the illness worsens, an individual’s bones get weaker over time until they start to have fractures. It is rare for someone to experience any symptoms in the early stages of osteoporosis. It’s also possible that they won’t become aware of their illness until they suffer a bone break.
Is walking good for osteoporosis?
Walking, dancing, low-impact aerobics, using an elliptical trainer, climbing stairs, and gardening are a few examples. To decrease bone loss, these exercises target the lower spine, hips, and legs directly. They benefit the heart and increase blood flow as well.
Which organ is most affected by osteoporosis?
The illness known as osteoporosis results in weak, thinning bones. The likelihood of the bones shattering increases as a result. The hips, spine, and wrists are the bones most frequently impacted. Men are four times less likely than women to develop osteoporosis due to a drop in estrogen following menopause.




52 Comments